Korean J Lab Med.
2008 Aug;28(4):251-257. 10.3343/kjlm.2008.28.4.251.
Incidence of Aspirin Resistance in the Patient Group of a University Hospital in Korea
- Affiliations
-
- 1Department of Laboratory Medicine, Hallym University College of Medicine, Chuncheon, Korea. lyoungk@hallym.or.kr
- KMID: 854885
- DOI: http://doi.org/10.3343/kjlm.2008.28.4.251
Abstract
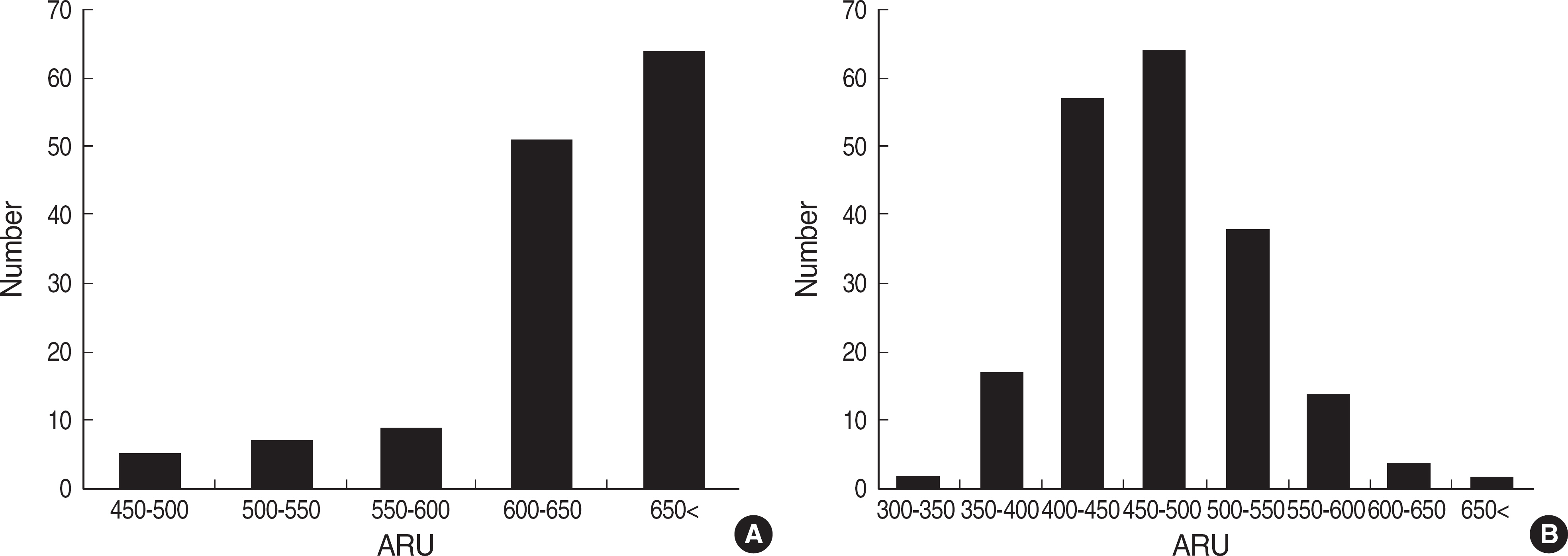
- BACKGROUND: Aspirin is the most common drug used for the prevention of arterial thrombosis. However, platelet responsiveness to aspirin is variable among individuals and it is important to detect aspirin resistance to improve clinical outcome. We analyzed the changes of platelet reactivity before and after aspirin treatment. We also investigated the incidence and influencing factors of aspirin resistance in Korean. METHODS: We tested platelet function in 198 patients who had been treated with aspirin in a Korean university hospital, and 59 of these patients were tested for platelet function before and after aspirin treatment. We also analyzed platelet reactivity in 136 patients who had not been treated with aspirin. Platelet function was tested using the VerifyNow Aspirin Assay (Accumetrics, USA). Platelet reactivity was expressed as aspirin reaction unit (ARU) and > or =550 ARU was defined as aspirin resistance. RESULTS: Platelet reactivity of 136 patients who had not been treated with aspirin was 632.2+/-46.3 ARU (mean+/-SD) (range, 462-675). Platelet reactivity of 198 patients who had been treated with aspirin was 472.5+/-60.0 (338-666) ARU, and 10.1% of patients were aspirin-resistant. The difference of platelet reactivity before and after aspirin treatment was 128.3+/-68.7 (-40-248) ARU. Hb level was lower and platelet count was higher in aspirin-resistant group than in aspirin-sensitive group (P<0.05). CONCLUSIONS: We demonstrated the distribution of platelet reactivity before and after aspirin treatment using the VerifyNow Aspirin Assay. The incidence of aspirin resistance was 10.1%, and low Hb level and high platelet count were related with aspirin resistance.
MeSH Terms
Figure
Cited by 1 articles
-
Aspirin in the prevention of cardiovascular disease and cancer
Yu-Jin Paek, Jong-Lull Yoon
J Korean Med Assoc. 2014;57(4):348-356. doi: 10.5124/jkma.2014.57.4.348.
Reference
-
1.Grotemeyer KH. Effects of acetylsalicylic acid in stroke patients. Evidence of nonresponders in a subpopulation of treated patients. Thromb Res. 1991. 63:587–93.
Article2.Gum PA., Kottke-Marchant K., Poggio ED., Gurm H., Welsh PA., Brooks L, et al. Profile and prevalence of aspirin resistance in patients with cardiovascular disease. Am J Cardiol. 2001. 88:230–5.
Article3.Gum PA., Kottke-Marchant K., Welsh PA., White J., Topol EJ. A prospective, blinded determination of the natural history of aspirin resistance among stable patients with cardiovascular disease. J Am Coll Cardiol. 2003. 41:961–5.
Article4.Andersen K., Hurlen M., Arnesen H., Seljeflot I. Aspirin non-responsiveness as measured by PFA-100 in patients with coronary artery disease. Thromb Res. 2002. 108:37–42.
Article5.Wang JC., Aucoin-Barry D., Manuelian D., Monobouquette R., Reisman M., Gray W, et al. Incidence of aspirin nonresponsiveness using the Ultegra Rapid Platelet Function Assay-ASA. Am J Cardiol. 2003. 92:1492–4.
Article6.Mirkhel A., Peyster E., Sundeen J., Greene L., Michelson AD., Hasan A, et al. Frequency of aspirin resistance in a community hospital. Am J Cardiol. 2006. 98:577–9.
Article7.Dyszkiewicz-Korpanty AM., Kim A., Burner JD., Frenkel EP., Sarode R. Comparison of a rapid platelet function assay–Verify Now Aspirin–with whole blood impedance aggregometry for the detection of aspirin resistance. Thromb Res. 2007. 120:485–8.8.Fontana P., Reber G., de Moerloose P. Assessing aspirin responsiveness using the Verify Now Aspirin assay. Thromb Res. 2008. 121:581–2.
Article9.McGlasson DL., Fritsma GA. Comparison of four laboratory methods to assess aspirin sensitivity. Blood Coagul Fibrinolysis. 2008. 19:120–3.
Article10.Cattaneo M. Laboratory detection of ‘aspirin resistance’: what test should we use (if any)? Eur Heart J. 2007. 28:1673–5.
Article11.Harrison P., Keeling D. Clinical tests of platelet function. Michelson AD, editor. Platelets. 2nd ed.California: Academic Press;2007. p. 445–74.
Article12.Bruno A., McConnel JP., Cohen SN., Tietjen GE., Wallis RA., Goreliek PB, et al. Serial urinary 11-dehydrothromboxane B2, aspirin dose, and vascular events in blacks after recent cerebral infarction. Stroke. 2004. 35:727–30.
Article13.Harrison P., Segal H., Silver L., Syed A., Cuthbertson FC., Rothwell PM. Lack of reproducibility of assessment of aspirin responsiveness by optical aggregometry and two platelet function tests. Platelets. 2008. 19:119–24.
Article14.Lordkipanidze M., Pharand C., Schampaert E., Turgeon J., Palisaitis DA., Diodati JG. A comparison of six major platelet function tests to determine the prevalence of aspirin resistance in patients with stable coronary artery disease. Eur Heart J. 2007. 28:1702–8.
Article15.Malinin A., Spergling M., Muhlestein B., Steinhubl S., Serebruany V. Assessing aspirin responsiveness in subjects with multiple risk factors for vascular disease with a rapid platelet function analyzer. Blood Coagul Fibrinolysis. 2004. 15:295–301.
Article16.Dichiara J., Bliden KP., Tantry US., Chaganti SK., Kreutz RP., Gesheff TB, et al. Platelet function measured by VerifyNow identifies generalized high platelet reactivity in aspirin treated patients. Platelets. 2007. 18:414–23.
Article17.Alberts MJ., Bergman DL., Molner E., Jovanovic BD., Ushiwata I., Teruya J. Antiplatelet effect of aspirin in patients with cerebrovascular disease. Stroke. 2004. 35:175–8.
Article18.George JN., Shattil SJ. Acquired disorders of platelet function. Hoffman R, Benz Jr EJ, editors. Hematology: Basic principles and practice. 3rd ed.New York: Churchill Livingstone;2000. p. 2172–86.19.Lee PY., Chen WH., Ng W., Cheng X., Kwok JY., Tse HF, et al. Low-dose aspirin increases aspirin resistance in patients with coronary artery disease. Am J Med. 2005. 118:723–7.
Article20.Lev EI., Patel RT., Maresh KJ., Guthikonda S., Granada J., DeLao T, et al. Aspirin and clopidogrel drug response in patients undergoing percutaneous coronary intervention: the role of dual drug resistance. J Am Coll Cardiol. 2006. 47:27–33.21.Cambria-Kiely JA., Gandhi PJ. Possible mechanisms of aspirin resistance. J Thromb Thrombolysis. 2002. 13:49–56.22.Santos MT., Valles J., Aznar J., Marcus AJ., Broekman MJ., Safier LB. Prothrombotic effects of erythrocytes on platelet reactivity. Reduction by aspirin. Circulation. 1997. 95:63–8.23.Rinaldi MJ., Kirtane AJ., Piana RN., Caputo RP., Gordon PC., Lopez JJ, et al. Clinical, procedural, and pharmacologic correlates of acute and subacute stent thrombosis: results of a multicenter case-control study with 145 thrombosis events. Am Heart J. 2008. 155:654–60.
Article24.Zakai NA., Wright J., Cushman M. Risk factors for venous thrombosis in medical inpatients: validation of a thrombosis risk score. J Thromb Haemost. 2004. 2:2156–61.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implication of aspirin resistance: Simple laboratory finding or important clinical criteria?
- Aspirin Resistance in Patients with End-Stage Renal Disease
- Effect of Premedication Method and Drug Resistance of Antiplatelet Agent on Periprocedural Thromboembolic Events During Coil Embolization of an Unruptured Intracranial Aneurysm
- Prevalence of aspirin resistance and related factors in patients with type-2 diabetes mellitus
- Aspirin Resistance in Patients Undergoing Dialysis