Korean J Radiol.
2009 Apr;10(2):135-143. 10.3348/kjr.2009.10.2.135.
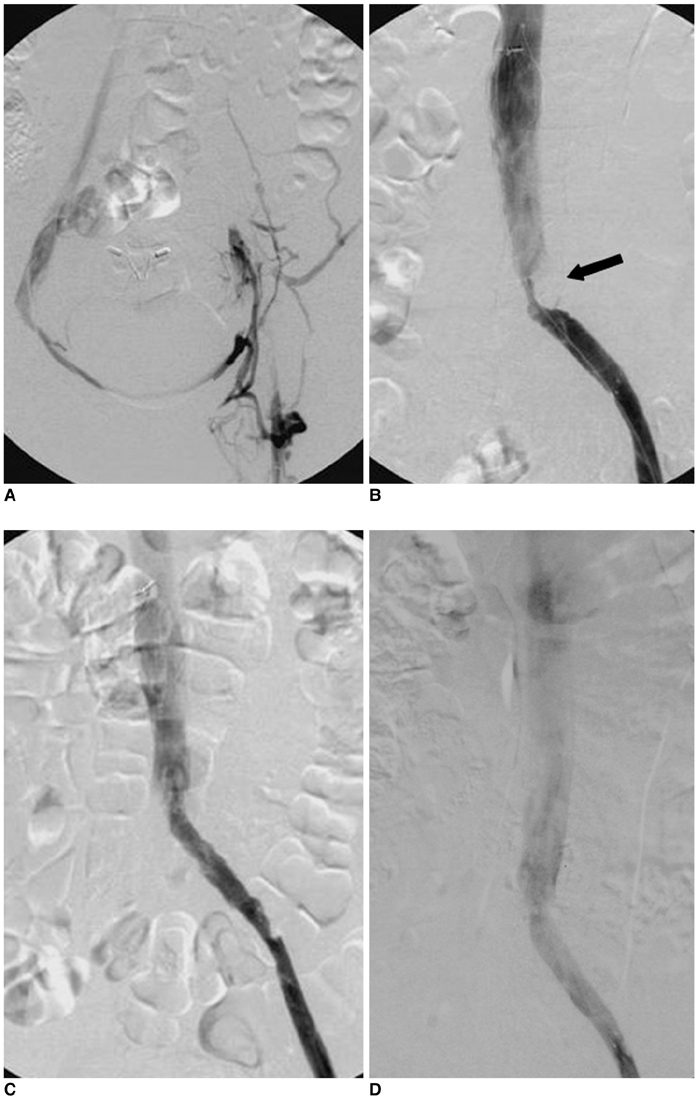
Endovascular Treatment for Iliac Vein Compression Syndrome: a Comparison between the Presence and Absence of Secondary Thrombosis
- Affiliations
-
- 1Department of Interventional Radiology, Nanjing First Hospital, China. (Affiliated to Nanjing Medical University). cjr.gujianping@vip.163.com
- KMID: 1088724
- DOI: http://doi.org/10.3348/kjr.2009.10.2.135
Abstract
OBJECTIVE
To evaluate the value of early identification and endovascular treatment of iliac vein compression syndrome (IVCS), with or without deep vein thrombosis (DVT).
MATERIALS AND METHODS
Three groups of patients, IVCS without DVT (group 1, n = 39), IVCS with fresh thrombosis (group 2, n = 52) and IVCS with non-fresh thrombosis (group 3, n = 34) were detected by Doppler ultrasonography, magnetic resonance venography, computed tomography or venography. The fresh venous thrombosis were treated by aspiration and thrombectomy, whereas the iliac vein compression per se were treated with a self-expandable stent. In cases with fresh thrombus, the inferior vena cava filter was inserted before the thrombosis suction, mechanical thrombus ablation, percutaneous transluminal angioplasty, stenting or transcatheter thrombolysis.
RESULTS
Stenting was performed in 111 patients (38 of 39 group 1 patients and 73 of 86 group 2 or 3 patients). The stenting was tried in one of group 1 and in three of group 2 or 3 patients only to fail. The initial patency rates were 95% (group 1), 89% (group 2) and 65% (group 3), respectively and were significantly different (p = 0.001). Further, the six month patency rates were 93% (group 1), 83% (group 2) and 50% (group 3), respectively, and were similarly significantly different (p = 0.001). Both the initial and six month patency rates in the IVCS patients (without thrombosis or with fresh thrombosis), were significantly greater than the patency rates of IVCS patients with non-fresh thrombosis.
CONCLUSION
From the cases examined, the study suggests that endovascular treatment of IVCS, with or without thrombosis, is effective.
MeSH Terms
-
Adolescent
Adult
Aged
*Angioplasty, Balloon
*Balloon Dilatation
Constriction, Pathologic/therapy
Diagnostic Imaging
Female
Humans
Iliac Vein/*pathology/surgery
Male
Middle Aged
Peripheral Vascular Diseases/complications/diagnosis/*therapy
Retrospective Studies
*Stents
Thrombectomy
Vascular Patency
Vena Cava Filters
Venous Thrombosis/complications/diagnosis/*therapy
Figure
Cited by 1 articles
-
Self-Expandable Stents in Vascular Stenosis of Moderate to Large-Sized Vessels in Congenital Heart Disease: Early and Intermediate-Term Results
Gi Young Jang, Kee Soo Ha
Korean Circ J. 2019;49(10):932-942. doi: 10.4070/kcj.2019.0067.
Reference
-
1. O'Sullivan GJ, Semba CP, Bittner CA, Kee ST, Razavi MK, Sze DY, et al. Endovascular management of iliac vein compression (May-Thurner) syndrome. J Vasc Interv Radiol. 2000. 11:823–836.2. Patel NH, Stookey KR, Ketcham DB, Cragg AH. Endovascular management of acute extensive iliofemoral deep venous thrombosis caused by May-Thurner syndrome. J Vasc Interv Radiol. 2000. 11:1297–1302.3. Bulger CM, Jacobs C, Patel NH. Epidemiology of acute deep vein thrombosis. Tech Vasc Interv Radiol. 2004. 7:50–54.4. Juhan C, Miltgen G, Barthélémy P, Ayuso D. Treatment of iliofemoral venous thromboses with surgical thrombectomy. Bull Acad Natl Med. 1991. 175:643–649.5. Plate G, Eklöf B, Norgren L, Ohlin P, Dahlström JA. Venous thrombectomy for iliofemoral vein thrombosis-10-year results of a prospective randomized study. Eur J Vasc Endovasc Surg. 1997. 14:367–374.6. Grossman C, McPherson S. Safety and efficacy of catheter-directed thrombolysis for iliofemoral venous thrombosis. AJR Am J Roentgenol. 1999. 172:667–672.7. Mewissen MW, Seabrook GR, Meissner MH, Cynamon J, Labropoulos N, Haughton SH. Caterter-directed thrombolysis for lower extremity deep venous thrombosis: report of a national multicenter registry. Radiology. 1999. 211:39–49.8. Kibbe MR, Ujiki M, Goodwin AL, Eskandari M, Yao J, Matsumura J. Iliac vein compression in an asymptomatic patient population. J Vasc Surg. 2004. 39:937–943.9. Raju S, Neglen P. High prevalence of nonthrombotic iliac vein lesions in chronic venous disease: a permissive role in pathogenicity. J Vasc Surg. 2006. 44:136–144.10. Sharafuddin MJ, Gu X, Han YM, Urness M, Gunther R, Amplatz K. Injury potential to venous valves from the Amplatz thrombectomy device. J Vasc Interv Radiol. 1999. 10:64–69.11. Delomez M, Beregi JP, Willoteaux S, Bauchart JJ, Janne d'Othée B, Asseman P, et al. Mechanical thrombectomy in patients with deep venous thrombosis. Cardiovasc Intervent Radiol. 2001. 24:42–48.12. Vedantham S, Vesely TM, Parti N, Darcy M, Hovsepian DM, Picus D. Lower extremity venous thrombolysis with adjunctive mechanical thrombectomy. J Vasc Interv Radiol. 2002. 13:1001–1008.13. Frisoli JK, Sze D. Mechanical thrombectomy for the treatment of lower extremity deep vein thrombosis. Tech Vasc Interv Radiol. 2003. 6:49–52.14. Sharafuddin MJ, Sun S, Hoballah JJ, Youness FM, Sharp WJ, Roh BS. Endovascular management of venous thrombotic and occlusive disease of the lower extremities. J Vasc Interv Radiol. 2003. 14:405–423.15. Decousus H, Leizorovicz A, Parent F, Page Y, Tardy B, Girard P, et al. A clinical trial of vena caval filters in the prevention of pulmonary embolism in patients with proximal deep-vein thrombosis. N Engl J Med. 1998. 338:409–415.16. Yamagami T, Kato T, Iida S, Hirota T, Nishimura T. Gunther tulip inferior vena cava filter placement for deep venous thrombosis of the lower extremity. Cardiovasc Intervent Radiol. 2005. 28:442–453.17. Rosenthal D, Wellons ED, Lai KM, Bikk A, Henderson VJ. Retrievable inferior vena cava filters: initial clinical results. Ann Vasc Surg. 2006. 20:157–165.18. Kalva SP, Wicky S, Waltman AC, Athanasoulis CA. TrapEase vena cava filter: experience in 751 patients. J Endovasc Ther. 2006. 13:365–372.19. Kim JY, Choi D, Guk Ko Y, Park S, Jang Y, Lee do Y. Percutaneous treatment of deep vein thrombosis in May-Thurner syndrome. Cardiovasc Intervent Radiol. 2006. 4:571–575.20. Kwak HS, Han YM, Lee YS, Jin GY, Chung GH. Stents in common iliac vein obstruction with acute ipsilateral deep venous thrombosis: early and late results. J Vasc Interv Radiol. 2005. 16:815–822.21. Blum A, Roche E. Endovascular management of acute deep vein thrombosis. Am J Med. 2005. 118:31S–36S.22. Liang HL, Pan HB, Lin YH, Chen CY, Chung HM, Wu TH, et al. Metallic stent placement in hemodialysis graft patients after insufficient balloon dilation. Korean J Radiol. 2006. 7:118–124.23. Cho SK, Do YS, Shin SW, Park KB, Kim DI, Kim YW, et al. Subintimal angioplasty in the treatment of chronic lower limb ischemia. Korean J Radiol. 2006. 7:131–138.24. Delis KT, Bountouroglou D, Mansfield AO. Venous claudication in iliofemoral thrombosis: long-term effects on venous hemodynamics, clinical status, and quality of life. Ann Surg. 2004. 239:118–126.25. Neglen P, Thrasher TL, Raju S. Venous outflow obstruction: an underestimated contributor to chronic venous disease. J Vasc Surg. 2003. 38:879–885.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Left Iliac Vein Thrombosis with May-Thurner Syndrome
- Endovascular Management of Iliac Vein Compression Syndrome Associated with Thrombosis
- May-Thurner Syndrome with Coexisting Arteriovenous Fistula Treated Using an Endovascular Procedure
- Iliac Vein Compression Syndrome: 4 Case
- May-Thurner Syndrome Treated with Endovascular Wall Stent