Yonsei Med J.
2007 Oct;48(5):833-838. 10.3349/ymj.2007.48.5.833.
A New Classification for Idiopathic Genu Vara
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. pedhkim@yuhs.ac
- 2Department of Orthopaedic Surgery, Hallym University College of Medicine, Anyang, Korea.
- 3BK21 Research Team of Nanobiomaterials for the Cell-based Implants, Seoul, Korea.
- KMID: 1122622
- DOI: http://doi.org/10.3349/ymj.2007.48.5.833
Abstract
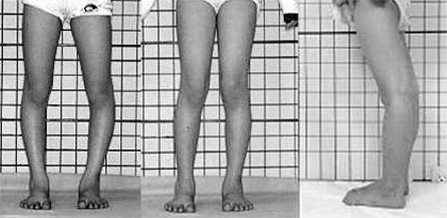
- PURPOSE: Past classification for the treatment of idiopathic genu vara depended simply on the measurement of distance between the knees, without attention to the rotational profile of the lower extremity. We retrospectively analyzed anatomical causes of idiopathic genu vara. PATIENTS AND METHODS: Twenty eight patients with idiopathic genu vara were included in this study. All patients were surgically treated. To evaluate the angular deformity, a standing orthoroentgenogram was taken and the lateral distal femoral angle and the medial proximal tibial angle were measured. In order to assess any accompanying torsional deformity, both femoral anteversion and tibial external rotation were measured using computerized tomographic scans. A derotational osteotomy was performed at the femur or tibia to correct rotational deformity, and a correctional osteotomy was performed at the tibia to correct angular deformity. RESULTS: Satisfactory functional results were obtained in all cases. Genu vara was divided into 3 groups according to the nature of the deformity; group 1 (6 patients) with increased femoral anteversion, group 2 (10 patients) with proximal tibial varus deformity alone, and group 3 (12 patients) with proximal tibial varus deformity accompanied by increased external tibial rotation. CONCLUSION: The success seen in our cases highlights the importance of an accurate preoperative analysis that accounts for both rotational and angular deformities that may underlie idiopathic genu vara.
Keyword
MeSH Terms
Figure
Reference
-
1. Kling TF Jr, Hensinger RN. Angular and torsional deformities of the lower limbs in children. Clin Orthop Relat Res. 1983. 176:136–147.
Article2. Shtarker H, Volpin G, Stolero J, Kaushansky A, Samchukov M. Correction of combined angular and rotational deformities by the Ilizarov method. Clin Orthop Relat Res. 2002. 402:184–195.
Article3. Delgado ED, Schoenecker PL, Rich MM, Capelli AM. Treatment of severe torsional malalignment syndrome. J Pediatr Orthop. 1996. 16:484–488.
Article4. Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994. 25:425–465.
Article5. Fabry G, MacEwen GD, Shands AR Jr. Torsion of the femur. A follow-up study in normal and abnormal conditions. J Bone Joint Surg Am. 1973. 55:1726–1738.6. Krengel WF 3rd, Staheli LT. Tibial rotational osteotomy for idiopathic torsion. A comparison of the proximal and distal osteotomy levels. Clin Orthop Relat Res. 1992. 283:285–289.7. Staheli LT. Rotational problems in children. Instr Course Lect. 1994. 43:199–209.
Article8. Visser JD, Jonkers A, Hillen B. Hip joint measurements with computerized tomography. J Pediatr Orthop. 1982. 2:143–146.
Article9. Meister K, James SL. Proximal tibial derotation osteotomy for anterior knee pain in the miserably malaligned extremity. Am J Orthop. 1995. 24:149–155.10. Halpern AA, Tanner J, Rinsky L. Does persistent fetal femoral anteversion contribute to osteoarthritis?: a preliminary report. Clin Orthop Relat Res. 1979. 145:213–216.11. Heller MO, Bergmann G, Deuretzbacher G, Claes L, Haas NP, Duda GN. Influence of femoral anteversion on proximal femoral loading: measurement and simulation in four patients. Clin Biomech (Bristol, Avon). 2001. 16:644–649.
Article12. Kitaoka HB, Weiner DS, Cook AJ, Hoyt WA Jr, Askew MJ. Relationship between femoral anteversion and osteoarthritis of the hip. J Pediatr Orthop. 1989. 9:396–404.
Article13. Turner MS, Smillie IS. The effect of tibial torsion on the pathology of the knee. J Bone Joint Surg Br. 1981. 63:396–398.14. Wedge JH, Munkacsi I, Loback D. Anteversion of the femur and idiopathic osteoarthrosis of the hip. J Bone Joint Surg Am. 1989. 71:1040–1043.
Article15. Alvik I. Increased anteversion of the femur as the only manifestation of dysplasia of the hip. Clin Orthop. 1962. 22:16–20.16. Eckhoff DG, Kramer RC, Alongi CA, VanGerven DP. Femoral anteversion and arthritis of the knee. J Pediatr Orthop. 1994. 14:608–610.
Article17. Cooke TD, Price N, Fisher B, Hedden D. The inwardly pointing knee. An unrecognized problem of external rotational malalignment. Clin Orthop Relat Res. 1990. 260:56–60.18. Herzenberg JE, Smith JD, Paley D. Correcting torsional deformities with Ilizarov's apparatus. Clin Orthop Relat Res. 1994. 302:36–41.19. Svenningsen S, Apalset K, Terjesen T, Anda S. Osteotomy for femoral anteversion. Complications in 95 children. Acta Orthop Scand. 1989. 60:401–405.
Article20. James SL. Kennedy JC, editor. Chondromalacia of the patella in the adolescent. The injured Adolescent Knee. 1979. Baltimore: Williams & Wilkins;205–251.21. Lee TQ, Anzel SH, Bennett KA, Pang D, Kim WC. The influence of fixed rotational deformities of the femur on the patellofemoral contact pressures in human cadaver knees. Clin Orthop Relat Res. 1994. 302:69–74.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Causes and Surgical Treatment of Idiopathic Genu Vara
- A Child with Familial Hypophosphatemic Ricket: A case report
- The Classification of Idiopathic Scoliosis
- The Efficacy of Percutaneous Lateral Hemiepiphysiodesis on Angular Correction in Idiopathic Adolescent Genu Varum
- Congenital Coxa Vara, Acquired Coxa Vara and Valga