Clin Orthop Surg.
2011 Mar;3(1):24-33. 10.4055/cios.2011.3.1.24.
Changes in Level of the Conus after Corrective Surgery for Scoliosis: MRI-Based Preliminary Study in 31 Patients
- Affiliations
-
- 1Depatment of Orthopaedics, Korea University Ansan Hospital, Ansan, Korea.
- 2Department of Orthopaedics, Korea University Guro Hospital, Seoul, Korea. spine@korea.ac.kr
- 3Department of Radiology, Korea University Guro Hospital, Seoul, Korea.
- KMID: 999457
- DOI: http://doi.org/10.4055/cios.2011.3.1.24
Abstract
- BACKGROUND
Detection of postoperative spinal cord level change can provide basic information about the spinal cord status, and electrophysiological studies regarding this point should be conducted in the future.
METHODS
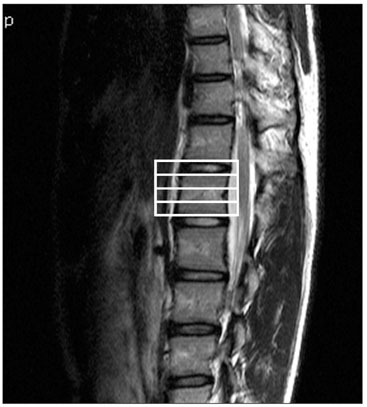
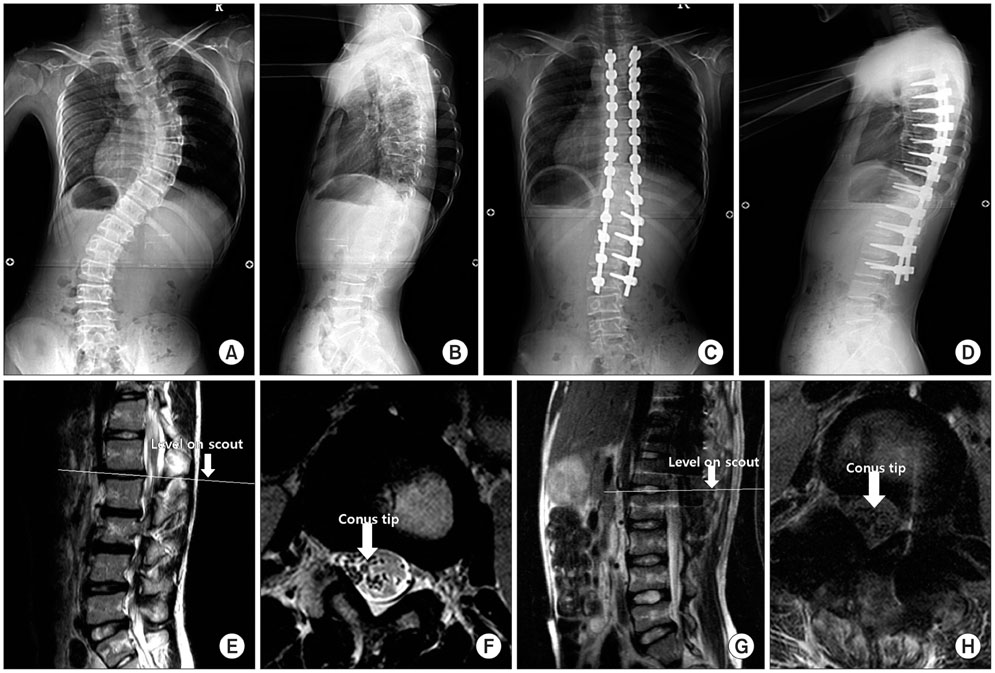
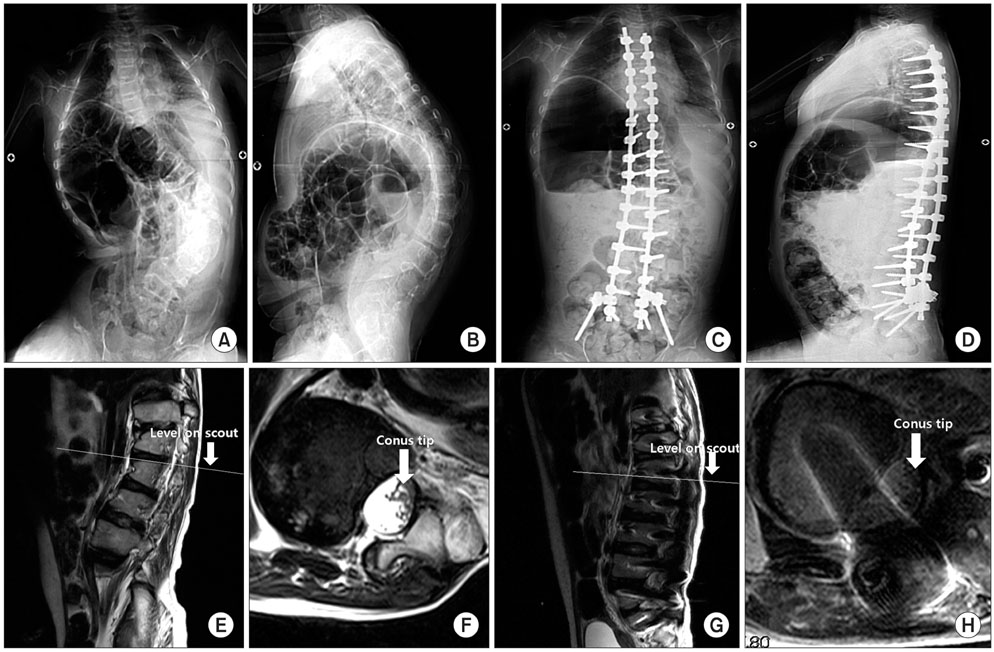
To determine the changes in the spinal cord level postoperatively and the possible associated factors, we prospectively studied 31 patients with scoliosis. All the patients underwent correction and posterior fusion using pedicle screws and rods between January 2008 and March 2009. The pre- and postoperative conus medullaris levels were determined by matching the axial magnetic resonance image to the sagittal scout image. The patients were divided according to the change in the postoperative conus medullaris level. The change group was defined as the patients who showed a change of more than one divided section in the vertebral column postoperatively, and the parameters of the change and non-change groups were compared.
RESULTS
The mean pre- and postoperative Cobb's angle of the coronal curve was 76.80degrees +/- 17.19degrees and 33.23degrees +/- 14.39degrees, respectively. Eleven of 31 patients showed a lower conus medullaris level postoperatively. There were no differences in the pre- and postoperative magnitude of the coronal curve, lordosis and kyphosis between the groups. However, the postoperative degrees of correction of the coronal curve and lumbar lordosis were higher in the change group. There were also differences in the disease entities between the groups. A higher percentage of patients with Duchene muscular dystrophy had a change in level compared to that of the patients with cerebral palsy (83.3% vs. 45.5%, respectively).
CONCLUSIONS
The conus medullaris level changed postoperatively in the patients with severe scoliosis. Overall, the postoperative degree of correction of the coronal curve was higher in the change group than that in the non-change group. The degrees of correction of the coronal curve and lumbar lordosis were related to the spinal cord level change after scoliosis correction.
MeSH Terms
-
Adolescent
Adult
Cerebral Palsy/complications
Child
Female
Humans
Kyphosis/radiography
Lordosis/radiography
Lumbar Vertebrae/radiography/surgery
*Magnetic Resonance Imaging
Male
Muscular Dystrophy, Duchenne/complications
Prospective Studies
Scoliosis/complications/radiography/*surgery
Severity of Illness Index
Spinal Cord/*pathology
Thoracic Vertebrae/radiography/surgery
Young Adult
Figure
Reference
-
1. Lehman RA Jr, Lenke LG, Keeler KA, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine (Phila Pa 1976). 2008. 33(14):1598–1604.
Article2. Steinmetz MP, Rajpal S, Trost G. Segmental spinal instrumentation in the management of scoliosis. Neurosurgery. 2008. 63:3 Suppl. 131–138.
Article3. Lenke LG, O'Leary PT, Bridwell KH, Sides BA, Koester LA, Blanke KM. Posterior vertebral column resection for severe pediatric deformity: minimum two-year follow-up of thirty-five consecutive patients. Spine (Phila Pa 1976). 2009. 34(20):2213–2221.4. Luhmann SJ, Lenke LG, Kim YJ, Bridwell KH, Schootman M. Thoracic adolescent idiopathic scoliosis curves between 70 degrees and 100 degrees: is anterior release necessary? Spine (Phila Pa 1976). 2005. 30(18):2061–2067.5. Suh SW, Modi HN, Yang J, Song HR, Jang KM. Posterior multilevel vertebral osteotomy for correction of severe and rigid neuromuscular scoliosis: a preliminary study. Spine (Phila Pa 1976). 2009. 34(12):1315–1320.
Article6. Reid JD. Effects of flexion-extension movements of the head and spine upon the spinal cord and nerve roots. J Neurol Neurosurg Psychiatry. 1960. 23(3):214–221.
Article7. Yuan Q, Dougherty L, Margulies SS. In vivo human cervical spinal cord deformation and displacement in flexion. Spine (Phila Pa 1976). 1998. 23(15):1677–1683.
Article8. Chu WC, Lam WW, Chan YL, et al. Relative shortening and functional tethering of spinal cord in adolescent idiopathic scoliosis Study with multiplanar reformat magnetic resonance imaging and somatosensory evoked potential. Spine (Phila Pa 1976). 2006. 31(1):E19–E25.9. Chu WC, Man GC, Lam WW, et al. Morphological and functional electrophysiological evidence of relative spinal cord tethering in adolescent idiopathic scoliosis. Spine (Phila Pa 1976). 2008. 33(6):673–680.
Article10. Porter RW. The pathogenesis of idiopathic scoliosis: uncoupled neuro-osseous growth? Eur Spine J. 2001. 10(6):473–481.
Article11. Roth M. Idiopathic scoliosis caused by a short spinal cord. Acta Radiol Diagn (Stockh). 1968. 7(3):257–271.
Article12. Sun X, Chu WC, Cheng JC, et al. Do adolescents with a severe idiopathic scoliosis have higher locations of the conus medullaris than healthy adolescents? J Pediatr Orthop. 2008. 28(6):669–673.
Article13. Sun X, Qiu Y, Zhu Z, et al. Variations of the position of the cerebellar tonsil in idiopathic scoliotic adolescents with a cobb angle > 40 degrees: a magnetic resonance imaging study. Spine (Phila Pa 1976). 2007. 32(15):1680–1686.
Article14. Ranger MR, Irwin GJ, Bunbury KM, Peutrell JM. Changing body position alters the location of the spinal cord within the vertebral canal: a magnetic resonance imaging study. Br J Anaesth. 2008. 101(6):804–809.
Article15. Rudisch A, Kremser C, Peer S, Kathrein A, Judmaier W, Daniaux H. Metallic artifacts in magnetic resonance imaging of patients with spinal fusion: a comparison of implant materials and imaging sequences. Spine (Phila Pa 1976). 1998. 23(6):692–699.
Article16. Chang SD, Lee MJ, Munk PL, Janzen DL, MacKay A, Xiang QS. MRI of spinal hardware: comparison of conventional T1-weighted sequence with a new metal artifact reduction sequence. Skeletal Radiol. 2001. 30(4):213–218.
Article17. Lee MJ, Kim S, Lee SA, et al. Overcoming artifacts from metallic orthopedic implants at high-field-strength MR imaging and multi-detector CT. Radiographics. 2007. 27(3):791–803.
Article18. Petersilge CA. Evaluation of the postoperative spine: reducing hardware artifacts during magnetic resonance imaging. Semin Musculoskelet Radiol. 2000. 4(3):293–297.
Article19. Stradiotti P, Curti A, Castellazzi G, Zerbi A. Metal-related artifacts in instrumented spine. Techniques for reducing artifacts in CT and MRI: state of the art. Eur Spine J. 2009. 18:Suppl 1. 102–108.
Article20. Saifuddin A, Burnett SJ, White J. The variation of position of the conus medullaris in an adult population. A magnetic resonance imaging study. Spine (Phila Pa 1976). 1998. 23(13):1452–1456.
Article21. Chu WC, Lam WM, Ng BK, et al. Relative shortening and functional tethering of spinal cord in adolescent scoliosis: result of asynchronous neuro-osseous growth, summary of an electronic focus group debate of the IBSE. Scoliosis. 2008. 3:8.22. Porter RW. Idiopathic scoliosis: the relation between the vertebral canal and the vertebral bodies. Spine (Phila Pa 1976). 2000. 25(11):1360–1366.23. Hahn F, Hauser D, Espinosa N, Blumenthal S, Min K. Scoliosis correction with pedicle screws in Duchenne muscular dystrophy. Eur Spine J. 2008. 17(2):255–261.
Article24. Manzur AY, Kinali M, Muntoni F. Update on the management of Duchenne muscular dystrophy. Arch Dis Child. 2008. 93(11):986–990.
Article25. Modi HN, Suh SW, Yang JH, et al. Surgical complications in neuromuscular scoliosis operated with posterior-only approach using pedicle screw fixation. Scoliosis. 2009. 4:11.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Magnetic Resonance Imaging Observations of the Conus Medullaris in a Korean Population
- The Tip Level of the Conus Medullaris by Magnetic Resonance Imaging and Cadaver Studies in Korean Adults
- Clinical and MR Findings of Tethered Cord Syndrome
- A Case of Tethered Cord Syndrome
- Decompressive Effect of Indirect Decompression in Thoracolumbar Burst Fracture