Korean J Ophthalmol.
2010 Apr;24(2):131-133. 10.3341/kjo.2010.24.2.131.
Case of Bilateral Retinal Neovascularization Associated with Chronic Idiopathic Myelofibrosis
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine and Sensory Organ Research Institute, Seoul National University Medical Research Center, Seoul, Korea. hgonyu@snu.ac.kr
- KMID: 946007
- DOI: http://doi.org/10.3341/kjo.2010.24.2.131
Abstract
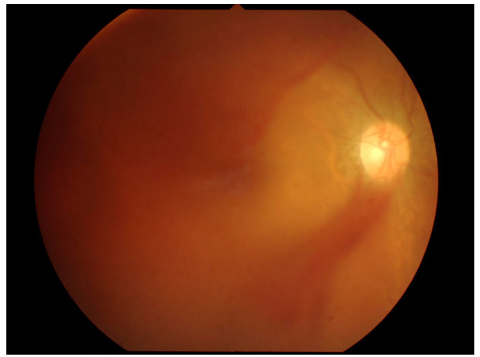
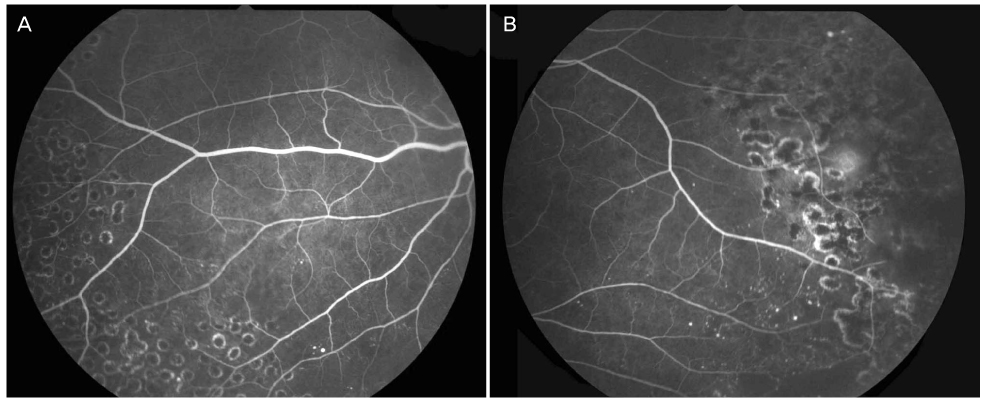
- We report a case of bilateral peripheral retinal neovascularization and chronic idiopathic myelofibrosis in a 69-year-old man. Ophthalmic examination revealed peripheral retinal nonperfusion with retinal neovascularization in both eyes and vitreous hemorrhage in the right eye. Fluorescein angiography of both eyes showed a marked midperipheral and peripheral avascular retina temporally with arteriovenous anastomosis and sea-fan neovascularizations. Blood tests showed pancytopenia and teardrop-shaped red blood cells, and bone marrow examination showed hypocellular marrow with severe fibrosis. The neovascularization was regressed following pars plana vitrectomy in the right eye and scatter laser photocoagulation in the left. The results suggest that peripheral retinal vessel occlusion and neovascularization may be associated with idiopathic myelofibrosis.
Keyword
MeSH Terms
Figure
Reference
-
1. Tefferi A. Myelofibrosis with myeloid metaplasia. N Engl J Med. 2000. 342:1255–1265.2. Haskes C, Gagnon K. Retinal manifestations of idiopathic myelofibrosis, a hematologic disorder. J Am Optom Assoc. 1998. 69:319–328.3. Morse PH, McCready JL. Peripheral retinal neovascularization in chronic myelocytic leukemia. Am J Ophthalmol. 1971. 72:975–978.4. Dhaliwal RS, Schachat AP. Ryan SJ, Hinton DR, Schachat AP, Wilkinson CP, editors. Leukemias and lymphomas. Retina. 2006. 4th ed. Philadelphia: Mosby;855.5. Leveille AS, Morse PH. Platelet-induced retinal neovascularization in leukemia. Am J Ophthalmol. 1981. 91:640–644.6. Ahmed A, Chang CC. Chronic idiopathic myelofibrosis: clinicopathologic features, pathogenesis and prognosis. Arch Pathol Lab Med. 2006. 130:1133–1143.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Cases of Myelofibrosis Mimicking Malignant Lymphoma in Computed Tomography of Abdomen: A Case of Autoimmune Myelofibrosis associated with Systemic Lupus Erythematosus Showing Extensive Lymphadenopathy and A Case of Chronic Idiopathic Myelofibrosis wit
- Clinical observation of the bilateral branch vein occlusion
- A Case of Idiopathic Choroidal Neovascularization
- Pyoderma Gangrenosum Associated with Idiopathic Myelofibrosis
- Cutaneous Extramedullary Hematopoiesis in Idiopathic Myelofibrosis