Pediatr Gastroenterol Hepatol Nutr.
2015 Dec;18(4):224-229. 10.5223/pghn.2015.18.4.224.
Cyclic Vomiting Syndrome: A Functional Disorder
- Affiliations
-
- 1Division of Gastroenterology, Hepatology and Nutrition, Cincinnati Children's Hospital Medical Center, Cincinnati, OH, USA. ajay.kaul@cchmc.org
- 2Department of Pediatrics, NSCB Medical College, Jabalpur, India.
- KMID: 2383299
- DOI: http://doi.org/10.5223/pghn.2015.18.4.224
Abstract
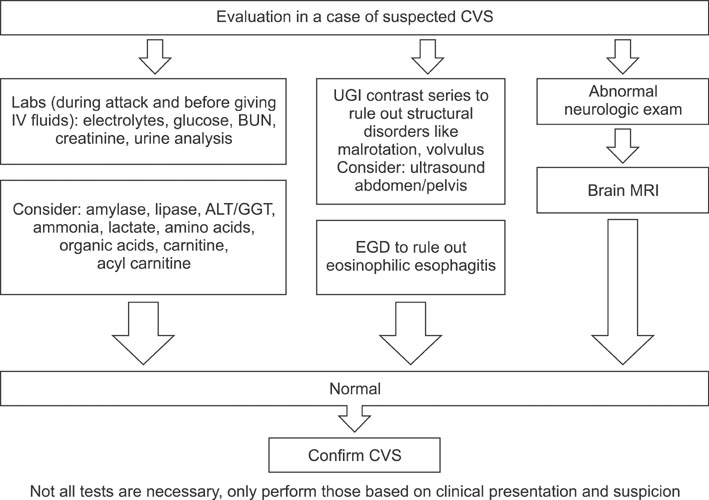
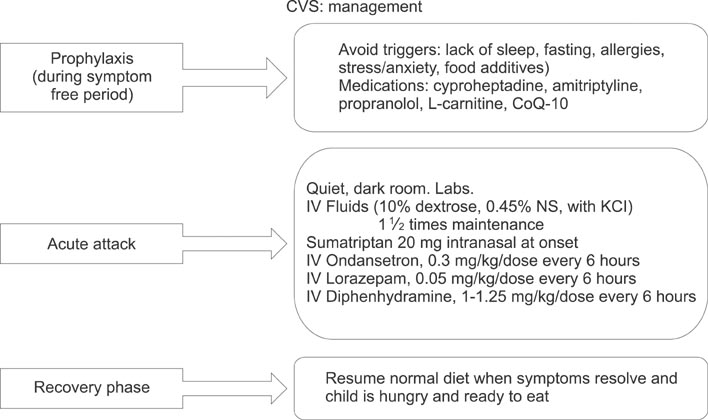
- Cyclic vomiting syndrome (CVS) is a functional disorder characterized by stereotypical episodes of intense vomiting separated by weeks to months. Although it can occur at any age, the most common age at presentation is 3-7 years. There is no gender predominance. The precise pathophysiology of CVS is not known but a strong association with migraine headaches, in the patient as well as the mother indicates that it may represent a mitochondriopathy. Studies have also suggested the role of an underlying autonomic neuropathy involving the sympathetic nervous system in its pathogenesis. CVS has known triggers in many individuals and avoiding these triggers can help prevent the onset of the episodes. It typically presents in four phases: a prodrome, vomiting phase, recovery phase and an asymptomatic phase until the next episode. Complications such as dehydration and hematemesis from Mallory Wise tear of the esophageal mucosa may occur in more severe cases. Blood and urine tests and abdominal imaging may be indicated depending upon the severity of symptoms. Brain magnetic resonance imaging and upper gastrointestinal endoscopy may also be indicated in certain circumstances. Management of an episode after it has started ('abortive treatment') includes keeping the patient in a dark and quiet room, intravenous hydration, ondansetron, sumatriptan, clonidine, and benzodiazepines. Prophylactic treatment includes cyproheptadine, propranolol and amitriptyline. No mortality has been reported as a direct result of CVS and many children outgrow it over time. A subset may develop other functional disorders like irritable bowel syndrome and migraine headaches.
Keyword
MeSH Terms
-
Amitriptyline
Benzodiazepines
Brain
Child
Clonidine
Cyproheptadine
Dehydration
Endoscopy, Gastrointestinal
Hematemesis
Humans
Irritable Bowel Syndrome
Magnetic Resonance Imaging
Migraine Disorders
Mortality
Mothers
Mucous Membrane
Ondansetron
Propranolol
Sumatriptan
Sympathetic Nervous System
Vomiting*
Amitriptyline
Benzodiazepines
Clonidine
Cyproheptadine
Ondansetron
Propranolol
Sumatriptan
Figure
Reference
-
1. Saps M, Nichols-Vinueza DX, Rosen JM, Velasco-Benítez CA. Prevalence of functional gastrointestinal disorders in Colombian school children. J Pediatr. 2014; 164:542–545.e1.2. Devanarayana NM, Adhikari C, Pannala W, Rajindrajith S. Prevalence of functional gastrointestinal diseases in a cohort of Sri Lankan adolescents: comparison between Rome II and Rome III criteria. J Trop Pediatr. 2011; 57:34–39.
Article3. Van Tilburg MAL, Walker LS, Palsson OS, Kim SM, Spiegel BM, Siller RC, et al. Prevalence of child/adolescent functional gastrointestinal disorders in a national U.S. community sample. Gastroenterology. 2014; 146:5 Suppl 1. S143–S144.4. Fitzpatrick E, Bourke B, Drumm B, Rowland M. The incidence of cyclic vomiting syndrome in children: population-based study. Am J Gastroenterol. 2008; 103:991–995. quiz 996
Article5. Liao KY, Chang FY, Wu LT, Wu TC. Cyclic vomiting syndrome in Taiwanese children. J Formos Med Assoc. 2011; 110:14–18.
Article6. Lin YP, Ni YH, Weng WC, Lee WT. Cyclic vomiting syndrome and migraine in children. J Formos Med Assoc. 2011; 110:382–387.
Article7. Withers GD, Silburn SR, Forbes DA. Precipitants and aetiology of cyclic vomiting syndrome. Acta Paediatr. 1998; 87:272–277.
Article8. Li BU, Balint JP. Cyclic vomiting syndrome: evolution in our understanding of a brain-gut disorder. Adv Pediatr. 2000; 47:117–160.9. Symon DN, Russell G. The relationship between cyclic vomiting syndrome and abdominal migraine. J Pediatr Gastroenterol Nutr. 1995; 21:Suppl 1. S42–S43.
Article10. Venkatesan T, Prieto T, Barboi A, Li B, Schroeder A, Hogan W, et al. Autonomic nerve function in adults with cyclic vomiting syndrome: a prospective study. Neurogastroenterol Motil. 2010; 22:1303–1307. e339
Article11. Taché Y. Cyclic vomiting syndrome: the corticotropin-releasing-factor hypothesis. Dig Dis Sci. 1999; 44:8 Suppl. 79S–86S.12. Zaki EA, Freilinger T, Klopstock T, Baldwin EE, Heisner KR, Adams K, et al. Two common mitochondrial DNA polymorphisms are highly associated with migraine headache and cyclic vomiting syndrome. Cephalalgia. 2009; 29:719–728.
Article13. Boles RG, Zaki EA, Lavenbarg T, Hejazi R, Foran P, Freeborn J, et al. Are pediatric and adult-onset cyclic vomiting syndrome (CVS) biologically different conditions? Relationship of adult-onset CVS with the migraine and pediatric CVS-associated common mtDNA polymorphisms 16519T and 3010A. Neurogastroenterol Motil. 2009; 21:936–e72.
Article14. Boles RG, Adams K, Li BU. Maternal inheritance in cyclic vomiting syndrome. Am J Med Genet A. 2005; 133A:71–77.
Article15. Wallace D, Martin AL, Park B. Cannabinoid hyperemesis: marijuana puts patients in hot water. Australas Psychiatry. 2007; 15:156–158.
Article16. Chang YH, Windish DM. Cannabinoid hyperemesis relieved by compulsive bathing. Mayo Clin Proc. 2009; 84:76–78.
Article17. Wong BS, Camilleri M, Busciglio I, Carlson P, Szarka LA, Burton D, et al. Pharmacogenetic trial of a cannabinoid agonist shows reduced fasting colonic motility in patients with nonconstipated irritable bowel syndrome. Gastroenterology. 2011; 141:1638–1647. 1647.e1–1647.e7.
Article18. Sullivan S. Cannabinoid hyperemesis. Can J Gastroenterol. 2010; 24:284–285.
Article19. Patterson DA, Smith E, Monahan M, Medvecz A, Hagerty B, Krijger L, et al. Cannabinoid hyperemesis and compulsive bathing: a case series and paradoxical pathophysiological explanation. J Am Board Fam Med. 2010; 23:790–793.
Article20. Noel RJ, Putnam PE, Rothenberg ME. Eosinophilic esophagitis. N Engl J Med. 2004; 351:940–941.
Article21. Landres RT, Kuster GG, Strum WB. Eosinophilic esophagitis in a patient with vigorous achalasia. Gastroenterology. 1978; 74:1298–1301.
Article22. Liacouras CA, Furuta GT, Hirano I, Atkins D, Attwood SE, Bonis PA, et al. Eosinophilic esophagitis: updated consensus recommendations for children and adults. J Allergy Clin Immunol. 2011; 128:3–20.
Article23. Wen T, Dellon ES, Moawad FJ, Furuta GT, Aceves SS, Rothenberg ME. Transcriptome analysis of proton pump inhibitor-responsive esophageal eosinophilia reveals proton pump inhibitor-reversible allergic inflammation. J Allergy Clin Immunol. 2015; 135:187–197.
Article24. Papadopoulou A, Koletzko S, Heuschkel R, Dias JA, Allen KJ, Murch SH, et al. ESPGHAN Eosinophilic Esophagitis Working Group and the Gastroenterology Committee. Management guidelines of eosinophilic esophagitis in childhood. J Pediatr Gastroenterol Nutr. 2014; 58:107–118.
Article25. Li BU, Lefevre F, Chelimsky GG, Boles RG, Nelson SP, Lewis DW, et al. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition. North American Society for Pediatric Gastroenterology, Hepatology, and Nutrition consensus statement on the diagnosis and management of cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr. 2008; 47:379–393.
Article26. Paul SP, Barnard P, Soondrum K, Candy DC. Antimigraine (low-amine) diet may be helpful in children with cyclic vomiting syndrome. J Pediatr Gastroenterol Nutr. 2012; 54:698–699.
Article27. Aanpreung P, Vajaradul C. Cyclic vomiting syndrome in Thai children. J Med Assoc Thai. 2002; 85:Suppl 2. S743–S748.28. Hikita T, Kodama H, Nakamoto N, Kaga F, Amakata K, Ogita K, et al. Effective prophylactic therapy for cyclic vomiting syndrome in children using valproate. Brain Dev. 2009; 31:411–413.
Article29. Boles RG, Lovett-Barr MR, Preston A, Li BU, Adams K. Treatment of cyclic vomiting syndrome with co-enzyme Q10 and amitriptyline, a retrospective study. BMC Neurol. 2010; 10:10.
Article30. Van Calcar SC, Harding CO, Wolff JA. L-carnitine administration reduces number of episodes in cyclic vomiting syndrome. Clin Pediatr (Phila). 2002; 41:171–174.
Article31. Hikita T, Kodama H, Kaneko S, Amakata K, Ogita K, Mochizuki D, et al. Sumatriptan as a treatment for cyclic vomiting syndrome: a clinical trial. Cephalalgia. 2011; 31:504–507.
Article32. Palmer GM, Cameron DJ. Use of intravenous midazolam and clonidine in cyclical vomiting syndrome: a case report. Paediatr Anaesth. 2005; 15:68–72.
Article33. Sato T, Igarashi N, Minami S, Okabe T, Hashimoto H, Hasui M, et al. Recurrent attacks of vomiting, hypertension and psychotic depression: a syndrome of periodic catecholamine and prostaglandin discharge. Acta Endocrinol (Copenh). 1988; 117:189–197.
Article34. Lee LY, Abbott L, Moodie S, Anderson S. Cyclic vomiting syndrome in 28 patients: demographics, features and outcomes. Eur J Gastroenterol Hepatol. 2012; 24:939–943.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cyclic Vomiting Syndrome Developed after Stroke
- Clinical Approach to Functional Gastrointestinal Disorders in Children: Revolve Around on Cyclic Vomiting Syndrome and Aerophagia
- Recent Concepts on Cyclic Vomiting Syndrome in Children
- Diagnosis and Treatment of Functional Nausea and Vomiting
- Understanding the Rome IV: Gastroduodenal Disorders