Ann Dermatol.
2017 Aug;29(4):454-461. 10.5021/ad.2017.29.4.454.
Morphological Characteristics of Residual Skin Surface Components Collected from the Surface of Facial Skin in Women of Different Age
- Affiliations
-
- 1Lycotec Ltd., Cambridge, United Kingdom. petyaev@lycotec.com
- 2Saratov State Medical University named after V. I. Razumovsky, Institute of Cardiology of the Ministry of Health of the Russian Federation, Saratov, Russian Federation.
- 3DiagNodus Ltd., Cambridge, United Kingdom.
- KMID: 2388944
- DOI: http://doi.org/10.5021/ad.2017.29.4.454
Abstract
- BACKGROUND
Problems of skin aging and its prevention currently attract increasing attention with the growth of human life expectancy. The morphology of the stratum corneum (SC) is well known, but investigation of age-related changes of its structure is difficult in the absence of non-invasive sampling methods. The residual skin surface components (RSSC) that overlay the SC can be easily collected non-invasively.
OBJECTIVE
The aim of this study was to examine morphology of RSSC samples collected from the surface of facial skin of healthy female volunteers of different age.
METHODS
RSSC samples were non-invasively collected from 53 adult female volunteers (22 aged in the range 18∼25 years and 31 aged in the range 50∼73 years). The samples were analysed microscopically.
RESULTS
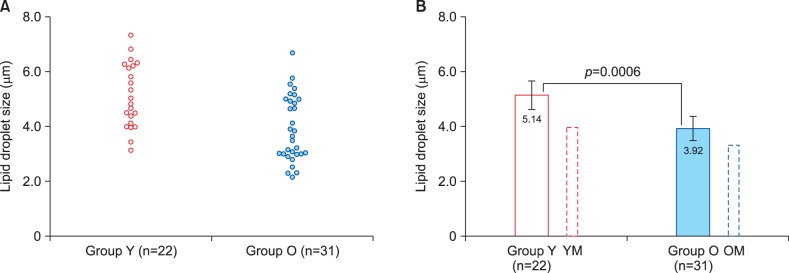
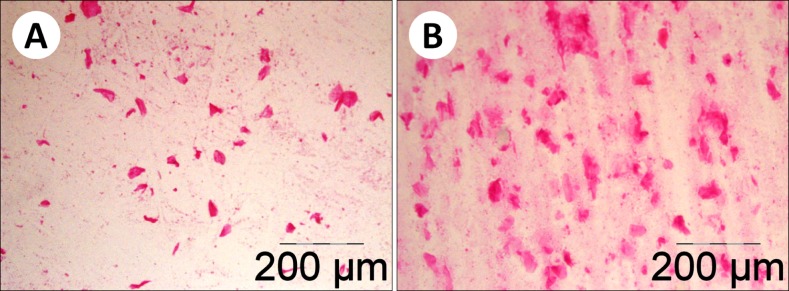
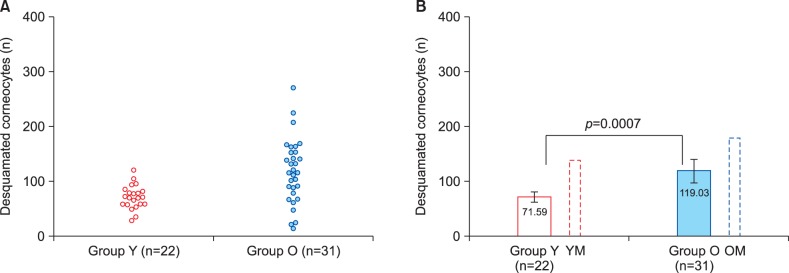
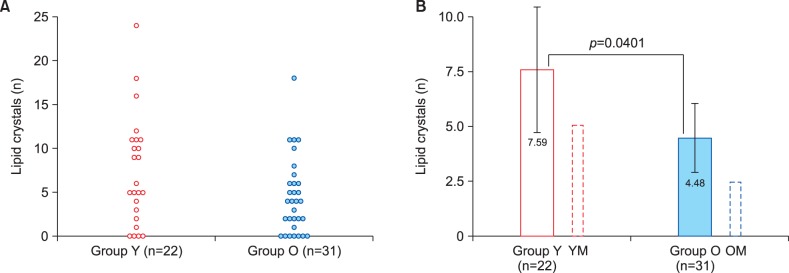
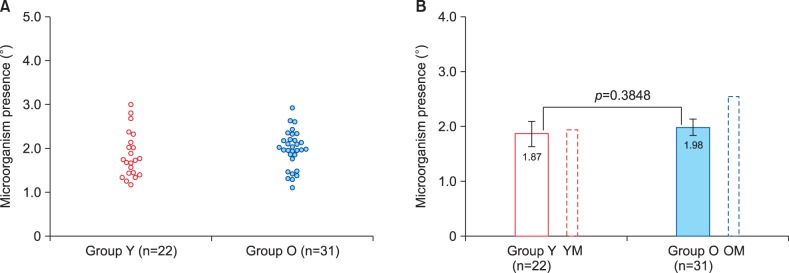
Distinct age-related changes were determined for lipid droplet size, corneocyte desquamation level and lipid crystal count. There was a significant (p=0.0006) decrease in lipid droplet size among older women. Similarly, significantly (p=0.0401) lower lipid crystal numbers were present in the older group. Conversely, corneocyte desquamation was significantly higher (p=0.0007) in older women. No age-related difference in microbial presence in the RSSC could be detected. Result patterns were generally similar to those previously found in male volunteers; however gender-related differences in the absolute values were revealed.
CONCLUSION
Non-invasively collected RSSC samples allow identifying age-related changes on facial skin surface. The results of this study highlight gender-dependence of distinct elements of age-associated impairment of epidermal barrier and can be employed for developing new approaches to prevent changes associated with skin aging.
Keyword
Figure
Reference
-
1. Christensen K, Doblhammer G, Rau R, Vaupel JW. Ageing populations: the challenges ahead. Lancet. 2009; 374:1196–1208. PMID: 19801098.
Article2. Fried LP. Investing in health to create a third demographic dividend. Gerontologist. 2016; 56(Suppl 2):S167–S177. PMID: 26994258.
Article3. Blume-Peytavi U, Kottner J, Sterry W, Hodin MW, Griffiths TW, Watson RE, et al. Age-associated skin conditions and diseases: current perspectives and future options. Gerontologist. 2016; 56(Suppl 2):S230–S242. PMID: 26994263.
Article4. Farage MA, Miller KW, Elsner P, Maibach HI. Characteristics of the aging skin. Adv Wound Care (New Rochelle). 2013; 2:5–10. PMID: 24527317.
Article5. Al-Nuaimi Y, Sherratt MJ, Griffiths CE. Skin health in older age. Maturitas. 2014; 79:256–264. PMID: 25213594.
Article6. Jenkins G. Molecular mechanisms of skin ageing. Mech Ageing Dev. 2002; 123:801–810. PMID: 11869737.
Article7. Vierkötter A, Krutmann J. Environmental influences on skin aging and ethnic-specific manifestations. Dermatoendocrinol. 2012; 4:227–231. PMID: 23467702.
Article8. Kuwazuru O, Miyamoto K, Yoshikawa N, Imayama S. Skin wrinkling morphology changes suddenly in the early 30s. Skin Res Technol. 2012; 18:495–503. PMID: 22233477.
Article9. Stevenson S, Thornton J. Effect of estrogens on skin aging and the potential role of SERMs. Clin Interv Aging. 2007; 2:283–297. PMID: 18044179.10. Emmerson E, Hardman MJ. The role of estrogen deficiency in skin ageing and wound healing. Biogerontology. 2012; 13:3–20. PMID: 21369728.
Article11. Anunciato TP, da Rocha Filho PA. Carotenoids and polyphenols in nutricosmetics, nutraceuticals, and cosmeceuticals. J Cosmet Dermatol. 2012; 11:51–54. PMID: 22360335.
Article12. Jenkins G, Wainwright LJ, Holland R, Barrett KE, Casey J. Wrinkle reduction in post-menopausal women consuming a novel oral supplement: a double-blind placebo-controlled randomized study. Int J Cosmet Sci. 2014; 36:22–31. PMID: 23927381.
Article13. Proksch E, Brandner JM, Jensen JM. The skin: an indispensable barrier. Exp Dermatol. 2008; 17:1063–1072. PMID: 19043850.
Article14. Menon GK, Cleary GW, Lane ME. The structure and function of the stratum corneum. Int J Pharm. 2012; 435:3–9. PMID: 22705878.
Article15. Shetage SS, Traynor MJ, Brown MB, Raji M, Graham-Kalio D, Chilcott RP. Effect of ethnicity, gender and age on the amount and composition of residual skin surface components derived from sebum, sweat and epidermal lipids. Skin Res Technol. 2014; 20:97–107. PMID: 23865719.
Article16. Schmid-Wendtner MH, Korting HC. The pH of the skin surface and its impact on the barrier function. Skin Pharmacol Physiol. 2006; 19:296–302. PMID: 16864974.
Article17. Ali SM, Yosipovitch G. Skin pH: from basic science to basic skin care. Acta Derm Venereol. 2013; 93:261–267. PMID: 23322028.
Article18. Chalyk NE, Bandaletova TY, Kyle NH, Petyaev IM. Age-related differences in morphological characteristics of residual skin surface components collected from the surface of facial skin of healthy male volunteers. Skin Res Technol. 2017; 23:212–220. PMID: 27427161.
Article19. González-Serva A, Kroumpouzos G. Demonstration of polarizable crystals in fresh comedonal extracts: sebum crystallizes. Acta Derm Venereol. 2004; 84:418–421. PMID: 15844629.
Article20. Tóth BI, Oláh A, Szöllosi AG, Czifra G, Bíró T. “Sebocytes' makeup”: novel mechanisms and concepts in the physiology of the human sebaceous glands. Pflugers Arch. 2011; 461:593–606. PMID: 21384129.21. Thiele JJ, Schroeter C, Hsieh SN, Podda M, Packer L. The antioxidant network of the stratum corneum. Curr Probl Dermatol. 2001; 29:26–42. PMID: 11225199.
Article22. Passi S, De Pità O, Puddu P, Littarru GP. Lipophilic antioxidants in human sebum and aging. Free Radic Res. 2002; 36:471–477. PMID: 12069113.
Article23. Luebberding S, Krueger N, Kerscher M. Age-related changes in skin barrier function - quantitative evaluation of 150 female subjects. Int J Cosmet Sci. 2013; 35:183–190. PMID: 23113564.
Article24. Boireau-Adamezyk E, Baillet-Guffroy A, Stamatas GN. Age-dependent changes in stratum corneum barrier function. Skin Res Technol. 2014; 20:409–415. PMID: 24517174.
Article25. Shah MG, Maibach HI. Estrogen and skin. An overview. Am J Clin Dermatol. 2001; 2:143–150. PMID: 11705091.26. Piérard GE, Humbert P, Berardesca E, Gaspard U, Hermanns-Lê T, Piérard-Franchimont C. Revisiting the cutaneous impact of oral hormone replacement therapy. Biomed Res Int. 2013; 2013:971760. PMID: 24455744.
Article27. Slominski A, Zbytek B, Nikolakis G, Manna PR, Skobowiat C, Zmijewski M, et al. Steroidogenesis in the skin: implications for local immune functions. J Steroid Biochem Mol Biol. 2013; 137:107–123. PMID: 23435015.
Article28. Chang KC, Wang Y, Oh IG, Jenkins S, Freedman LP, Thompson CC, et al. Estrogen receptor beta is a novel therapeutic target for photoaging. Mol Pharmacol. 2010; 77:744–750. PMID: 20110405.29. Zouboulis CC, Chen WC, Thornton MJ, Qin K, Rosenfield R. Sexual hormones in human skin. Horm Metab Res. 2007; 39:85–95. PMID: 17326004.
Article30. Seo YJ, Li ZJ, Choi DK, Sohn KC, Kim HR, Lee Y, et al. Regional difference in sebum production by androgen susceptibility in human facial skin. Exp Dermatol. 2014; 23:70–72. PMID: 24289322.
Article31. Chu M, Kollias N. Documentation of normal stratum corneum scaling in an average population: features of differences among age, ethnicity and body site. Br J Dermatol. 2011; 164:497–507. PMID: 21054338.
Article32. Pomari E, Dalla Valle L, Pertile P, Colombo L, Thornton MJ. Intracrine sex steroid synthesis and signaling in human epidermal keratinocytes and dermal fibroblasts. FASEB J. 2015; 29:508–524. PMID: 25392269.
Article33. Inoue T, Miki Y, Abe K, Hatori M, Hosaka M, Kariya Y, et al. The role of estrogen-metabolizing enzymes and estrogen receptors in human epidermis. Mol Cell Endocrinol. 2011; 344:35–40. PMID: 21740958.
Article34. Zapata HJ, Quagliarello VJ. The microbiota and microbiome in aging: potential implications in health and age-related diseases. J Am Geriatr Soc. 2015; 63:776–781. PMID: 25851728.
Article35. Luebberding S, Krueger N, Kerscher M. Skin physiology in men and women: in vivo evaluation of 300 people including TEWL, SC hydration, sebum content and skin surface pH. Int J Cosmet Sci. 2013; 35:477–483. PMID: 23713991.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Effect of Lipid Peroxide in Skin Surface Lipid on the Clinical Aspect of Acne and Melasma
- Skin Dose Distrubution with Spoiler of 6 MV X-ray for head and Neck Tumor
- A study on the changes of sebaceous gland activity during aging by analysis of skin surface lipids
- Skin Hydration Status and Skin Surface pH According to the Body Parts of the Aged with Immobilization
- Quantitative Analysis of Solvent Extracted Skin Surface Lipid in Human Skin ( - hexane, hexane/ methanol, ethanol - )