J Korean Med Sci.
2011 Jul;26(7):962-965. 10.3346/jkms.2011.26.7.962.
A Case of Atypical Skull Base Osteomyelitis with Septic Pulmonary Embolism
- Affiliations
-
- 1Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea. docra@docra.pe.kr
- 2Department of Radiology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 3Department of Pathology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- 4Department of Neurology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea.
- KMID: 1094272
- DOI: http://doi.org/10.3346/jkms.2011.26.7.962
Abstract
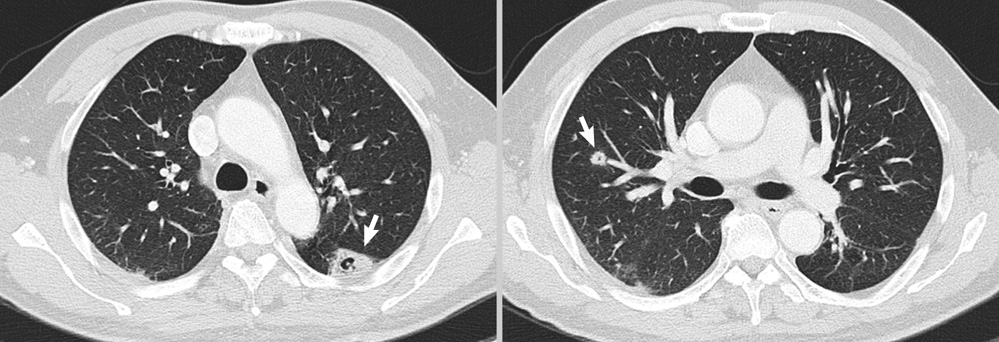
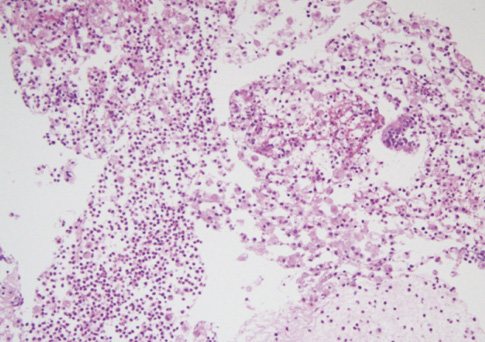
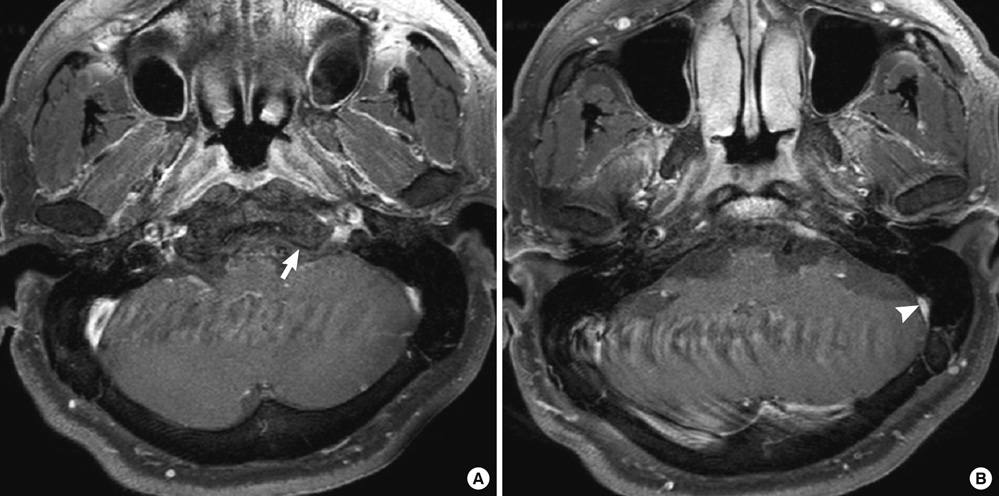
- Skull base osteomyelitis (SBO) is difficult to diagnose when a patient presents with multiple cranial nerve palsies but no obvious infectious focus. There is no report about SBO with septic pulmonary embolism. A 51-yr-old man presented to our hospital with headache, hoarseness, dysphagia, frequent choking, fever, cough, and sputum production. He was diagnosed of having masked mastoiditis complicated by SBO with multiple cranial nerve palsies, sigmoid sinus thrombosis, and septic pulmonary embolism. We successfully treated him with antibiotics and anticoagulants alone, with no surgical intervention. His neurologic deficits were completely recovered. Decrease of pulmonary nodules and thrombus in the sinus was evident on the follow-up imaging one month later. In selected cases of intracranial complications of SBO and septic pulmonary embolism, secondary to mastoiditis with early response to antibiotic therapy, conservative treatment may be considered and surgical intervention may be withheld.
MeSH Terms
-
Anti-Bacterial Agents/therapeutic use
Anticoagulants/therapeutic use
C-Reactive Protein/analysis
Cranial Nerve Diseases/complications/diagnosis
Diagnosis, Differential
Enterobacter aerogenes/isolation & purification
Enterobacteriaceae Infections/diagnosis/drug therapy
Humans
Lung/pathology/radiography
Magnetic Resonance Imaging
Male
Mastoiditis/complications/diagnosis
Middle Aged
Osteomyelitis/complications/*diagnosis/drug therapy
Pulmonary Embolism/complications/*diagnosis/microbiology
Sinus Thrombosis, Intracranial/complications/diagnosis
Skull Base
Sputum/microbiology
Tomography, X-Ray Computed
Figure
Reference
-
1. Grobman LR, Ganz W, Casiano R, Goldberg S. Atypical osteomyelitis of the skull base. Laryngoscope. 1989. 99:671–676.2. Chandler JR, Grobman L, Quencer R, Serafini A. Osteomyelitis of the base of the skull. Laryngoscope. 1986. 96:245–251.3. Go C, Bernstein JM, de Jong AL, Sulek M, Friedman EM. Intracranial complications of acute mastoiditis. Int J Pediatr Otorhinolaryngol. 2000. 52:143–148.4. Holt GR, Gates GA. Masked mastoiditis. Laryngoscope. 1983. 93:1034–1037.5. Hoshino C, Satoh N, Sugawara S, Kuriyama C, Kikuchi A, Ohta M. Septic cavernous sinus thrombosis complicated by narrowing of the internal carotid artery, subarachnoid abscess and multiple pulmonary septic emboli. Intern Med. 2007. 46:317–323.6. Lepage AA, Hess EP, Schears RM. Septic thrombophlebitis with acute osteomyelitis in adolescent children: a report of two cases and review of the literature. Int J Emerg Med. 2008. 1:155–159.7. Sibai TA, Ben-Galim PJ, Eicher SA, Reitman CA. Infectious Collet-Sicard syndrome in the differential diagnosis of cerebrovascular accident: a case of head-to-neck dissociation with skull-based osteomyelitis. Spine J. 2009. 9:e6–e10.8. Bhatia K, Jones NS. Septic cavernous sinus thrombosis secondary to sinusitis: are anticoagulants indicated? A review of the literature. J Laryngol Otol. 2002. 116:667–676.