Korean J Lab Med.
2010 Apr;30(2):153-159. 10.3343/kjlm.2010.30.2.153.
Evaluation of the Clinical Performance of an Automated Procalcitonin Assay for the Quantitative Detection of Bloodstream Infection
- Affiliations
-
- 1Department of Laboratory Medicine, Dong-A University College of Medicine, Busan, Korea. jyhan@dau.ac.kr
- KMID: 1096801
- DOI: http://doi.org/10.3343/kjlm.2010.30.2.153
Abstract
- BACKGROUND
Bloodstream infection (BSI) is associated with a high mortality rate. Since the origin of infection is demonstrated in approximately 2/3rds of cases, early and established biomarkers are warranted. We evaluated the clinical performances of automated procalcitonin (PCT) and C-reactive protein (CRP) assays for the quantitative detection of BSI. Analytical performance of the VIDAS(R) B.R.A.H.M.S PCT assay (bioMerieux, France) was assessed and also compared with the semi-quantitative PCT-Q test (B.R.A.H.M.S Aktiengesellschaft, Germany).
METHODS
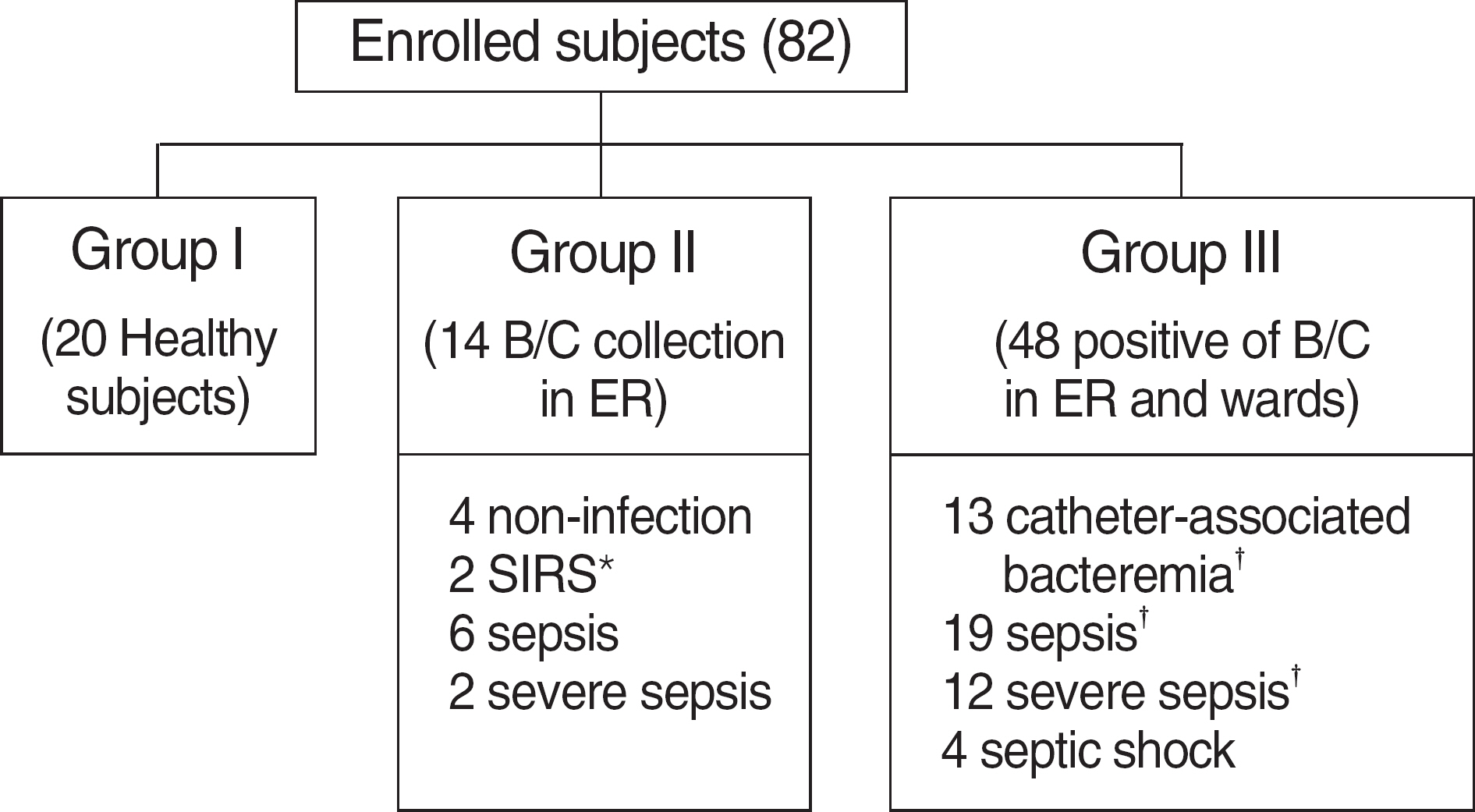
We prospectively included consecutive patients divided into 3 groups at the Dong-A University Medical Center. Patients were categorized according to the criteria of the American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference (ACCP/SCCM), and also on the basis of catheter-associated bacteremia.
RESULTS
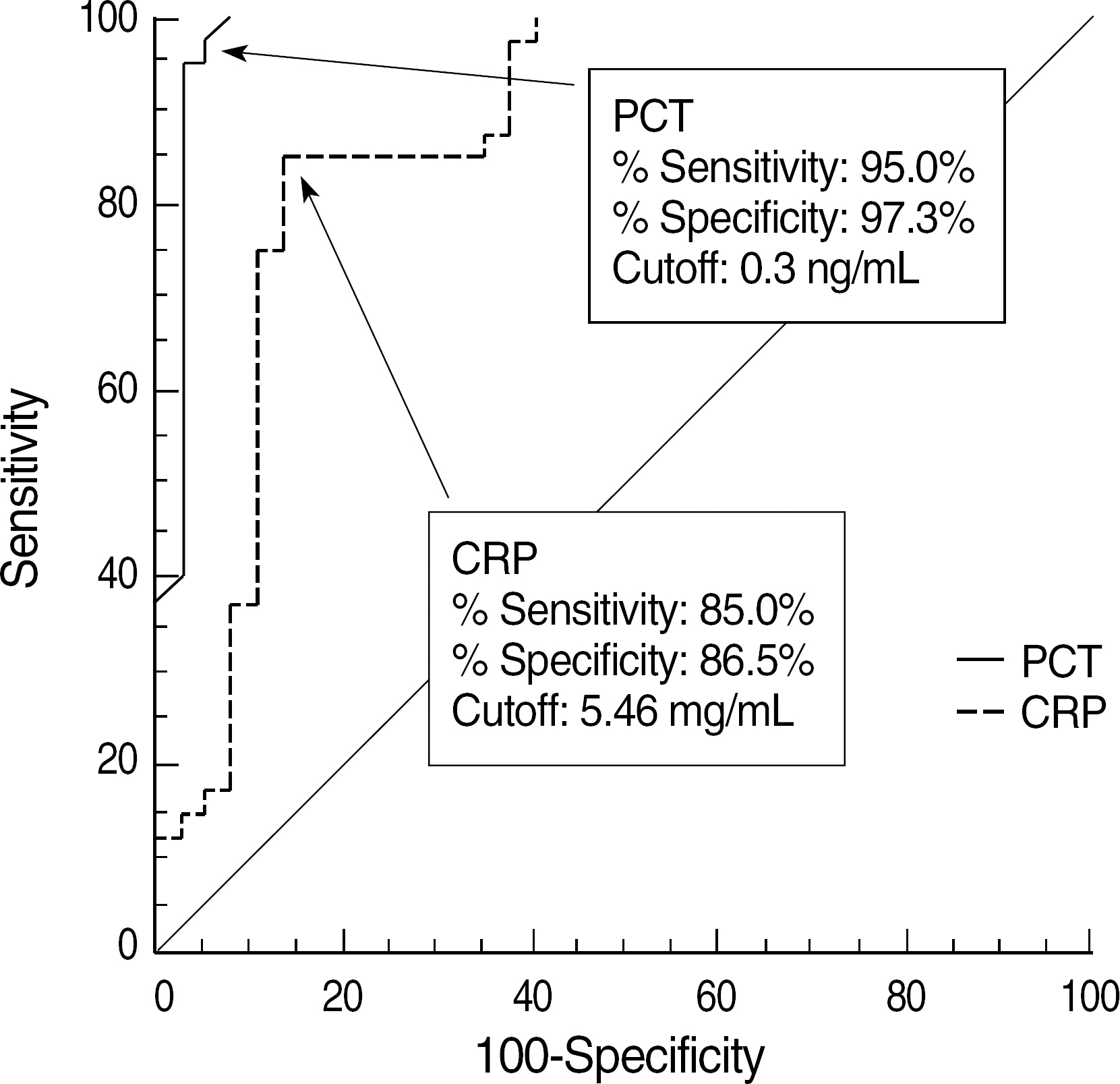
A total 77 patients were enrolled. All mean values of PCT and PCT-Q were consistent with the reference value. Measured PCT concentrations showed good linearity (r=0.983). The between-run, within-run, and total imprecisions were below 5%. The PCT levels in gram-negative bacteremia were significantly higher than those in gram-positive bacteremia. Furthermore, the PCT concentrations were significantly different among non-infection, bacteremia, sepsis, severe sepsis, and septic shock groups. Our study showed that PCT >0.3 ng/mL had 95.0% sensitivity and 97.3% specificity, whereas CRP >5.46 mg/dL had 85.0% sensitivity and 86.5% specificity for diagnosing sepsis.
CONCLUSIONS
We suggest that, compared with CRP, PCT is a better diagnostic and discriminative biomarker of sepsis categorized according to the ACCP/SCCM. Moreover, catheter-associated bacteremia could be discriminated from sepsis using PCT concentration.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Performance Evaluation of the ichroma SMART Analyzer in Measuring C-reactive Protein and Procalcitonin Levels
John Hoon Rim, Hyo-Jun Ahn, Kwang Kuk Yoon, Hye Ryun Kim, Young-Ah Kim, Hwan Sub Lim, Jongha Yoo
Lab Med Online. 2016;6(1):19-24. doi: 10.3343/lmo.2016.6.1.19.Clinical Value of Procalcitonin in Patients with Spinal Infection
Deok-Ki Jeong, Hyun-Woo Lee, Young-Min Kwon
J Korean Neurosurg Soc. 2015;58(3):271-275. doi: 10.3340/jkns.2015.58.3.271.
Reference
-
1.Mylotte JM., Kahler L., McCann C. Community-acquired bacteremia at a teaching versus a nonteaching hospital: impact of acute severity of illness on 30-day mortality. Am J Infect Control. 2001. 29:13–9.
Article2.Weinstein MP., Towns ML., Quartey SM., Mirrett S., Reimer LG., Parmigiani G, et al. The clinical significance of positive blood cultures in the 1990s: a prospective comprehensive evaluation of the microbiology, epidemiology, and outcome of bacteremia and fungemia in adults. Clin Infect Dis. 1997. 24:584–602.
Article3.Munson EL., Diekema DJ., Beekmann SE., Chapin KC., Doern GV. Detection and treatment of bloodstream infection: laboratory reporting and antimicrobial management. J Clin Microbiol. 2003. 41:495–7.
Article4.Khatib R., Saeed S., Sharma M., Riederer K., Fakih MG., Johnson LB. Impact of initial antibiotic choice and delayed appropriate treatment on the outcome of Staphylococcus aureus bacteremia. Eur J Clin Microbiol Infect Dis. 2006. 25:181–5.
Article5.Angus DC., Linde-Zwirble WT., Lidicker J., Clermont G., Carcillo J., Pinsky MR. Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med. 2001. 29:1303–10.
Article6.Sudhoff T., Giagounidis A., Karthaus M. Serum and plasma parameters in clinical evaluation of neutropenic fever. Antibiot Chemother. 2000. 50:10–9.7.Assicot M., Gendrel D., Carsin H., Raymond J., Guilbaud J., Bohuon C. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet. 1993. 341:515–8.
Article8.American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med. 1992. 20:864–74.9.Muller B., Becker KL. Procalcitonin: how a hormone became a marker and mediator of sepsis. Swiss Med Wkly. 2001. 131:595–602.10.Clinical and Laboratory Standards Institute. Evaluation of the linearity of quantitative measurement procedures: a statistical approach: approved guideline. Document EP6-A. Wayne, PA: Clinical and Laboratory Standards Institute;2003.11.Clinical and Laboratory Standards Institute. Evaluation of precision performance of quantitative measurement methods: approved guideline. Document EP5-A2. 2nd ed.Wayne, PA: Clinical and Laboratory Standards Institute;2004.12.Schuetz P., Christ-Crain M., Huber AR., Muller B. Long-term stability of procalcitonin in frozen samples and comparison of Kryptor and VIDAS automated immunoassays. Clin Biochem. 2010. 43:341–4.
Article13.Jongwutiwes U., Suitharak K., Tiengrim S., Thamlikitkul V. Serum procalcitonin in diagnosis of bacteremia. J Med Assoc Thai. 2009. ;92 (Suppl 2):S. 79–87.14.Levy MM., Fink MP., Marshall JC., Abraham E., Angus D., Cook D, et al. 2001 SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Crit Care Med. 2003. 31:1250–6.
Article15.Brunkhorst FM., Wegscheider K., Forycki ZF., Brunkhorst R. Procalcitonin for early diagnosis and differentiation of SIRS, sepsis, severe sepsis, and septic shock. Intensive Care Med. 2000. 26(Suppl 2):148–52.
Article16.Al-Nawas B., Krammer I., Shah PM. Procalcitonin in diagnosis of severe infections. Eur J Med Res. 1996. 1:331–3.17.Simon L., Gauvin F., Amre DK., Saint-Louis P., Lacroix J. Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis. 2004. 39:206–17.
Article18.Uzzan B., Cohen R., Nicolas P., Cucherat M., Perret GY. Procalcitonin as a diagnostic test for sepsis in critically ill adults and after surgery or trauma: a systematic review and meta-analysis. Crit Care Med. 2006. 34:1996–2003.
Article19.Nakamura A., Wada H., Ikejiri M., Hatada T., Sakurai H., Matsushima Y, et al. Efficacy of procalcitonin in the early diagnosis of bacterial infections in a critical care unit. Shock. 2009. 31:586–91.
Article20.Catton JA., Dobbins BM., Kite P., Wood JM., Eastwood K., Sugden S, et al. In situ diagnosis of intravascular catheter-related bloodstream infection: a comparison of quantitative culture, differential time to positivity, and endoluminal brushing. Crit Care Med. 2005. 33:787–91.
Article21.Charles PE., Ladoire S., Aho S., Quenot JP., Doise JM., Prin S, et al. Serum procalcitonin elevation in critically ill patients at the onset of bacteremia caused by either Gram negative or Gram positive bacteria. BMC Infect Dis. 2008. 8:38.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Performance Evaluation of the Automated Fluorescent Immunoassay System Rotavirus Assay in Clinical Samples
- Performance Evaluation of the ELITe InGenius System for Detecting Cytomegalovirus, EpsteinBarr Virus, and BK Virus Infections
- Performance Evaluation of a New Automated Chemiluminescent Immunoanalyzer-Based Interferon-Gamma Releasing Assay AdvanSure I3 in Comparison With the QuantiFERON-TB Gold In-Tube Assay
- Development of One-step Real-time Reverse Transcription-polymerase Chain Reaction in Combination with Automated RNA Extraction for Detection and Quantitation of Hepatitis A Virus
- Recommendations for the Verification of Quantitative Molecular Hemato-Oncology Tests