Korean J Ophthalmol.
2010 Aug;24(4):252-255. 10.3341/kjo.2010.24.4.252.
Neovascular Glaucoma Following Stereotactic Radiosurgery for an Optic Nerve Glioma: A Case Report
- Affiliations
-
- 1Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, The Catholic University of Korea School of Medicine, Seoul, Korea. ckpark@catholic.ac.kr
- KMID: 949066
- DOI: http://doi.org/10.3341/kjo.2010.24.4.252
Abstract
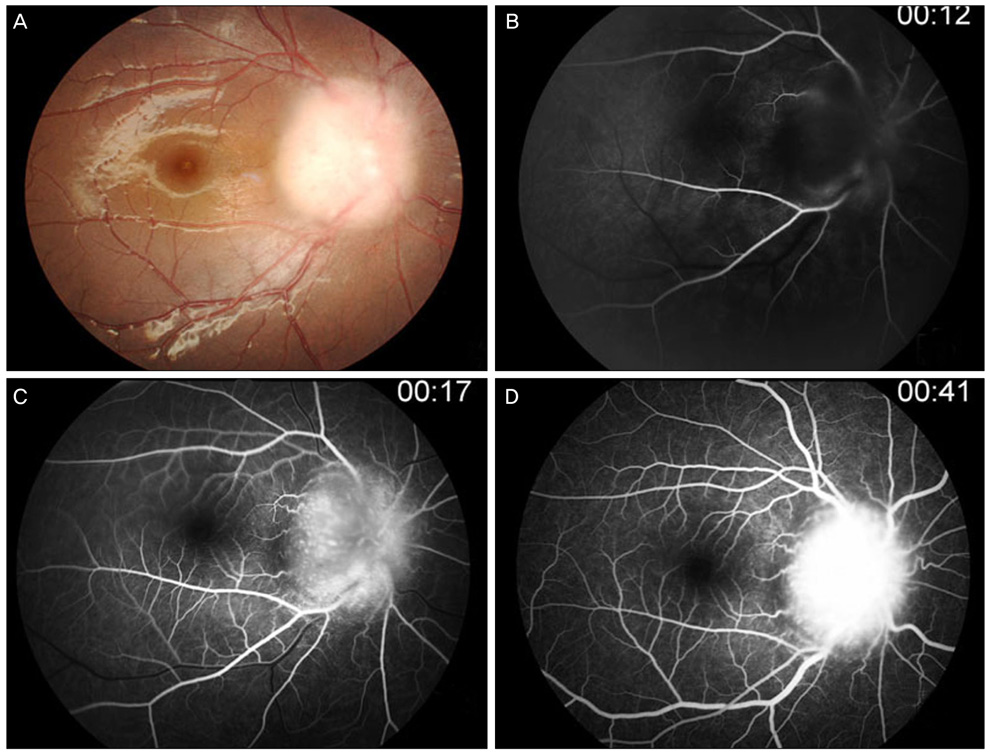
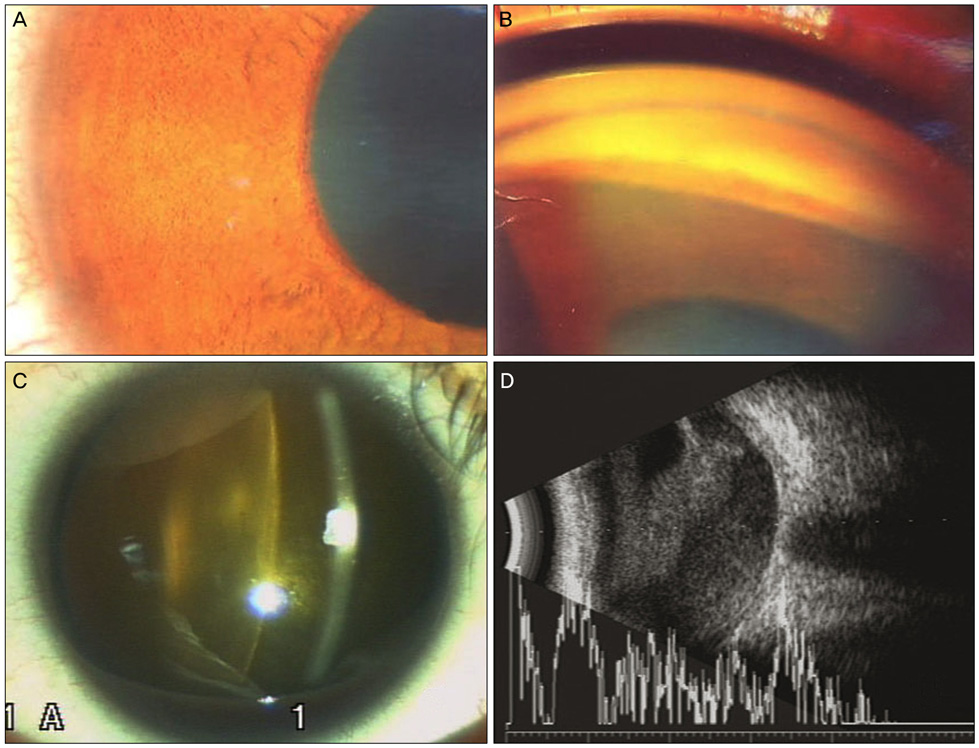
- A 13-year-old girl with a right intraorbital optic nerve glioma (ONG) was referred to our glaucoma clinic because of uncontrolled intraocular pressure (IOP) in her right eye. The IOP reached as high as 80 mmHg. Several months earlier, she had undergone stereotactic image-guided robotic radiosurgery using the CyberKnife for her ONG; the mass had become smaller after treatment. Her visual acuity was no light perception. Slit lamp examination revealed rubeosis iridis, a swollen pale optic disc, and vitreous hemorrhage. After medical treatment, the IOP decreased to 34 mmHg, and no pain was reported. Although the mass effect of an ONG can cause neovascular glaucoma (NVG), this case shows that stereotactic radiosurgery may also cause NVG, even after reducing the mass of the tumor. Patients who undergo radiosurgery targeting the periocular area should be followed carefully for complications.
MeSH Terms
-
Adolescent
Diagnosis, Differential
Female
Fluorescein Angiography
Follow-Up Studies
Fundus Oculi
Glaucoma, Neovascular/diagnosis/*etiology/physiopathology
Glioma/diagnosis/*surgery
Gonioscopy
Humans
Intraocular Pressure
Magnetic Resonance Imaging
Optic Nerve Neoplasms/diagnosis/*surgery
Radiosurgery/*adverse effects
Figure
Reference
-
1. Charles NC, Nelson L, Brookner AR, et al. Pilocytic astrocytoma of the optic nerve with hemorrhage and extreme cystic degeneration. Am J Ophthalmol. 1981. 92:691–695.2. Henkind P, Benjamin JV. Vascular anomalies and neoplasms of the optic nerve head. Trans Ophthalmol Soc UK. 1976. 96:418–423.3. Hovland KR, Ellis PP. Hemorrhagic glaucoma with optic nerve glioma. Arch Ophthalmol. 1966. 75:806–809.4. Buchanan TA, Hoyt WF. Optic nerve glioma and neovascular glaucoma: report of a case. Br J Ophthalmol. 1982. 66:96–98.5. Bergman L, Nilsson B, Lundell G, et al. Ruthenium brachytherapy for uveal melanoma, 1979-2003: survival and functional outcomes in the Swedish population. Ophthalmology. 2005. 112:834–840.6. Demaerel P, de Ruyter N, Casteels I, et al. Visual pathway glioma in children treated with chemotherapy. Eur J Paediatr Neurol. 2002. 6:207–212.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiation-Induced Neovascular Glaucoma: Dose and Volume Issues
- A Case of Bilateral Optic Nerve Glioma
- Fractionated Stereotactic Radiosurgery(FSRS) for Sella and Parasella Tumors Adjacent to Optic Apparatus
- Treatment of Compressive Optic Neuropathy by Recurred Maxillary Cancer Using Stereotactic Radiosurgery: A Case Report
- Glioma of the Optic Nerve and Optic Chiasm