J Korean Med Sci.
2023 May;38(19):e142. 10.3346/jkms.2023.38.e142.
Changes in the Circadian Rhythm of High-Frequency Heart Rate Variability Associated With Depression
- Affiliations
-
- 1Department of Psychiatry, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 2Institute of Behavioral Science in Medicine, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Yongin, Korea
- 4Department of Biomedical Informatics, Ajou University School of Medicine, Suwon, Korea
- 5BUD.on Inc., Seoul, Korea
- 6Department of Cardiology, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 7Center for Digital Health, Yongin Severance Hospital, Yonsei University Health System, Yongin, Korea
- KMID: 2542393
- DOI: http://doi.org/10.3346/jkms.2023.38.e142
Abstract
- Background
Heart rate variability (HRV) extracted from electrocardiogram measured for a short period during a resting state is clinically used as a bio-signal reflecting the emotional state. However, as interest in wearable devices increases, greater attention is being paid to HRV extracted from long-term electrocardiogram, which may contain additional clinical information. The purpose of this study was to examine the characteristics of HRV parameters extracted through long-term electrocardiogram and explore the differences between participants with and without depression and anxiety symptoms.
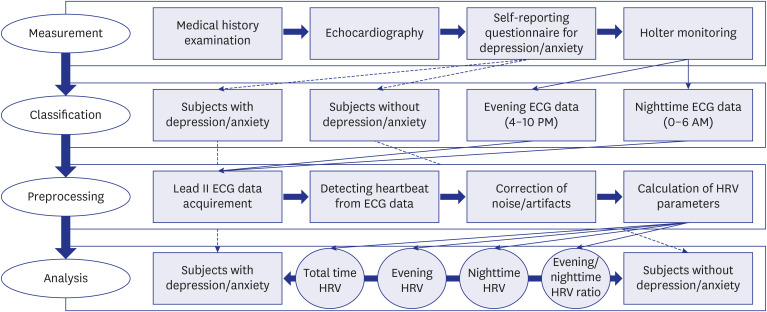
Methods
Long-term electrocardiogram was acquired from 354 adults with no psychiatric history who underwent Holter monitoring. Evening and nighttime HRV and the ratio of nighttime-to-evening HRV were compared between 127 participants with depressive symptoms and 227 participants without depressive symptoms. Comparisons were also made between participants with and without anxiety symptoms.
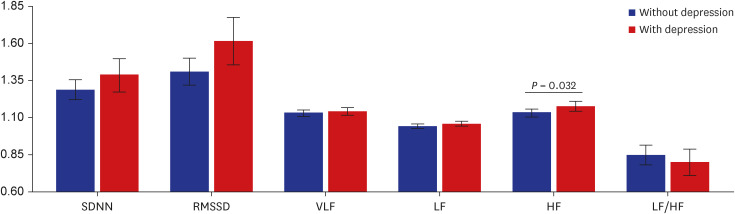
Results
Absolute values of HRV parameters did not differ between groups based on the presence of depressive or anxiety symptoms. Overall, HRV parameters increased at nighttime compared to evening. Participants with depressive symptoms showed a significantly higher nighttime-to-evening ratio of high-frequency HRV than participants without depressive symptoms. The nighttime-to-evening ratio of HRV parameters did not show a significant difference depending on the presence of anxiety symptoms.
Conclusion
HRV extracted through long-term electrocardiogram showed circadian rhythm. Depression may be associated with changes in the circadian rhythm of parasympathetic tone.
Figure
Reference
-
1. Sztajzel J. Heart rate variability: a noninvasive electrocardiographic method to measure the autonomic nervous system. Swiss Med Wkly. 2004; 134(35-36):514–522. PMID: 15517504.2. Kemp AH, Quintana DS, Gray MA, Felmingham KL, Brown K, Gatt JM. Impact of depression and antidepressant treatment on heart rate variability: a review and meta-analysis. Biol Psychiatry. 2010; 67(11):1067–1074. PMID: 20138254.3. Chalmers JA, Quintana DS, Abbott MJ, Kemp AH. Anxiety disorders are associated with reduced heart rate variability: a meta-analysis. Front Psychiatry. 2014; 5:80. PMID: 25071612.4. Shaffer F, McCraty R, Zerr CL. A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Front Psychol. 2014; 5:1040. PMID: 25324790.5. Shaffer F, Ginsberg JP. An overview of heart rate variability metrics and norms. Front Public Health. 2017; 5:258. PMID: 29034226.6. Laborde S, Mosley E, Thayer JF. Heart rate variability and cardiac vagal tone in psychophysiological research–recommendations for experiment planning, data analysis, and data reporting. Front Psychol. 2017; 8:213. PMID: 28265249.7. Kleiger RE, Stein PK, Bigger JT Jr. Heart rate variability: measurement and clinical utility. Ann Noninvasive Electrocardiol. 2005; 10(1):88–101. PMID: 15649244.8. Li KH, White FA, Tipoe T, Liu T, Wong MC, Jesuthasan A, et al. The current state of mobile phone apps for monitoring heart rate, heart rate variability, and atrial fibrillation: narrative review. JMIR Mhealth Uhealth. 2019; 7(2):e11606. PMID: 30767904.9. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983; 67(6):361–370. PMID: 6880820.10. Pan J, Tompkins WJ, Tompkins WJ. A real-time QRS detection algorithm. IEEE Trans Biomed Eng. 1985; 32(3):230–236. PMID: 3997178.11. Rasmussen JH, Rosenberger K, Langbein J. EasieRR: an open-source software for non-invasive heart rate variability assessment. Methods Ecol Evol. 2020; 11(6):773–782.12. Kher R. Signal processing techniques for removing noise from ECG signals. J Biomed Eng Res. 2019; 3(101):1–9.13. Lipponen JA, Tarvainen MP. A robust algorithm for heart rate variability time series artefact correction using novel beat classification. J Med Eng Technol. 2019; 43(3):173–181. PMID: 31314618.14. Kemp AH, Quintana DS. The relationship between mental and physical health: insights from the study of heart rate variability. Int J Psychophysiol. 2013; 89(3):288–296. PMID: 23797149.15. Björ B, Burström L, Karlsson M, Nilsson T, Näslund U, Wiklund U. Acute effects on heart rate variability when exposed to hand transmitted vibration and noise. Int Arch Occup Environ Health. 2007; 81(2):193–199. PMID: 17541625.16. Sammito S, Sammito W, Böckelmann I. The circadian rhythm of heart rate variability. Biol Rhythm Res. 2016; 47(5):717–730.17. Bertsch K, Hagemann D, Naumann E, Schächinger H, Schulz A. Stability of heart rate variability indices reflecting parasympathetic activity. Psychophysiology. 2012; 49(5):672–682. PMID: 22335779.18. Burgess HJ, Trinder J, Kim Y, Luke D. Sleep and circadian influences on cardiac autonomic nervous system activity. Am J Physiol. 1997; 273(4):H1761–H1768. PMID: 9362241.19. Jarczok MN, Guendel H, McGrath JJ, Balint EM. Circadian rhythms of the autonomic nervous system: scientific implication and practical implementation. Švorc P, editor. Chronobiology - The Science of Biological Time Structure. London, UK: IntechOpen;2019.20. Bansal D, Khan M, Salhan A. A review of measurement and analysis of heart rate variability. In : Conference proceedings of 2009 International Conference on Computer and Automation Engineering; 2009 March 8-10; Bangkok, Thailand. New York, NY, USA: Institute of Electrical and Electronics Engineers (IEEE);2009. p. 243–246.21. Beauchaine TP, Thayer JF. Heart rate variability as a transdiagnostic biomarker of psychopathology. Int J Psychophysiol. 2015; 98(2 Pt 2):338–350. PMID: 26272488.22. Rennie KL, Hemingway H, Kumari M, Brunner E, Malik M, Marmot M. Effects of moderate and vigorous physical activity on heart rate variability in a British study of civil servants. Am J Epidemiol. 2003; 158(2):135–143. PMID: 12851226.23. Kim JA, Kang SW. Relationship among sleep quality, heart rate variability, fatigue, depression, and anxiety in adults. Korean J Adult Nurs. 2017; 29(1):87–97.24. Park DH, Shin CJ, Hong SC, Yu J, Ryu SH, Kim EJ, et al. Correlation between the severity of obstructive sleep apnea and heart rate variability indices. J Korean Med Sci. 2008; 23(2):226–231. PMID: 18437004.25. Verkuil B, Brosschot JF, Marques AH, Kampschroer K, Sternberg EM, Thayer JF. Gender differences in the impact of daily sadness on 24-h heart rate variability. Psychophysiology. 2015; 52(12):1682–1688. PMID: 26338472.26. Antelmi I, de Paula RS, Shinzato AR, Peres CA, Mansur AJ, Grupi CJ. Influence of age, gender, body mass index, and functional capacity on heart rate variability in a cohort of subjects without heart disease. Am J Cardiol. 2004; 93(3):381–385. PMID: 14759400.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Circadian Variation of Cardiac Autonomic Function in Hypertensives
- The Changes in Heart Rate Variability between Morning and Afternoon
- Nonlinear Cardiac Dynamics and Morning Dip: An Unsound Circadian Rhythm
- Circadian Rhythm Disruption in Cancer Biology: A Review of Literature
- Reproducibility and diurnal variation of heart rate variability in predischarge period of acute myocardial infarction