Korean J Ophthalmol.
2011 Aug;25(4):294-297. 10.3341/kjo.2011.25.4.294.
A Congruous Superior Quadrantanopsia Following a Junctional Scotoma Induced by Asperogillosis
- Affiliations
-
- 1Department of Ophthalmology, Kyung Hee University School of Medicine, Seoul, Korea.
- 2Department of Ophthalmology, Chung-Ang University Hospital, Chung-Ang University College of Medicine, Seoul, Korea. yschun100@hanmail.net
- KMID: 1018422
- DOI: http://doi.org/10.3341/kjo.2011.25.4.294
Abstract
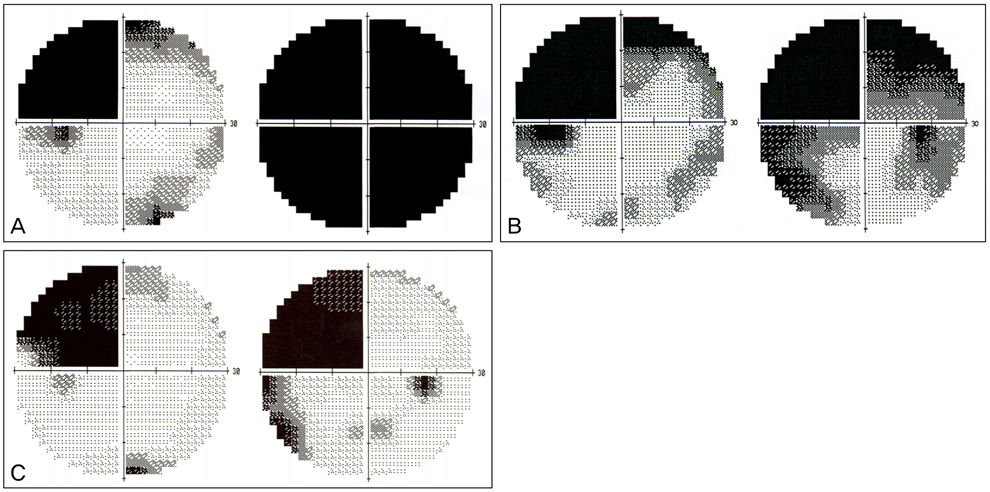
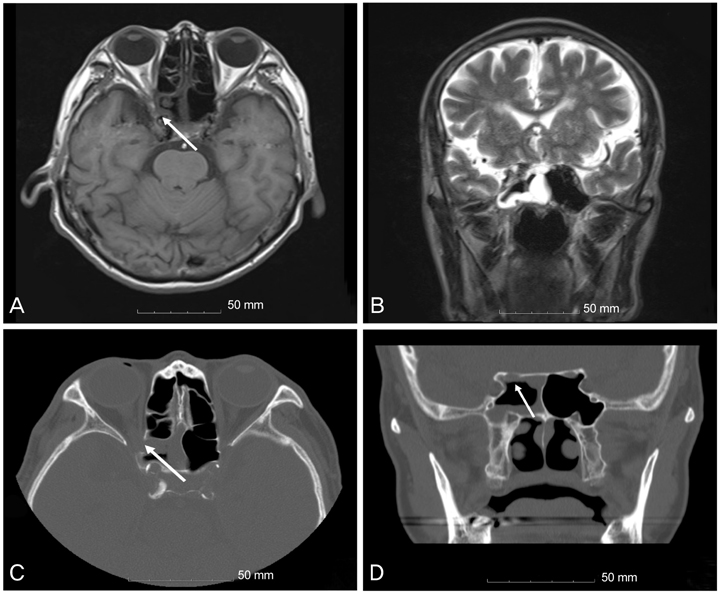
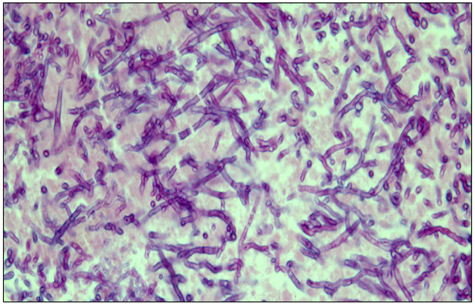
- A 69-year old man presented to us with decreased vision in his right eye and a relative afferent pupillary defect. Under the presumption that he was suffering from retrobulbar optic neuritis or ischemic optic neuropathy, visual field tests were performed, revealing the presence of a junctional scotoma. Imaging studies revealed tumorous lesions extending from the sphenoid sinus at the right superior orbital fissure, with erosion of the right medial orbital wall and optic canal. Right optic nerve decompression was performed via an endoscopic sphenoidectomy, and histopathologic examination confirmed the presence of aspergillosis. The patient did not receive any postoperative antifungal treatment; however, his vision improved to 20 / 40, and his visual field developed a left congruous superior quadrantanopsia 18 months postoperatively. A junctional scotoma can be caused by aspergillosis, demonstrating the importance of examining the asymptomatic eye when a patient is experiencing a loss of vision in one eye. Furthermore, damage to the distal optic nerve adjacent to the proximal optic chiasm can induce unusual congruous superior quadrantanopsia.
Keyword
MeSH Terms
-
Aged
Antifungal Agents/therapeutic use
Aspergillosis/*complications/diagnosis
Decompression, Surgical/methods
Diagnosis, Differential
Endoscopy/methods
Eye Infections, Fungal/*complications/diagnosis/therapy
Follow-Up Studies
Hemianopsia/*complications/diagnosis/therapy
Humans
Magnetic Resonance Imaging
Male
Optic Nerve/pathology
Scotoma/diagnosis/*etiology/therapy
Sphenoid Bone/surgery
Visual Acuity
Visual Fields
Figure
Reference
-
1. Brown P, Demaerel P, McNaught A, et al. Neuro-ophthalmological presentation of non-invasive Aspergillus sinus disease in the non-immunocompromised host. J Neurol Neurosurg Psychiatry. 1994. 57:234–237.2. Hora JF. Primary aspergillosis of the paranasal sinuses and associated areas. Laryngoscope. 1965. 75:768–773.3. Hedges TR, Leung LS. Parasellar and orbital apex syndrome caused by aspergillosis. Neurology. 1976. 26:117–120.4. Pieroth L, Winterkorn JM, Schubert H, et al. Concurrent sinoorbital aspergillosis and cerebral nocardiosis. J Neuroophthalmol. 2004. 24:135–137.5. Weinstein JM, Sattler FA, Towfighi J, et al. Optic neuropathy and paratrigeminal syndrome due to Aspergillus fumigatus. Arch Neurol. 1982. 39:582–585.6. Nielsen EW, Weisman RA, Savino PJ, Schatz NJ. Aspergillosis of the sphenoid sinus presenting as orbital pseudotumor. Otolaryngol Head Neck Surg. 1983. 91:699–703.7. O'Toole L, Acheson JA, Kidd D. Orbital apex lesion due to Aspergillosis presenting in immunocompetent patients without apparent sinus disease. J Neurol. 2008. 255:1798–1801.8. Bahadur S, Kacker SK, D'souza B, Chopra P. Paranasal sinus aspergillosis. J Laryngol Otol. 1983. 97:863–867.9. Miller NR, Newman NJ, Hoyt WF, Walsh FB, editors. Walsh and Hoyt's clinical neuro-ophthalmology. 1998. 5th ed. Baltimore: Lipponcott Williams & Wilkins;104–106.10. Kedar S, Zhang X, Lynn MJ, et al. Congruency in homonymous hemianopia. Am J Ophthalmol. 2007. 143:772–780.11. Horton JC. Wilbrand's knee of the primate optic chiasm is an artefact of monocular enucleation. Trans Am Ophthalmol Soc. 1997. 95:579–609.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Ophthalmic Migraine
- Junctional scotoma in giant cerebral aneurysm
- Transient Homonymous Superior Quadrantanopsia in Nonketotic Hyperglycemia: A Case Report and Systematic Review
- Nine Cases of Ethambutol Toxicity on Human Eye
- Junctional Neurulation : A Junction between Primary and Secondary Neural Tubes