J Korean Med Sci.
2005 Apr;20(2):316-318. 10.3346/jkms.2005.20.2.316.
Preoperative Embolization in Surgical Treatment of a Primary Hemangiopericytoma of the Rib: A Case Report
- Affiliations
-
- 1Department of Pulmonary Medicine, Faculty of Medicine Ondokuz Mayis University, Samsun, Turkey. serhatf@omu.edu.tr
- 2Department of Radiology, Faculty of Medicine Ondokuz Mayis University, Samsun, Turkey.
- 3Department of Pathology, Faculty of Medicine Ondokuz Mayis University, Samsun, Turkey.
- KMID: 1095211
- DOI: http://doi.org/10.3346/jkms.2005.20.2.316
Abstract
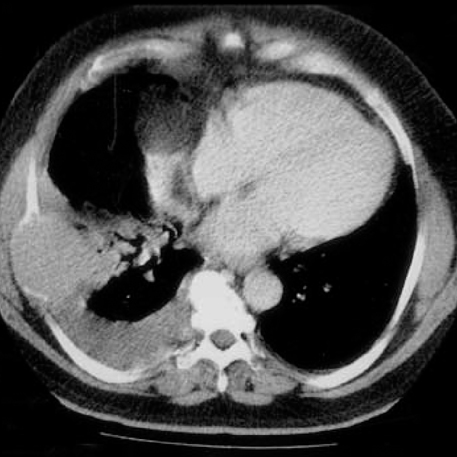
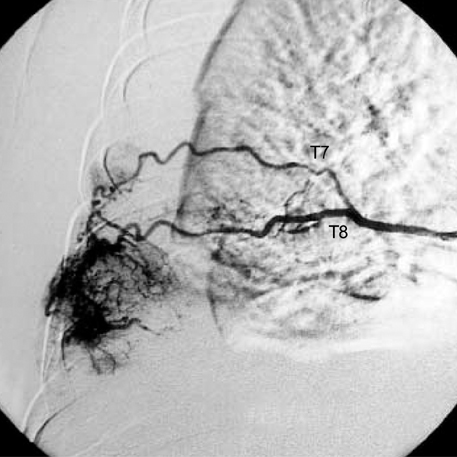
- Primary hemangiopericytoma of the rib is extremely rare and only a few cases have been reported. A 62-yr-old man presented with an aching chest pain and dyspnea. Thoracic computed tomography revealed a homogenous mass expanding the right seventh rib. A diagnosis of hemangiopericytoma was established by percutaneous needle biopsy. Preoperative embolization of the feeding vessels of the tumor was performed in order to prevent perioperative bleeding. There was no significant bleeding during the surgery, where complete resection of the tumor with 7th to 9th ribs with a surgical margin of 5 cm was performed. Postoperative course was uneventful and there has been no recurrence for thirteen months. To our knowledge, there has been no report to apply a preoperative embolization of a primary hemangiopericytoma of the rib.
MeSH Terms
Figure
Reference
-
1. Enzinger FM, Smith BH. Hemangiopericytoma. An analysis of 106 cases. Hum Pathol. 1976. 7:61–82.2. Collet P, Loire R, Guerin JC, Brune J. Hemangiopericytomes thoraciques apparemment primitifs. Rev Pneumol Clin. 1985. 41:151–154.3. Craven JP, Quigley TM, Bolen JW, Raker EJ. Current management and clinical outcome of hemangiopericytomas. Am J Surg. 1992. 163:490–493.
Article4. Morandi U, Stefani A, De Santis M, Paci M, Lodi R. Preoperative embolization in surgical treatment of mediastinal hemangiopericytoma. Ann Thorac Surg. 2000. 69:937–939.
Article5. Yanagihara K, Ueno Y, Isobe J, Yoshimi N, Itoh M. Hemangiopericytoma of the chest wall. Ann Thorac Surg. 1997. 63:537–539.6. Fraser RS, Müller NL, Colman N, Pare PD. Diagnosis of Diseases of the Chest. 1999. 4th ed. Philadelphia: W.B. Saunders Company.7. Biagi G, Gotti G, Bisceglie M, Lorenzini L, Toscano M, Sforza V. Uncommon intrathoracic extrapulmonary tumor: primary hemangiopericytoma. Ann Thorac Surg. 1990. 49:998–999.
Article8. Wick MR, Swanson PE, Manivel JC. Immunohistochemical analysis of soft tissue sarcomas. Comparisons with electron microscopy. Appl Pathol. 1988. 6:169–196.9. Feldman F, Seaman WB. Primary thoracic hemangiopericytoma. Radiology. 1964. 182:998–1009.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Primary hemongiopericytoma of the lung
- A case of successfully resected retroperitoneal hemangiopericytoma
- Intracranial Hemorrhage as a Complication of Preoperative Embolization for Brain Tumor: Report of Two Cases
- Primary Malignant Hemangiopericytoma of the Lung: A case report
- Malignant Prostatic Hemangiopericytoma