Korean J Ophthalmol.
2005 Dec;19(4):258-263. 10.3341/kjo.2005.19.4.258.
The Effect of Low-Dose Doxycycline Therapy in Chronic Meibomian Gland Dysfunction
- Affiliations
-
- 1Department of Ophthalmology, Dankook University College of Medicine, Cheonan, Korea. cataract@empal.com
- KMID: 754436
- DOI: http://doi.org/10.3341/kjo.2005.19.4.258
Abstract
- PURPOSE
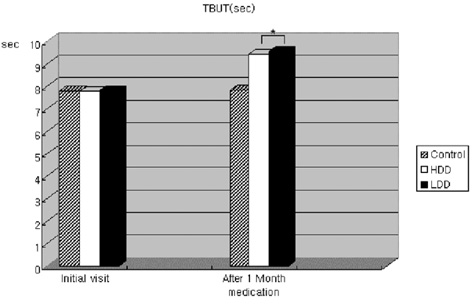
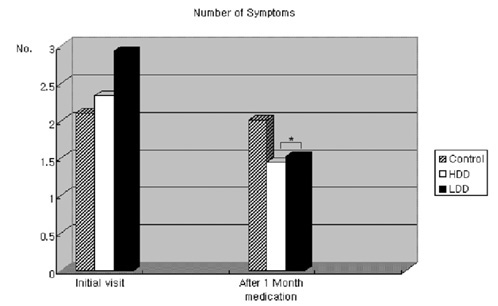
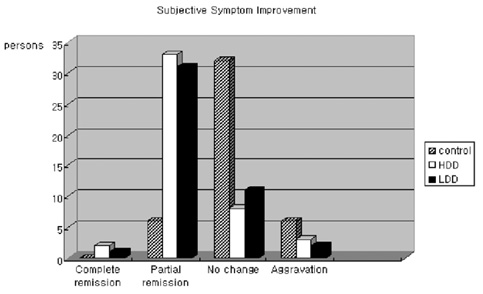
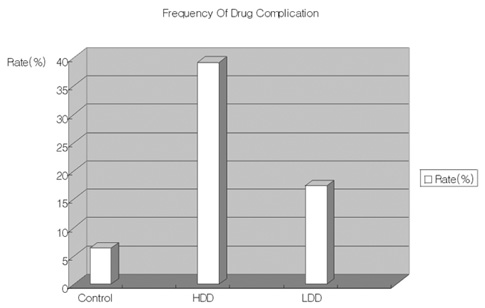
The aim was to investigate the effect of low dose doxycycline (20 mg) therapy in patients with chronic meibomian gland dysfunction that were refractory to conventional therapy. METHODS: The randomized prospective study enrolled 150 patients (300 eyes) who have chronic meibomian gland dysfunction and who didn't respond to lid hygiene and topical therapy for more than 2 months. All topical therapy was stopped for at least 2 weeks prior to beginning the study. After conducting the tear break up time test (TBUT) and Schirmer test, the authors randomly divided the patients into three groups a high dose group (doxycycline, 200 mg, twice a day), a low dose group (doxycycline, 20 mg, twice a day) and a control group (placebo). After one month, the author repeated the TBUT and Schirmer tests, and analyzed the degree of symptomatic improvement. RESULTS: Compared to the control group, both the high and low dose group showed statistically significant differences after treatment in TBUT, Schirmer test, the number of symptoms reported and the degree of improvement of subjective symptoms. However, there was no statistically significant difference between the high and low dose group after treatment in TBUT (9.42+/-2.87 sec, 9.54+/-1.58 sec, p=0.726), Schirmer test (19.98+/-4.05 mm, 19.65+/-5.02 mm, p=0.624), the number of symptoms reported (1.45+/-0.62, 1.53+/-0.52, p=0.304), as well as the degree of improvement of subjective symptoms (p=0.288). The high dose group (18 patients, 39.13%) reported side effects more frequently than did the low dose group (8 patients, 17.39%) (P=0.002). CONCLUSIONS: Low dose doxycycline (20 mg twice a day) therapy was effective in patients with chronic meibomian gland dysfunction that were refractory to conventional therapy.
MeSH Terms
-
Treatment Outcome
Tears/drug effects/secretion
Prospective Studies
Middle Aged
Meibomian Glands/*drug effects
Male
Humans
Follow-Up Studies
Female
Eyelid Diseases/*drug therapy/metabolism
Doxycycline/*administration & dosage/therapeutic use
Dose-Response Relationship, Drug
Chronic Disease
Anti-Bacterial Agents/*administration & dosage/therapeutic use
Administration, Oral
Figure
Reference
-
1. Cho JH, Young A. Assessment of Meibomian gland dysfunction and comparison of the results of BUT and Schirmer test according to meibomian gland state. J Korean Ophthalmol Soc. 2000. 41:1874–1882.2. Smith VA, Cook SD. Doxycycline - a role in ocular surface repair. Br J Ophthalmol. 2004. 88:619–625.3. Preshaw PM, Hefti AF, Jepsen S, et al. Subantimicrobial dose doxycycline as adjunctive treatment for periodontitis. J Clin Periodonta. 2004. 31:697–707.4. Shimazaki J, Skkata M, Tsubota K. Ocular surface changes and discomfort in patients with meibomian gland dysfunction. Arch Ophthalmol. 1995. 113:1266–1270.5. Ahn CS, Ko HJ, Lee SW. The significance of clinical symptoms in dry eye patients and statistical analysis of the patients. J Korean Ophthalmol Soc. 1990. 31:571–577.6. Mathers WD, Shields WJ, Sachdev MS, et al. Meibomian gland morphology and tear osmolarity: change with accutane therapy. Cornea. 1991. 10:286–290.7. Tiffany JM. The role of meibomian secretion in the tears. Trans Ophthalmol Sac UK. 1985. 104:396–401.8. Robin JB, Jester JV, Nobe J, et al. In vivo transillumination biomicroscopy and photography of meibomian gland dysfunction. A clinical study. Ophthalmology. 1985. 92:1423–1426.9. Obata H, Horiuchi H, Miyata K, et al. Histopathological study of the meibomian glands in 72 autopsy cases. Nippon Gank Gaakkai Zasshi. 1994. 98:765–771.10. Gutgesell VJ, Stern GA, Hood Cl. Histopathology of meibomian gland dysfunction. Am J Ophthalmol. 1982. 94:383–387.11. McCulley JP, Shine WE. The lipid layer of tears: dependent on meibomian gland dysfunction. Exp Eye Res. 2004. 78:361–365.12. Zengin N, Tol H, Gunduz K, et al. Meibomian gland dysfunction and tear film abnormalities in rosasea. Cornea. 1995. 14:144–146.13. Glibard JP, Farris RL, Santamaria J 2nd. Osmolarity of tear microvolumnes in keratoconjunctivitis sicca. Arch Ophthalmol. 1978. 96:677–681.14. Goren MB, Goren SB. Diagnostic tests in patients with symptoms of keratoconjunctivitis sicca. Am J Ophthalmol. 1988. 106:570–574.15. Lee JH, Hyun PM. The reproducibility of Schirmer test. J Korean Ophthalmol Soc. 1986. 27:31–35.16. Norn MS. Tear fluid PH in normals, contact lens wearers, and pathological cases. Acta Ophthalmol. 1988. 66:485–489.17. Vanley GT, Leopold IH, Gregg TH. Interpretation of tear film break-up. Arch Ophthalmol. 1977. 95:445–448.18. Lemp MA, Hamill JR. Factors affecting tear film break-up in normal eyes. Arch Ophthalmol. 1973. 89:103–105.19. Lee HB, Rhee SW. Tear Film Break up Time in Normal Korean. J Korean Opthalmol Soc. 1981. 22:729–731.20. Lee JH, Ki CW, Roh KG. The Significance of the Tear Film Break-up Time(BUT) in the Diagnosis of the Dry Eye Syndrome. J Korean Opthalmol Soc. 1985. 26:1131–1135.21. Lucca JA, Nunez JN, Farris RL. A comparison of diagnostic tests for keratoconjunctivitis sicca : latoplate, Schirmer, and tear osmolarity. CLAO J. 1990. 16:109–112.22. Lamberts DW, Foster CS, Perry HD. Schirmer test after topical anesthesia and the tear meniscus in normal eyes. Arch Ophthalmol. 1979. 97:1082–1085.23. Glibard JP, Farris RL. Tear osmolarity and ocular surface disease in keratoconjunctivitis sicca. Arch Ohthalmol. 1979. 97:1642–1646.24. Farris RL, Gilbard JP, Stuchell RN, Mandel ID. Diagnositc test in keratoconjunctivitis sicca. CLAO J. 1983. 9:23–28.25. Golub LM, Ramamurthy NS, McNamara TF, et al. Tetracyclines inhibit connective tissue breakdown : new therapeutic implications for an old family of drugs. Crit Rev Oral Biol Med. 1991. 2:297–322.26. Golub LM, Lee HM, Ryan ME, et al. Tetracyclines inhibit connective tissue breakdown by multiple non-antimicrobial mechanisms. Adv Dent Res. 1998. 12:12–26.27. Thomas J, Walker C, Bradshaw M. Long-term use of subantimicrobial dose doxycycline does not lead to changes in antimicrobial susceptibility. J Periodonto. 2000. 71:1472–1483.28. Walker C, Thomas J, Nango S, et al. Long-term treatment with subantimicrobial dose doxycycline exerts no antibacterial effect on the subgingival microflora associated with adult periodontitis. J Periodontol. 2000. 71:1465–1471.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Meibomian Gland Adenocarcinoma of the Orbit
- Therapeutic Effect of Intense Pulsed Light of Dry Eye with Meibomian Gland Dysfunction
- Assessment of Meibomian Gland Dysfunction and Comparison of The Results of BUT and Schirmer Test According to Meibomian Gland State
- A Case of Meibomian Gland Carcinoma
- Risk Factors of Meibomian Gland Loss in Dry Eye Disease