Korean J Ophthalmol.
2005 Jun;19(2):136-139. 10.3341/kjo.2005.19.2.136.
Change of Stereoacuity with Aging in Normal Eyes
- Affiliations
-
- 1Department of Ophthalmology, Keimyung University School of Medicine, Dongsan Medical Center, Daegu, Korea. lsy3379@dsmc.or.kr
- KMID: 754412
- DOI: http://doi.org/10.3341/kjo.2005.19.2.136
Abstract
- PURPOSE
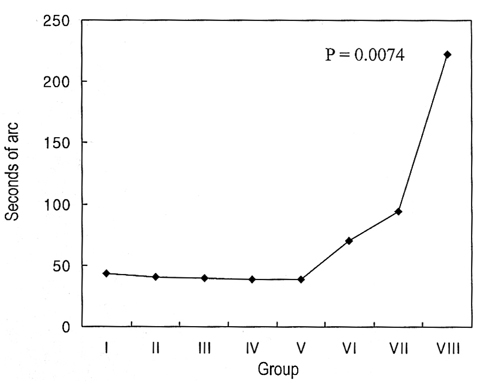
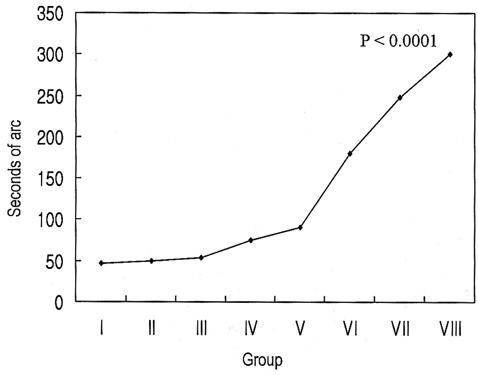
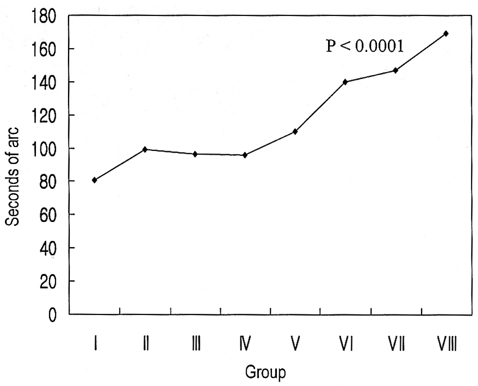
Stereopsis in normal subjects aged between 7 and 76 years was compared to examine changes in stereopsis with age. METHODS: Eighty subjects with no ocular disease were divided into 8 groups by age. Near stereopsis was evaluated with the TNO, Titmus, and Randot tests; distance stereopsis with the Mentor B-VAT II video acuity tester. RESULTS: The results of all 4 tests showed decreased stereopsis with increasing age (p< 0.05). Compared to the stereoacuity of 7 to 10-year-old group, both the TNO and distance stereopsis test results were significantly decreased for the 6th, 7th, and 8th decade groups, while both the Titmus and Randot test results were significantly decreased for the 8th decade group (p< 0.05). CONCLUSIONS: Overall, both near and distance stereopsis decreased with increasing age. Thus, decreased stereopsis should be taken into account when performing the stereopsis test.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Normal Distance Stereoacuity by Age Assessed by the Frisby Davis Distance Stereotest
Sung Jae Kim, Sook Young Kim
J Korean Ophthalmol Soc. 2008;49(1):158-163. doi: 10.3341/jkos.2008.49.1.158.Distance Stereoacuity by Frisby Davis Distance Stereotest after Surgery in Intermittent Exotropic Patients
Kyung Tae Kang, Young Chun Lee, Se Youp Lee
J Korean Ophthalmol Soc. 2013;54(7):1086-1090. doi: 10.3341/jkos.2013.54.7.1086.
Reference
-
1. Wheatstone C. Contributions to the physiology of vision. Part the first. On some remarkable and hitherto unobserved phenomena of binocular vision. Philos. Trans R Soc Lond B Biol Sci. 1838. 371:128.2. Birch B, Williams C, Hunter J, Lapa MC. Random dot stereoacuity of preschool children. J Pediatr Ophthalmol Strabismus. 1997. 34:217–222.3. Tyler CW. Schor CM, Cuiffreda KJ, editors. Sensory processing of binocular disparity. Vergence Eye Movement: Basic and Clinical Aspects. 1983. Boston, Mass: Butterworths;199–295.4. Romano PE, Romano JA, Puklin JE. Stereoacuity development in children with normal binocular single vision. Am J Ophthalmol. 1975. 79:966–971.5. Jani SN. The age factor in stereopsis screening. Am J Optom. 1966. 43:653–657.6. Lee BH, Kim MM. Comparison of the Lang, Randot, TNO and new stereotests in screening and office use in children. J Korean Ophthalmol Soc. 1990. 31:651–660.7. Lee SY, Park WT. Assessment of stereoacuity with the Frisby and Lang II stereotests in preschool children. J Korean Ophthalmol Soc. 1998. 39:2165–2172.8. Lee SY, Bae SH. Assessment of stereoacuity with the Randot preschool stereoacuity and Lang test in the 2- to 5-year age range. J Korean Ophthalmol Soc. 1999. 40:1385–1390.9. Lee SY, Bae SH. Comparison of various kinds of stereoacuity tests in preschool children. J Korean Ophthalmol Soc. 2000. 41:1383–1388.10. Cho YA, Cho SW, Roh GH. Evaluation of criteria of stereoacuity for Titmus, Randot & TNO stereotests. J Korean Ophthalmol Soc. 1999. 40:532–537.11. Tychsen L. William MH, editor. Binocular vision. Adler's physiology of the eye. 1992. 9th ed. St. Louis: Mosby;773–853.12. von Noorden GK. Binocular vision and ocular motility. 1996. 5th ed. St. Louis: Mosby;8–40.13. Tatsumi S, Tahira K. Study on the stereotest (Titmus) in childhood. Folia Ophthalmol Jpn. 1972. 23:620–632.14. Tiffin B, Joseph S. Industrial Psychology. 1942. New York: Prentice-Hall Inc;134–135.15. Cohn TE, Lasley DJ. Visual depth illusion and falls in the eldly. Clin in Geriatric Med. 1985. 3:608–611.16. Kiyosawa M, Bosley TM, Chawluk J, et al. Alzheimer's disease with prominent visual symptoms. Ophthalmology. 1989. 96:1077–1086.17. Wright LA, Wormald RPL. Stereopsis and ageing. Eye. 1992. 6:473–476.18. Sadun AA, Bassi CJ. Optic nerve damage in Alzheimer's disease. Ophthalmology. 1990. 97:9–17.19. Allen MJ. Vision screening at Indiana State Fair. J Am Optom Assoc. 1964. 35:974–977.20. Bell B, Wolf E, Bernholz CD. Depth perception as a function of age. Aging Hum Dev. 1972. 3:77–81.21. Haegerstom-Portnoy G, Schneck ME, Brabyn JA. Seeing into old age: vision function beyond acuity. Opted Vis Sci. 1999. 76:141–158.22. Rubin GS, West SK, Munoz B, et al. A comprehensive assessment of visual impairment in a population of older Americans. Invest Ophthalmol Vis Sci. 1997. 38:557–568.23. Zaroff CM, Knutelska M, Frumkes TE. Variation in stereoacuity: normative description, fixation disparity, and the roles of ageing and gender. Invest Ophthalmol Vis Sci. 2003. 44:891–900.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Affecting Stereopsis After Pediatric Cataract Surgery
- Normal Distance Stereoacuity by Age Assessed by the Frisby Davis Distance Stereotest
- Stereoacuity after Successful Occlusion Therapy in Children with Anisometropic Amblyopia
- The Stereoacuity on Child Strabismus 1. Aflalysis of Horizontal Deviations
- Effect of Spherical Lens Induced Anisometropia on Dynamic Stereoacuity