Korean J Radiol.
2011 Feb;12(1):97-106. 10.3348/kjr.2011.12.1.97.
Catheter-Directed Thrombolysis with a Continuous Infusion of Low-Dose Urokinase for Non-Acute Deep Venous Thrombosis of the Lower Extremity
- Affiliations
-
- 1Department of Vascular Surgery, Shandong Provincial Hospital, Shandong University, Ji'nan 250021, China. zhangjingyongfree@163.com
- KMID: 991687
- DOI: http://doi.org/10.3348/kjr.2011.12.1.97
Abstract
OBJECTIVE
We wanted to evaluate the feasibility of catheter-directed thrombolysis with a continuous infusion of low-dose urokinase for treating non-acute (less than 14 days) deep venous thrombosis of the lower extremity.
MATERIALS AND METHODS
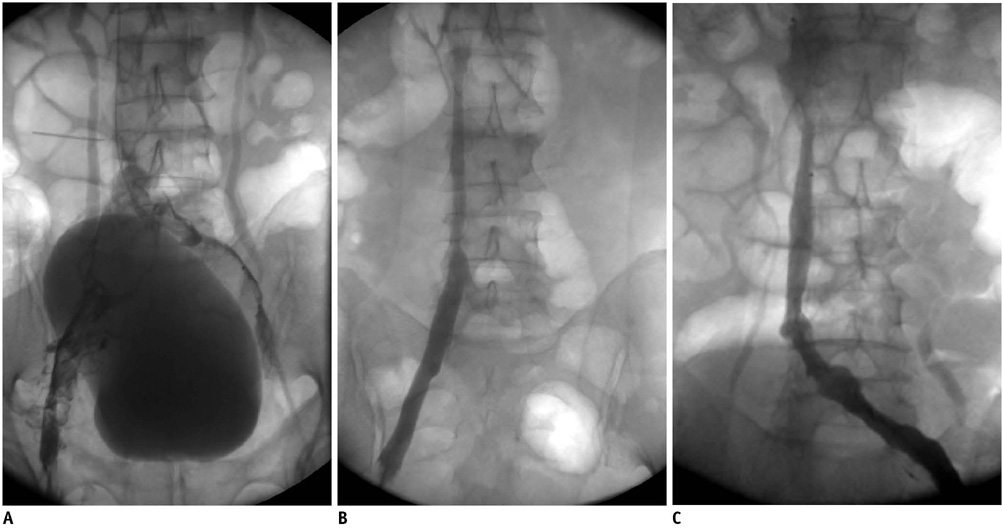
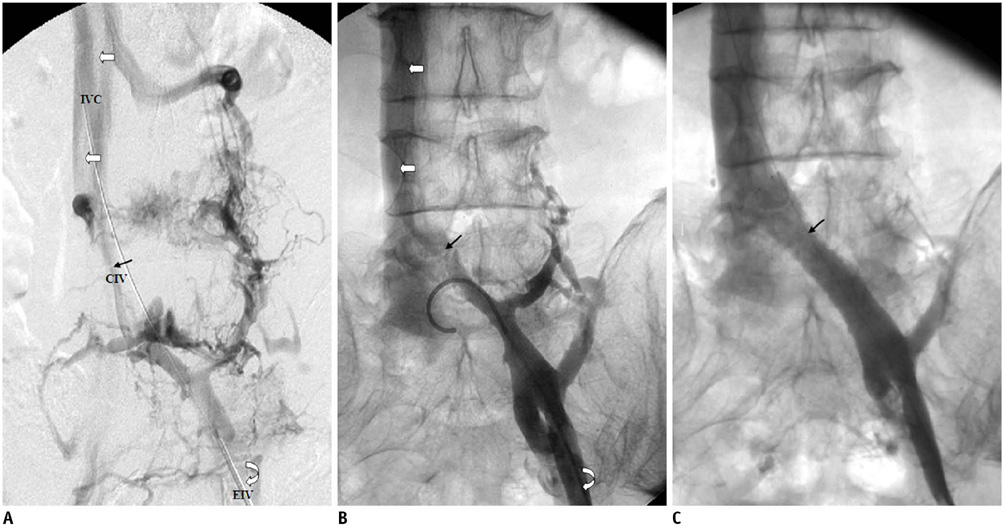
The clinical data of 110 patients who were treated by catheter-directed thrombolysis with a continuous infusion of low-dose urokinase for lower extremity deep venous thrombosis was analysed. Adjunctive angioplasty or/and stenting was performed for the residual stenosis. Venous recanalization was graded by pre- and post-treatment venography. Follow-up was performed by clinical evaluation and Doppler ultrasound.
RESULTS
A total of 112 limbs with deep venous thrombosis with a mean symptom duration of 22.7 days (range: 15-38 days) were treated with a urokinase infusion (mean: 3.5 million IU) for a mean of 196 hours. After thrombolysis, stent placement was performed in 25 iliac vein lesions and percutaneous angioplasty (PTA) alone was done in five iliac veins. Clinically significant recanalization was achieved in 81% (90 of 112) of the treated limbs; complete recanalization was achieved in 28% (31 of 112) and partial recanalization was achieved in 53% (59 of 112). Minor bleeding occurred in 14 (13%) patients, but none of the patients suffered from major bleeding or symptomatic pulmonary embolism. During follow-up (mean: 15.2 months, range: 3-24 months), the veins were patent in 74 (67%) limbs. Thirty seven limbs (32%) showed progression of the stenosis with luminal narrowing more than 50%, including three with rethrombosis, while one revealed an asymptomatic iliac vein occlusion; 25 limbs (22%) developed mild post-thrombotic syndrome, and none had severe post-thrombotic syndrome. Valvular reflux occurred in 24 (21%) limbs.
CONCLUSION
Catheter-directed thrombolysis with a continuous infusion of low-dose urokinase combined with adjunctive iliac vein stenting is safe and effective for removal of the clot burden and for restoration of the venous flow in patients with non-acute lower extremity deep venous thrombosis.
Keyword
MeSH Terms
-
Adult
Aged
Angioplasty, Balloon
*Catheterization, Peripheral
Combined Modality Therapy
Female
Fibrinolytic Agents/*administration & dosage
Humans
*Infusion Pumps
Infusions, Intravenous
Leg/*blood supply
Male
Middle Aged
Phlebography
*Thrombolytic Therapy/methods
Ultrasonography, Doppler
Urokinase-Type Plasminogen Activator/*administration & dosage
Vascular Patency
Venous Thrombosis/*drug therapy/radiography/ultrasonography
Figure
Reference
-
1. Blum A, Roche E. Endovascular management of acute deep vein thrombosis. Am J Med. 2005. 118:31S–36S.2. Baekgaard N, Broholm R, Just S, Jørgensen M, Jensen LP. Long-term results using catheter-directed thrombolysis in 103 lower limbs with acute iliofemoral venous thrombosis. Eur J Vasc Endovasc Surg. 2010. 39:112–117.3. Grossman C, McPherson S. Safety and efficacy of catheter-directed thrombolysis for iliofemoral venous thrombosis. AJR Am J Roentgenol. 1999. 172:667–672.4. Kearon C, Kahn SR, Agnelli G, Goldhaber S, Raskob GE, Comerota AJ. Antithrombotic therapy for venous thromboembolic disease: American College of Chest Physicians Evidence Based Clinical Practice Guidelines (8th Edition). Chest. 2008. 133:454S–545S.5. Vedantham S, Millward SF, Cardella JF, Hofmann LV, Razavi MK, Grassi CJ, et al. Society of Interventional Radiology position statement: treatment of acute iliofemoral deep vein thrombosis with use of adjunctive catheter-directed intrathrombus thrombolysis. J Vasc Interv Radiol. 2006. 17:613–616.6. Lou WS, Gu JP, He X, Chen L, Su HB, Chen GP, et al. Endovascular treatment for iliac vein compression syndrome: a comparison between the presence and absence of secondary thrombosis. Korean J Radiol. 2009. 10:135–143.7. Patel N, Sacks D, Patel RI, Moresco KP, Ouriel K, Gray R, et al. SIR reporting standards for the treatment of acute limb ischemia with use of transluminal removal of arterial thrombus. J Vasc Interv Radiol. 2003. 14:S453–S465.8. Sacks D, McClenny TE, Cardella JF, Lewis CA. Society of Interventional radiology clinical practice guidelines. J Vasc Interv Radiol. 2003. 14:S199–S202.9. Mewissen MW, Seabrook GR, Meissner MH, Cynamon J, Labropoulos N, Haughton SH. Catheter-directed thrombolysis for lower extremity deep venous thrombosis: report of a national multicenter registry. Radiology. 1999. 211:39–49.10. Vedantham S, Grassi CJ, Ferral H, Patel NH, Thorpe PE, Antonacci VP, et al. Reporting standards for endovascular treatment of lower extremity deep vein thrombosis. J Vasc Interv Radiol. 2006. 17:417–434.11. Park YJ, Choi JY, Min SK, Lee T, Jung IM, Chung JK, et al. Restoration of patency in iliofemoral deep vein thrombosis with catheter-directed thrombolysis does not always prevent post-thrombotic damage. Eur J Vasc Endovasc Surg. 2008. 36:725–730.12. Prandoni P, Lensing AW, Prins MH, Frulla M, Marchiori A, Bernardi E, et al. Below-knee elastic compression stockings to prevent the post-thrombotic syndrome: a randomized, controlled trial. Ann Intern Med. 2004. 141:249–256.13. Mattos MA, Sumner DS. Gloviczki P, Yao JS, editors. Direct noninvasive tests (duplex scan) for the evaluation of chronic venous obstruction and valvular incompetence. Handbook of venous disorders. 2001. 2nd ed. New York, NY: Arnold;120–131.14. Kölbel T, Lindh M, Akesson M, Wassèlius J, Gottsäter A, Ivancev K. Chronic iliac vein occlusion: midterm results of endovascular recanalization. J Endovasc Ther. 2009. 16:483–491.15. See-Tho K, Harris EJ Jr. Thrombosis with outflow obstruction delays thrombolysis and results in chronic wall thickening of rat veins. J Vasc Surg. 1998. 28:115–122.16. Gogalniceanu P, Johnston CJ, Khalid U, Holt PJ, Hincliffe R, Loftus IM, et al. Indications for thrombolysis in deep venous thrombosis. Eur J Vasc Endovasc Surg. 2009. 38:192–198.17. Beygui RE, Olcott C 4th, Dalman RL. Subclavian vein thrombosis: outcome analysis based on etiology and modality of treatment. Ann Vasc Surg. 1997. 11:247–255.18. Kim HS, Patra A, Paxton BE, Khan J, Streiff MB. Catheter-directed thrombolysis with percutaneous rheolytic thrombectomy versus thrombolysis alone in upper and lower extremity deep vein thrombosis. Cardiovasc Intervent Radiol. 2006. 29:1003–1007.19. Vedantham S, Vesely TM, Sicard GA, Brown D, Rubin B, Sanchez LA, et al. Pharmacomechanical thrombolysis and early stent placement for iliofemoral deep vein thrombosis. J Vasc Interv Radiol. 2004. 15:565–574.20. Jackson LS, Wang XJ, Dudrick SJ, Gersten GD. Catheter-directed thrombolysis and/or thrombectomy with selective endovascular stenting as alternatives to systemic anticoagulation for treatment of acute deep vein thrombosis. Am J Surg. 2005. 190:864–868.21. Kwak HS, Han YM, Lee YS, Jin GY, Chung GH. Stents in common iliac vein obstruction with acute ipsilateral deep venous thrombosis: early and late results. J Vasc Interv Radiol. 2005. 16:815–822.22. Bjarnason H, Kruse JR, Asinger DA, Nazarian GK, Dietz CA Jr, Caldwell MD, et al. Iliofemoral deep venous thrombosis: safety and efficacy outcome during 5 years of catheter-directed thrombolytic therapy. J Vasc Interv Radiol. 1997. 8:405–418.23. Ouriel K, Gray B, Clair DG, Olin J. Complications associated with the use of urokinase and recombinant tissue plasminogen activator for catheter-directed peripheral arterial and venous thrombolysis. J Vasc Interv Radiol. 2000. 11:295–298.24. Alesh I, Kayali F, Stein PD. Catheter-directed thrombolysis (intrathrombus injection) in treatment of deep venous thrombosis: a systematic review. Catheter Cardiovasc Interv. 2007. 70:143–148.25. Segal JB, Streiff MB, Hofmann LV, Thornton K, Bass EB. Management of venous thromboembolism: a systematic review for a practice guideline. Ann Intern Med. 2007. 146:211–222.26. Kahn SR, Solymoss S, Lamping DL, Abenhaim L. Long-term outcomes after deep vein thrombosis: postphlebitic syndrome and quality of life. J Gen Intern Med. 2000. 15:425–429.27. Kahn SR, Ginsberg JS. Relationship between deep venous thrombosis and the postthrombotic syndrome. Arch Intern Med. 2004. 164:17–26.28. Kahn SR. The post-thrombotic syndrome: the forgotten morbidity of deep venous thrombosis. J Thromb Thrombolysis. 2006. 21:41–48.29. Markel A, Manzo RA, Bergelin RO, Strandness DE Jr. Valvular reflux after deep vein thrombosis: incidence and time of occurrence. J Vasc Surg. 1992. 15:377–382.30. Cho JS, Martelli E, Mozes G, Miller VM, Gloviczki P. Effects of thrombolysis and venous thrombectomy on valvular competence, thrombogenicity, venous wall morphology, and function. J Vasc Surg. 1998. 28:787–799.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catheter-directed Thrombolysis of Below-Knee Deep Venous Thrombosis of the Lower Extremities
- Short-Term Catheter-Directed Thrombolysis with Low-Dose Urokinase Followed by Aspiration Thrombectomy for Treatment of Symptomatic Lower Extremity Deep Venous Thrombosis
- Intra-Arterial Thrombolysis for Deep Vein Thrombosis of the Lower Extremity: Case Report
- Deep Venous Thrombosis in the Lower Extremity: Catheter-Directed Thrombolysis
- Treatment of Deep Venous Thromboses of Lower Leg with Thrombolysis