Korean J Gastroenterol.
2010 Sep;56(3):186-191. 10.4166/kjg.2010.56.3.186.
Portal Hypertensive Gastropathy and Gastric Antral Vascular Ectasia
- Affiliations
-
- 1Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea. 20050101@kuh.ac.kr
- KMID: 948780
- DOI: http://doi.org/10.4166/kjg.2010.56.3.186
Abstract
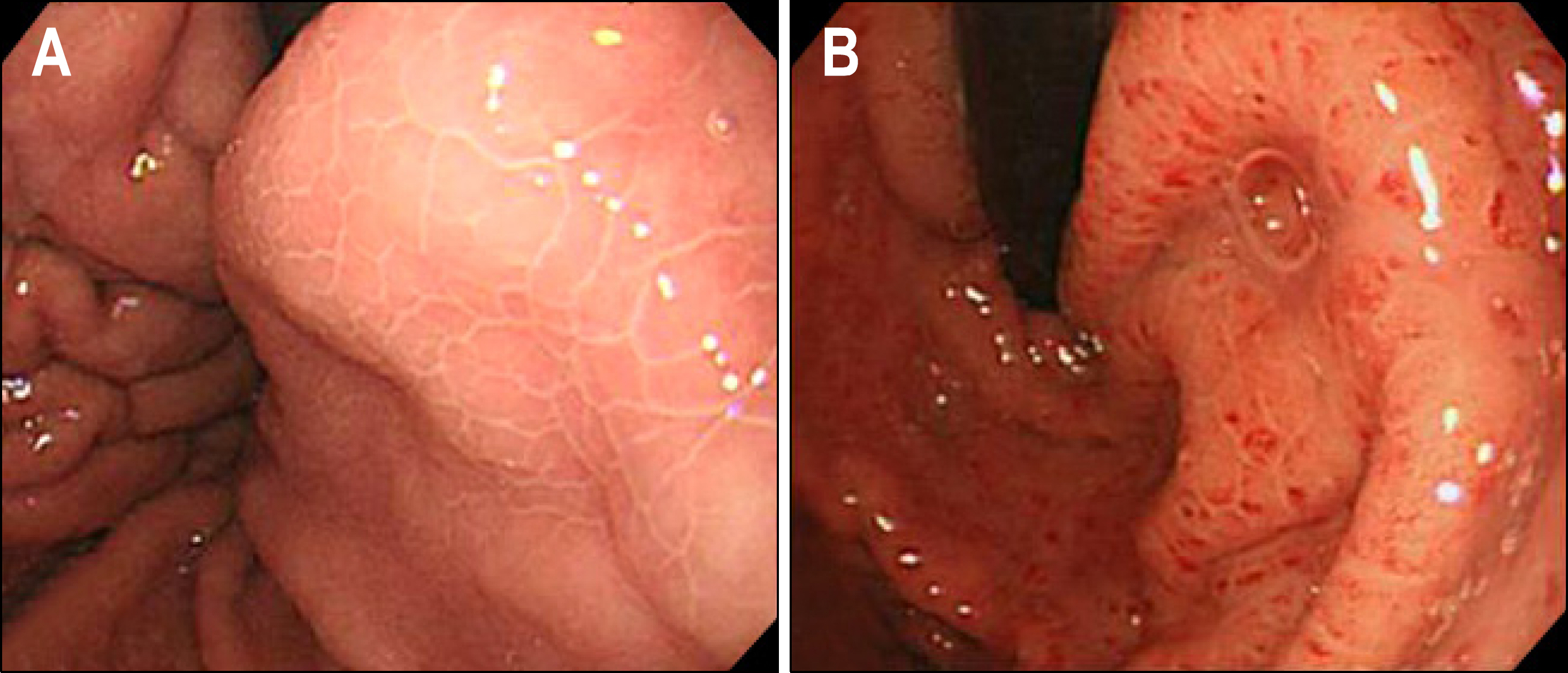
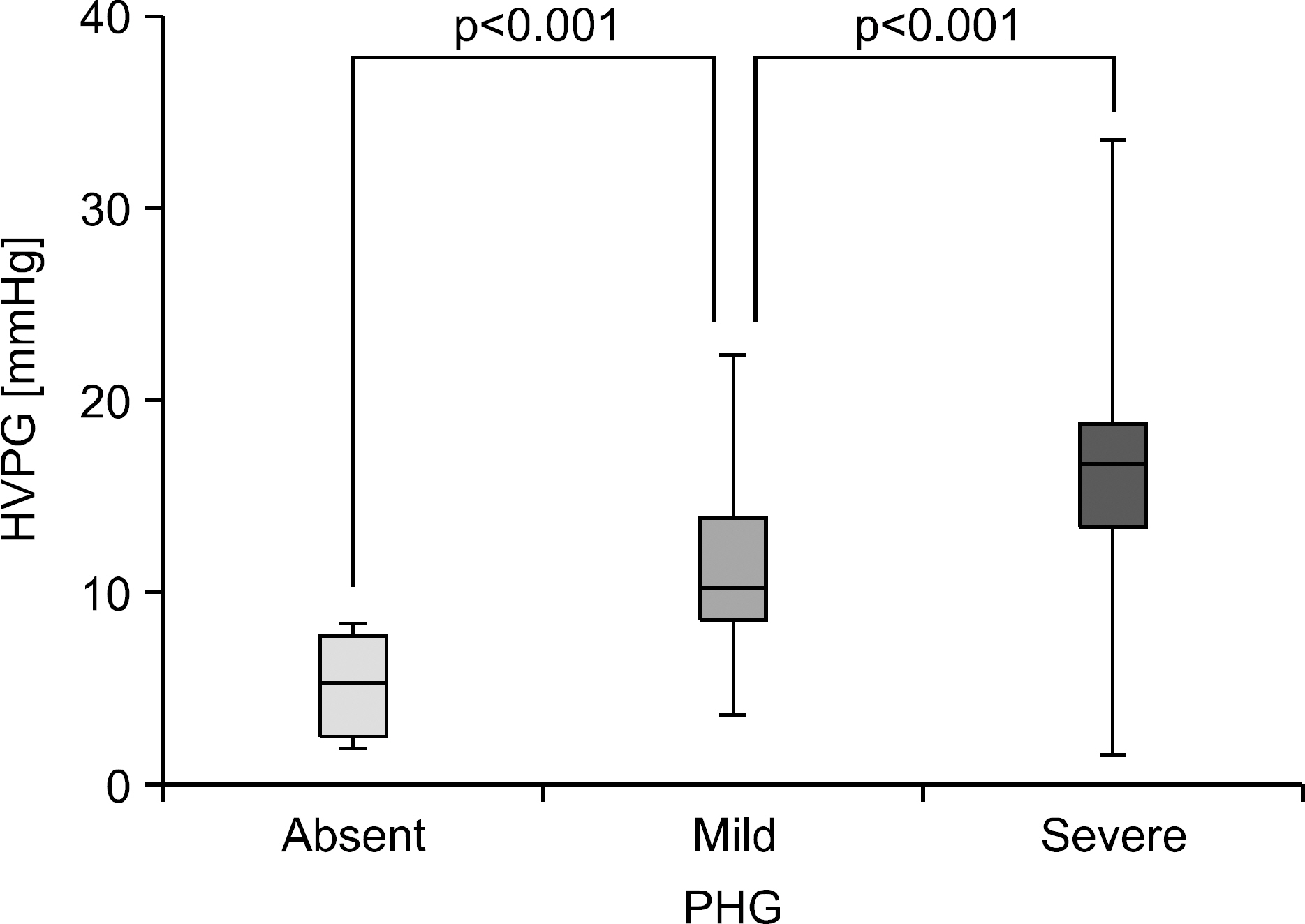
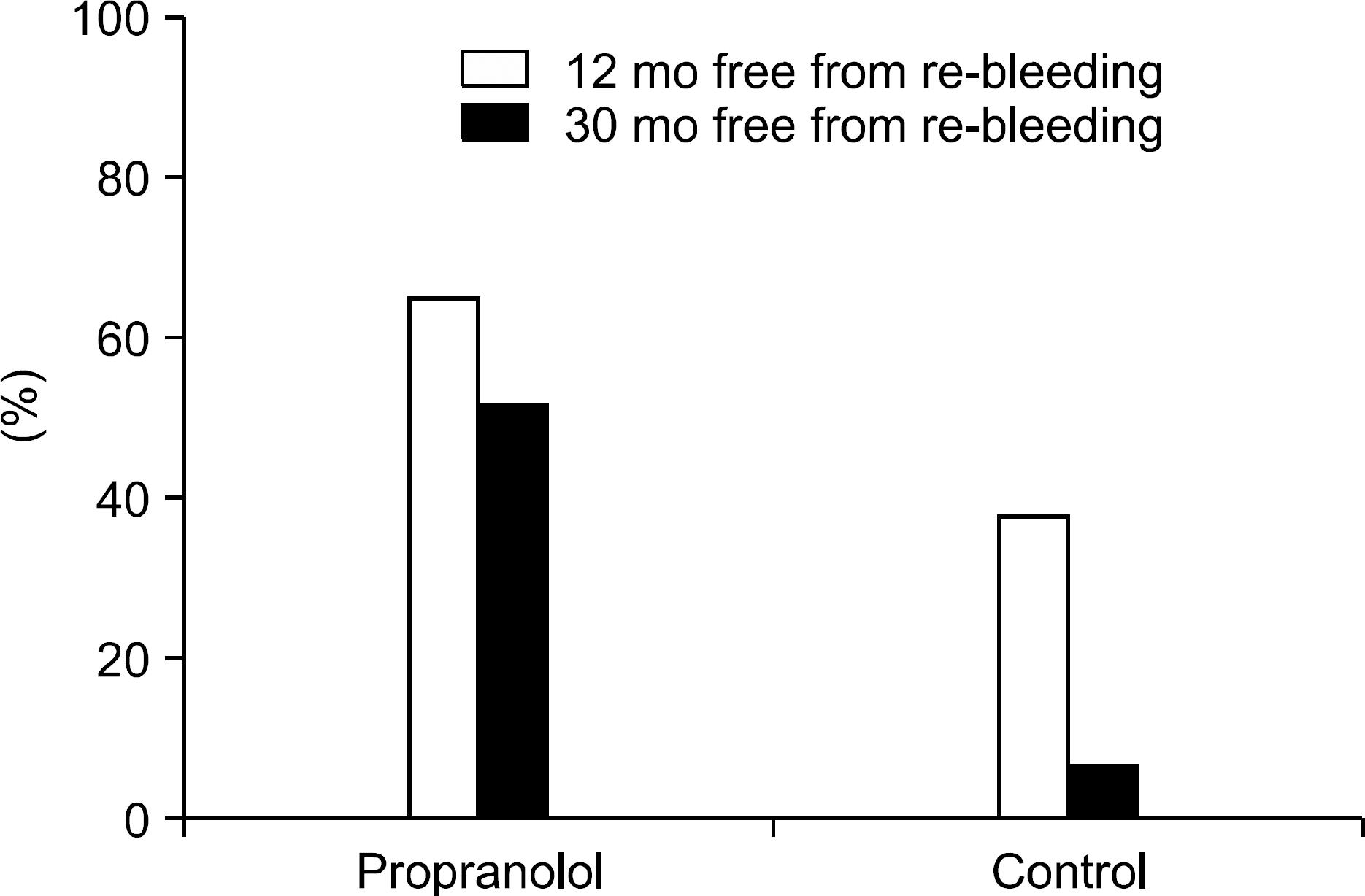
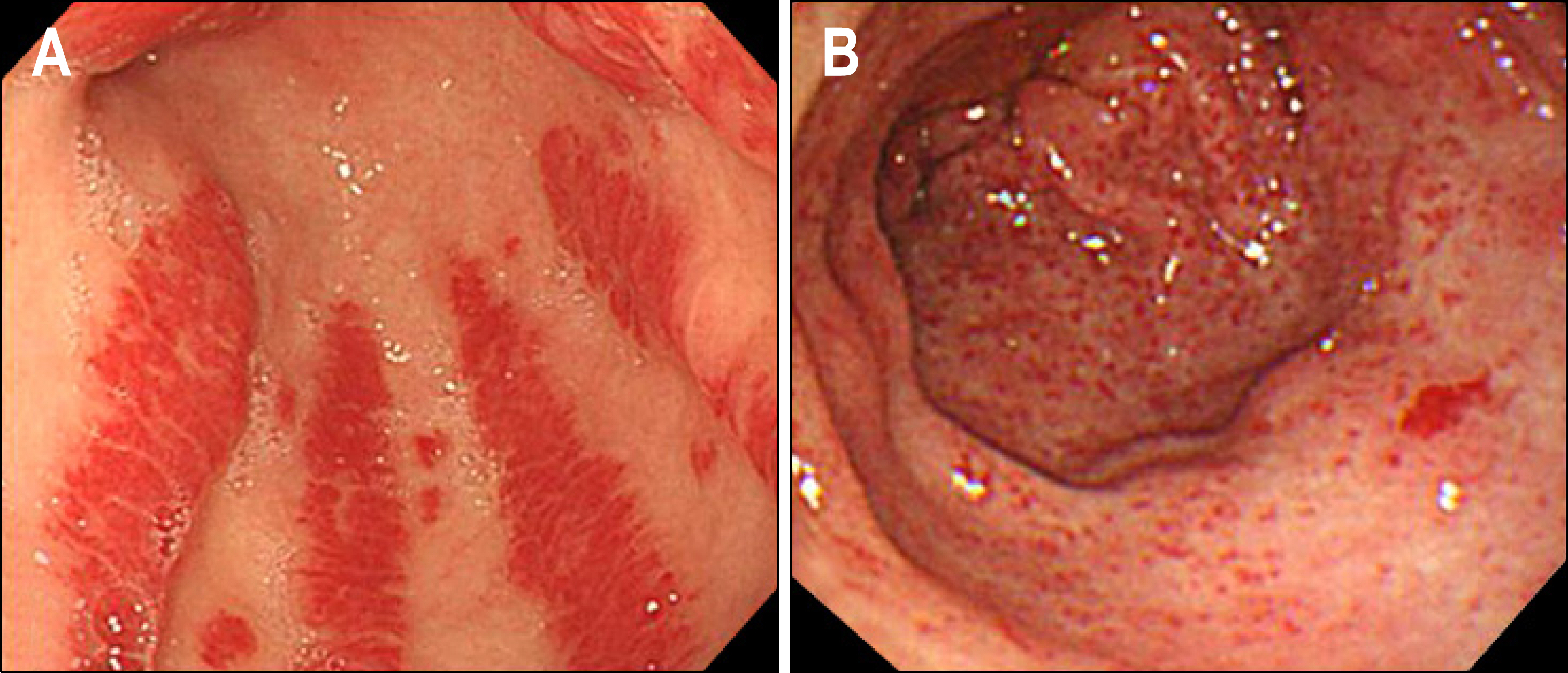
- Portal hypertensive gastropathy (PHG) is a term used to define the endoscopic findings of gastric mucosa with a characteristic mosaic-like pattern with or without red spots, and a common finding in patients with portal hypertension. These endoscopic findings correspond to dilated mucosal capillaries without inflammation. The pathogenesis of PHG in not well known, but portal hypertension and some humoral factors seem to be crucial factors for its development. Pharmacological (e.g. propranolol), or interventional radiological (such as transjugular intrahepatic portosystemic shunt) procedures may be useful in preventing re-bleeding from PHG. The classic features of gastric antral vascular ectasia (GAVE) syndrome include red, often haemorrhagic lesions predominantly located in the gastric antrum which can result in significant blood loss. Although the pathogenesis of GAVE is not clearly defined, it seems to be a separate disease entity from PHG, because GAVE generally does not respond to a reduction of portal pressures. Endoscopic ablation (such as argon plasma coagulation) is the first-line treatment of choice. This review will focus on the incidence, clinical importance, etiology, pathophysiology, and treatment of PHG and GAVE syndrome in the setting of portal hypertension.
Keyword
MeSH Terms
Figure
Reference
-
1. Ripoll C, Garcia-Tsao G. Management of gastropathy and gastric vascular ectasia in portal hypertension. Clin Liver Dis. 2010; 14:281–295.
Article2. Perini RF, Camara PR, Ferraz JG. Pathogenesis of portal hypertensive gastropathy: translating basic research into clinical practice. Nat Clin Pract Gastroenterol Hepatol. 2009; 6:150–158.
Article3. Thuluvath PJ, Yoo HY. Portal Hypertensive gastropathy. Am J Gastroenterol. 2002; 97:2973–2978.
Article4. Burak KW, Lee SS, Beck PL. Portal hypertensive gastropathy and gastric antral vascular ectasia (GAVE) syndrome. Gut. 2001; 49:866–872.
Article5. Kim MY, Choi H, Baik SK, et al. Portal hypertensive gastropathy: correlation with portal hypertension and prognosis in cirrhosis. Dig Dis Sci. 2010. [Epub ahead of print].
Article6. Dră ghia AC. Histochemical and histopathological study of the gastric mucosa in the portal hypertensive gastropathy. Rom J Morphol Embryol. 2006; 47:259–262.7. de Franchis R. Updating consensus in portal hypertension: report of the Baveno III Consensus Workshop on definitions, methodology and therapeutic strategies in portal hypertension. J Hepatol. 2000; 33:846–852.8. Burak KW, Beck PL. Diagnosis of portal hypertensive gastropathy. Curr Opin Gastroenterol. 2003; 19:477–482.
Article9. Bellis L, Nicodemo S, Galossi A, et al. Hepatic venous pressure gradient does not correlate with the presence and the severity of portal hypertensive gastropathy in patients with liver cirrhosis. J Gastrointestin Liver Dis. 2007; 16:273–277.10. Kinjo N, Kawanaka H, Akahoshi T, et al. Significance of ERK nitration in portal hypertensive gastropathy and its therapeutic implications. Am J Physiol Gastrointest Liver Physiol. 2008; 295:G1016–G1024.
Article11. Zullo A, Hassan C, Morini S. Helicobacter pylori infection in patients with liver cirrhosis: facts and fictions. Dig Liver Dis. 2003; 35:197–205.
Article12. Kim TU, Kim S, Woo SK, et al. Dynamic CT of portal hypertensive gastropathy: significance of transient gastric perfusion defect sign. Clin Radiol. 2008; 63:783–790.
Article13. Primignani M, Carpinelli L, Preatoni P, et al. Natural history of portal hypertensive gastropathy in patients with liver cirrhosis. The New Italian Endoscopic Club for the study and treatment of esophageal varices (NIEC). Gastroenterology. 2000; 119:181–187.14. Zhou Y, Qiao L, Wu J, et al. Comparison of the efficacy of octreotide, vasopressin, and omeprazole in the control of acute bleeding in patients with portal hypertensive gastropathy: a controlled study. J Gastroenterol Hepatol. 2002; 17:973–979.
Article15. Pé rez-Ayuso RM, Piqueé JM, Bosch J, et al. Propranolol in prevention of recurrent bleeding from severe portal hypertensive gastropathy in cirrhosis. Lancet. 1991; 337:1431–1434.16. Baik SK. Pharmacological therapy of portal hypertension–focused on Korean data. Korean J Gastroenterol. 2005; 45:381–386.17. Mezawa S, Homma H, Ohta H, et al. Effect of transjugular intrahepatic portosystemic shunt formation on portal hypertensive gastropathy and gastric circulation. Am J Gastroenterol. 2001; 96:1155–1159.
Article18. Takeuchi Y, Kitano S, Bandoh T, et al. Acceleration of gastric ulcer healing by omeprazole in portal hypertensive rats. Is its action mediated by gastrin release and the stimulation of epithelial proliferation? Eur Surg Res. 2003; 35:75–80.
Article19. Selinger CP, Ang YS. Gastric antral vascular ectasia (GAVE): an update on clinical presentation, pathophysiology and treatment. Digestion. 2008; 77:131–137.
Article20. Sebastian S, O'Morain CA, Buckley MJ. Review article: current therapeutic options for gastric antral vascular ectasia. Aliment Pharmacol Ther. 2003; 18:157–165.21. Spahr L, Villeneuve JP, Dufresne MP, et al. Gastric antral vascular ectasia in cirrhotic patients: absence of relation with portal hypertension. Gut. 1999; 44:739–742.
Article22. Ito M, Uchida Y, Kamano S, et al. Clinical comparisons between two subsets of gastric antral vascular ectasia. Gastrointest Endosc. 2001; 53:764–770.
Article23. Lecleire S, Ben-Soussan E, Antonietti M, et al. Bleeding gastric vascular ectasia treated by argon plasma coagulation: a comparison between patients with and without cirrhosis. Gastrointest Endosc. 2008; 67:219–225.
Article24. Ward EM, Raimondo M, Rosser BG, et al. Prevalence and natural history of gastric antral vascular ectasia in patients undergoing orthotopic liver transplantation. J Clin Gastroenterol. 2004; 38:898–900.
Article25. Cho S, Zanati S, Yong E, et al. Endoscopic cryotherapy for the management of gastric antral vascular ectasia. Gastrointest Endosc. 2008; 68:895–902.
Article26. Tran A, Villeneuve JP, Bilodeau M, et al. Treatment of chronic bleeding from gastric antral vascular ectasia (GAVE) with estrogen-progesterone in cirrhotic patients: an open pilot study. Am J Gastroenterol. 1999; 94:2909–2911.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Management of portal hypertensive gastropathy and other bleeding
- Radiologic Finding of Gastric Antral Vascular Ectasia: A Case Report
- A case of gastric antral vascular ectasia treated with argon plasma coagulation
- A Case of Watermelon Stomach ( Gastric Antral Vascular Ectasia )
- Elevated Gastric Antrum Erosions in Portal Hypertension Patients: Peptic Disease or Mucosal Congestion?