Korean J Ophthalmol.
2005 Sep;19(3):235-238. 10.3341/kjo.2005.19.3.235.
Subretinal Inflammatory Myofibroblastic Tumor: Clinicopathological Findings
- Affiliations
-
- 1Department of Ophthalmology, Seoul National University College of Medicine, Seoul, Korea. hgonyu@snu.ac.kr
- 2Seoul Artificial Eye Center, Seoul National University Hospital Clinical Research Institute, Seoul, Korea.
- KMID: 754431
- DOI: http://doi.org/10.3341/kjo.2005.19.3.235
Abstract
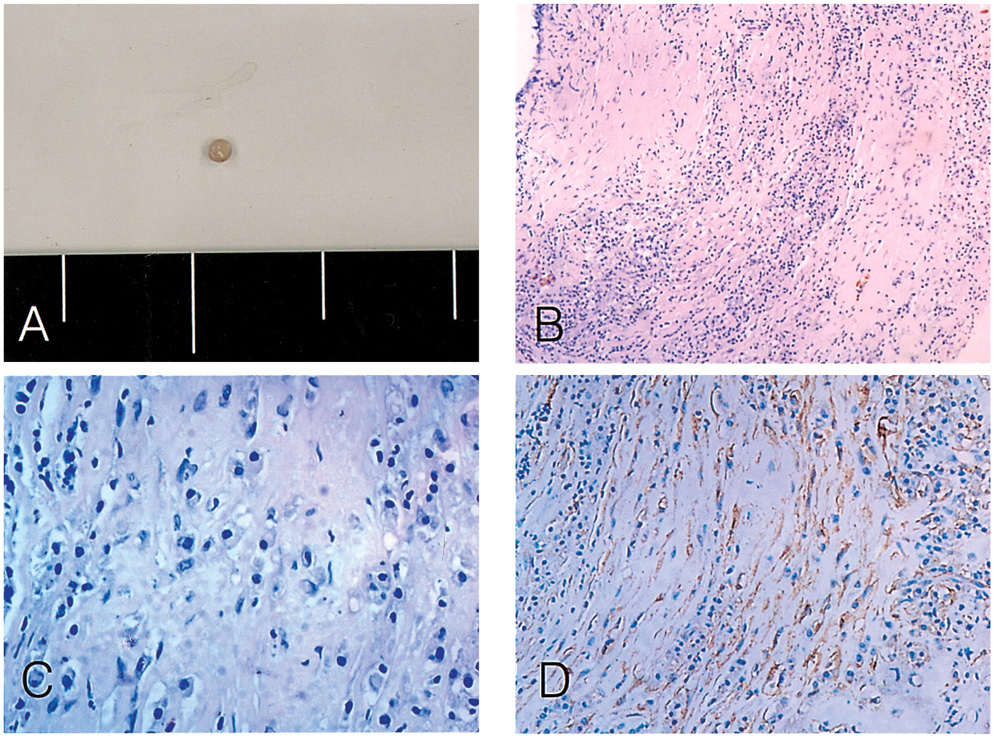
- PURPOSE
To present a case of inflammatory myofibroblastic tumor which was manifested as an idiopathic subretinal mass without underlying pathology. METHODS: The subretinal mass was surgically excised and evaluated histopathologically. Fluorescein angiography and optical coherence tomography were performed pre- and post-operatively. RESULTS: The mass was histologically composed of lymphoplasma cell infiltration and fibrous proliferation without microorganisms or malignant cells. Immunohistochemistry for smooth muscle actin revealed myofibroblasts as a major cellular component. Preoperative optical coherent tomography showed that the lesion was contiguous to the retina while inducing foveal detachment. Postoperatively, the fovea was attached with visual recovery, and the subretinal lesion did not recur during the follow up. CONCLUSIONS: Inflammatory myofibroblastic tumors may be included in the differential diagnoses of subretinal masses.
MeSH Terms
Figure
Reference
-
1. Neuhauser TS, Derringer GA, Thomson LD, et al. Splenic Inflammatory Myofibroblastic Tumor (Inflammatory Pseudotumor): A Clinicopathologic and Immunophenotypic Study of 12 Cases. Arch Pathol Lab Med. 2001. 125:379–385.2. Uy HS, Nguyen QD, Arbour J, et al. Sclerosing inflammatory pseudotumor of the eye. Arch Ophthalmol. 2001. 119:603–607.3. O'Malley DP, Poulos C, Czader M, et al. Intraocular inflammatory myofibroblastic tumor with ALK overexpression. Arch Pathol Lab Med. 2004. 128:e5–e7.4. Bernardino CR, Davidson RS, Maus M, Spaeth GL. Angle-closure glaucoma in association with orbital pseudotumor. Ophthalmology. 2001. 108:1603–1606.5. Heidenkummer HP, Kampik A. Surgical extraction of subretinal pseudotumors in age related macular degeneration. Clinical, morphologic and immunohistochemical results. Ophthalmologe. 1995. 92:631–639.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Inflammatory Myofibroblastic Tumor of Nasal Septum after Septoplasty: A Case Report
- Inflammatory Myofibroblastic Tumor of Kidney
- A Case of Inflammatory Myofibroblastic Tumor of the Maxillary Sinus
- Inflammatory Myofibroblastic Tumor of the Breast: A Case Report
- Inflammatory Myofibroblastic Tumor in Posterior Mediastinum