Korean J Ophthalmol.
2010 Aug;24(4):213-218. 10.3341/kjo.2010.24.4.213.
Central Photoreceptor Viability and Prediction of Visual Outcome in Patients with Idiopathic Macular Holes
- Affiliations
-
- 1Department of Ophthalmology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. swkang@skku.edu
- 2Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 3Department of Ophthalmology, Chungbuk National University College of Medicine, Cheongju, Korea.
- 4Department of Ophthalmology, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea.
- KMID: 949058
- DOI: http://doi.org/10.3341/kjo.2010.24.4.213
Abstract
- PURPOSE
To identify the correlation between preoperative optical coherence tomography (OCT) features and postoperative visual outcomes in eyes with idiopathic macular holes (MHs).
METHODS
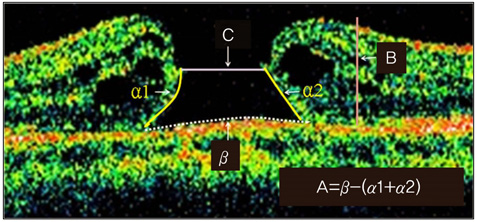
Data from 55 eyes with idiopathic MHs which had been sealed by vitrectomy were retrospectively reviewed. Correlation analysis was conducted between postoperative visual acuity (V(postop), logarithm of the minimum angle of resolution [logMAR]) and preoperative factors, including four OCT parameters: the anticipated length (A) devoid of photoreceptors after hole closure, MH height (B), MH size (C), and the grading (D) of the viability of detached photoreceptors. Additionally, the formula for the prediction of visual outcome was deduced.
RESULTS
V(postop) was determined to be significantly correlated with the preoperative visual acuity (V(preop)) and OCT parameters A, C, and D (p<0.001). Based on the correlation, the formula for the prediction of V(postop) was derived from the most accurate regression analysis: V(postop)=0.248xV(preop)+1.1x10(-6)xA(2)-0.121xD+0.19.
CONCLUSIONS
The length and viability of detached photoreceptors are significant preoperative OCT features for predicting visual prognosis. This suggests that, regardless of the MH size and symptom duration, active surgical intervention should be encouraged, particularly if the MH exhibits good viability in the detached photoreceptor layer.
MeSH Terms
Figure
Reference
-
1. Sjaarda RN, Thompson JT. Ryan SJ, Wilkinson CP, editors. Macular hole. Retina. 2006. Vol. 3, Surgical retina:4th ed. Philadelphia: Elsevier;2527–2542.2. Smiddy WE, Feuer W, Cordahi G. Internal limiting membrane peeling in macular hole surgery. Ophthalmology. 2001. 108:1471–1476.3. Freeman WR, Azen SP, Kim JW, et al. The Vitrectomy for Treatment of Macular Hole Study Group. Vitrectomy for the treatment of full-thickness stage 3 or 4 macular holes: results of a multicentered randomized clinical trial. Arch Ophthalmol. 1997. 115:11–21.4. Mester V, Kuhn F. Internal limiting membrane removal in the management of full-thickness macular holes. Am J Ophthalmol. 2000. 129:769–777.5. Smiddy WE, Pimentel S, Williams GA. Macular hole surgery without using adjunctive additives. Ophthalmic Surg Lasers. 1997. 28:713–717.6. Kasuga Y, Arai J, Akimoto M, Yoshimura N. Optical coherence tomograghy to confirm early closure of macular holes. Am J Ophthalmol. 2000. 130:675–676.7. Brooks HL Jr. Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology. 2000. 107:1939–1948.8. Lai MM, Williams GA. Anatomical and visual outcomes of idiopathic macular hole surgery with internal limiting membrane removal using low-concentration indocyanine green. Retina. 2007. 27:477–482.9. Banker AS, Freeman WR, Azen SP, Lai MY. A multicentered clinical study of serum as adjuvant therapy for surgical treatment of macular holes: Vitrectomy for Macular Hole Study Group. Arch Ophthalmol. 1999. 117:1499–1502.10. Cheng L, Azen SP, El-Bradey MH, et al. Effects of preoperative and postoperative epiretinal membranes on macular hole closure and visual restoration. Ophthalmology. 2002. 109:1514–1520.11. Ullrich S, Haritoglou C, Gass C, et al. Macular hole size as a prognostic factor in macular hole surgery. Br J Ophthalmol. 2002. 86:390–393.12. Haritoglou C, Neubauer AS, Reiniger IW, et al. Long-term functional outcome of macular hole surgery correlated to optical coherence tomography measurements. Clin Experiment Ophthalmol. 2007. 35:208–213.13. Uemoto R, Yamamoto S, Aoki T, et al. Macular configuration determined by optical coherence tomography after idiopathic macular hole surgery with or without internal limiting membrane peeling. Br J Ophthalmol. 2002. 86:1240–1242.14. Villate N, Lee JE, Venkatraman A, Smiddy WE. Photoreceptor layer features in eyes with closed macular holes: optical coherence tomography findings and correlation with visual outcomes. Am J Ophthalmol. 2005. 139:280–289.15. Kang SW, Ahn K, Ham DI. Types of macular hole closure and their clinical implications. Br J Ophthalmol. 2003. 87:1015–1019.16. Guyer DR, Green WR, de Bustros S, Fine SL. Histopathologic features of idiopathic macular holes and cysts. Ophthalmology. 1990. 97:1045–1051.17. Funata M, Wendel RT, de la Cruz Z, Green WR. Clinicopathologic study of bilateral macular holes treated with pars plana vitrectomy and gas tamponade. Retina. 1992. 12:289–298.18. Frangieh GT, Green WR, Engel HM. A histopathologic study of macular cysts and holes. Retina. 1981. 1:311–336.19. Srinivasan VJ, Wojtkowski M, Witkin AJ, et al. High-definition and 3-dimensional imaging of macular pathologies with high-speed ultrahigh-resolution optical coherence tomography. Ophthalmology. 2006. 113:2054.e1–2054.e14.20. Hangai M, Ojima Y, Gotoh N, et al. Three-dimensional imaging of macular holes with high-speed optical coherence tomography. Ophthalmology. 2007. 114:763–773.21. Sjaarda RN, Frank DA, Glaser BM, et al. Resolution of an absolute scotoma and improvement of relative scotomata after successful macular hole surgery. Am J Ophthalmol. 1993. 116:129–139.22. Lee JE, Lee SU, Jea SY, et al. Reorganization of photoreceptor layer on optical coherence tomography concurrent with visual improvement after macular hole surgery. Korean J Ophthalmol. 2008. 22:137–142.23. Kusuhara S, Teraoka Escano MF, Fujii S, et al. Prediction of postoperative visual outcome based on hole configuration by optical coherence tomography in eyes with idiopathic macular holes. Am J Ophthalmol. 2004. 138:709–716.24. Smiddy WE, Glaser BM, Thompson JT, et al. Transforming growth factor-beta 2 significantly enhances the ability to flatten the rim of subretinal fluid surrounding macular holes: preliminary anatomic results of a multicenter prospective randomized study. Retina. 1993. 13:296–301.25. Paques M, Chastang C, Mathis A, et al. Platelets in Macular Hole Surgery Group. Effect of autologous platelet concentrate in surgery for idiopathic macular hole: results of a multicenter, double-masked, randomized trial. Ophthalmology. 1999. 106:932–938.26. Kim SS, Smiddy WE, Feuer WJ, Shi W. Outcomes of sulfur hexafluoride (SF6) versus perfluoropropane (C3F8) gas tamponade for macular hole surgery. Retina. 2008. 28:1408–1415.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of Macular Hole Surgery using Confocal Laser Tomography
- Vitreous Surgery for Macular Hole
- Two years results of surgery for idiopathic macular hole
- Evaluation of Correlation Between OCT Findings and Delayed Visual Acuity Improvement After Macular Hole Surgery
- Reorganization of Photoreceptor Layer on Optical Coherence Tomography Concurrent with Visual Improvement after Macular Hole Surgery