J Korean Med Sci.
2023 May;38(19):e141. 10.3346/jkms.2023.38.e141.
The Profile of Early Sedation Depth and Clinical Outcomes of Mechanically Ventilated Patients in Korea
- Affiliations
-
- 1Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Medical Research Project Team, IM Medical, Pfizer Korea Pharmaceuticals Limited Company, Seoul, Korea
- 3Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 4Division of Biostatistics, Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea
- 5Division of Acute Care Surgery, Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 6Department of Trauma and Surgical Critical Care and Biomedical Research Institute, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
- 7Department of Intensive Care Medicine, Dong-A University Hospital, Busan, Korea
- 8Department of Surgery, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 9Department of Thoracic & Cardiovascular Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 10Department of Critical Care Medicine, Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 11Department of Critical Care Medicine, Anesthesiology and Pain Medicine, Seoul National University Hospital, Seoul, Korea
- 12Department of Acute Care Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 13Department of Thoracic and Cardiovascular Surgery, Keimyung University School of Medicine, Daegu, Korea
- 14Division of Pulmonology and Allergy, Department of Internal Medicine, Regional Center for Respiratory Diseases, Yeungnam University Medical Center, College of Medicine, Yeungnam University, Daegu, Korea
- 15Department of Thoracic and Cardiovascular Surgery, Yeungnam University Medical Center, College of Medicine, Yeungnam University, Daegu, Korea
- 16Division of Critical Care Medicine, Department of Anesthesiology and Pain Medicine, Yonsei University College of Medicine, Seoul, Korea
- 17Department of Internal Medicine, Daegu Catholic University Medical Center, Daegu Catholic University School of Medicine, Daegu, Korea
- 18Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- 19Department of Critical Care Medicine, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 20Department of Pulmonary, Allergy and Critical Care Medicine, Hallym University Sacred Heart Hospital, Hwaseong, Korea
- 21Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 22Department of Pulmonary, Allergy, and Critical Care Medicine, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 23Division of Acute Care Surgery, Department of Surgery, Korea University Guro Hospital, Seoul, Korea
- 24Department of Internal Medicine, Inje University Haeundae Paik Hospital, Busan, Korea
- KMID: 2542392
- DOI: http://doi.org/10.3346/jkms.2023.38.e141
Abstract
- Background
Current international guidelines recommend against deep sedation as it is associated with worse outcomes in the intensive care unit (ICU). However, in Korea the prevalence of deep sedation and its impact on patients in the ICU are not well known.
Methods
From April 2020 to July 2021, a multicenter, prospective, longitudinal, noninterventional cohort study was performed in 20 Korean ICUs. Sedation depth extent was divided into light and deep using a mean Richmond Agitation–Sedation Scale value within the first 48 hours. Propensity score matching was used to balance covariables; the outcomes were compared between the two groups.
Results
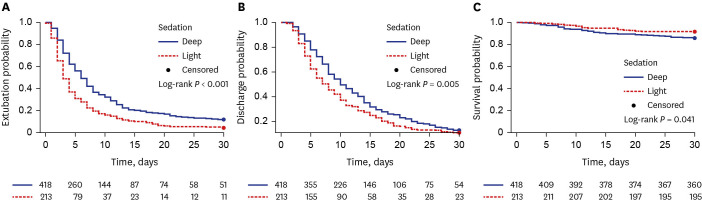
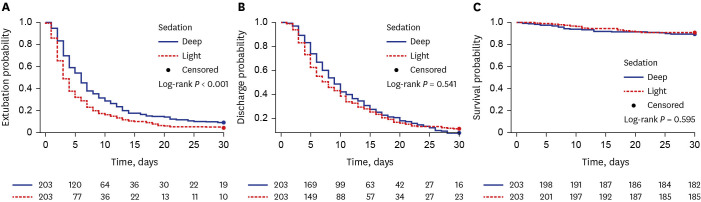
Overall, 631 patients (418 [66.2%] and 213 [33.8%] in the deep and light sedation groups, respectively) were included. Mortality rates were 14.1% and 8.4% in the deep and light sedation groups (P = 0.039), respectively. Kaplan-Meier estimates showed that time to extubation (P < 0.001), ICU length of stay (P = 0.005), and death P = 0.041) differed between the groups. After adjusting for confounders, early deep sedation was only associated with delayed time to extubation (hazard ratio [HR], 0.66; 95% confidence inter val [CI], 0.55– 0.80; P < 0.001). In the matched cohort, deep sedation remained significantly associated with delayed time to extubation (HR, 0.68; 95% 0.56–0.83; P < 0.001) but was not associated with ICU length of stay (HR, 0.94; 95% CI, 0.79–1.13; P = 0.500) and in-hospital mortality (HR, 1.19; 95% CI, 0.65–2.17; P = 0.582).
Conclusion
In many Korean ICUs, early deep sedation was highly prevalent in mechanically ventilated patients and was associated with delayed extubation, but not prolonged ICU stay or in-hospital death.
Keyword
Figure
Reference
-
1. Owen GD, Stollings JL, Rakhit S, Wang L, Yu C, Hosay MA, et al. International analgesia, sedation, and delirium practices: a prospective cohort study. J Intensive Care. 2019; 7(1):25. PMID: 31049203.2. Seo Y, Lee HJ, Ha EJ, Ha TS. 2021 KSCCM clinical practice guidelines for pain, agitation, delirium, immobility, and sleep disturbance in the intensive care unit. Acute Crit Care. 2022; 37(1):1–25. PMID: 35279975.3. Stephens RJ, Dettmer MR, Roberts BW, Ablordeppey E, Fowler SA, Kollef MH, et al. Practice patterns and outcomes associated with early sedation depth in mechanically ventilated patients: a systematic review and meta-analysis. Crit Care Med. 2018; 46(3):471–479. PMID: 29227367.4. Lee YK, Yang HS, Jeong SM, Jun GW, Um SJ. Clinical survey of sedation and analgesia procedures in intensive care units. Korean J Anesthesiol. 2009; 56(3):295–302. PMID: 30625739.5. Shehabi Y, Bellomo R, Reade MC, Bailey M, Bass F, Howe B, et al. Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am J Respir Crit Care Med. 2012; 186(8):724–731. PMID: 22859526.6. Shehabi Y, Bellomo R, Kadiman S, Ti LK, Howe B, Reade MC, et al. Sedation intensity in the first 48 hours of mechanical ventilation and 180-day mortality: a multinational prospective longitudinal cohort study. Crit Care Med. 2018; 46(6):850–859. PMID: 29498938.7. Balzer F, Weiß B, Kumpf O, Treskatsch S, Spies C, Wernecke KD, et al. Early deep sedation is associated with decreased in-hospital and two-year follow-up survival. Crit Care. 2015; 19(1):197. PMID: 25928417.8. Kress JP, Pohlman AS, O’Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N Engl J Med. 2000; 342(20):1471–1477. PMID: 10816184.9. Girard TD, Kress JP, Fuchs BD, Thomason JW, Schweickert WD, Pun BT, et al. Efficacy and safety of a paired sedation and ventilator weaning protocol for mechanically ventilated patients in intensive care (Awakening and Breathing Controlled trial): a randomised controlled trial. Lancet. 2008; 371(9607):126–134. PMID: 18191684.10. Burry L, Rose L, McCullagh IJ, Fergusson DA, Ferguson ND, Mehta S. Daily sedation interruption versus no daily sedation interruption for critically ill adult patients requiring invasive mechanical ventilation. Cochrane Database Syst Rev. 2014; 2014(7):CD009176. PMID: 25005604.11. Olsen HT, Nedergaard HK, Strøm T, Oxlund J, Wian KA, Ytrebø LM, et al. Nonsedation or light sedation in critically ill, mechanically ventilated patients. N Engl J Med. 2020; 382(12):1103–1111. PMID: 32068366.12. Devlin JW, Skrobik Y, Gélinas C, Needham DM, Slooter AJ, Pandharipande PP, et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit Care Med. 2018; 46(9):e825–e873. PMID: 30113379.13. Pearson SD, Patel BK. Evolving targets for sedation during mechanical ventilation. Curr Opin Crit Care. 2020; 26(1):47–52. PMID: 31764193.14. Jackson DL, Proudfoot CW, Cann KF, Walsh TS. The incidence of sub-optimal sedation in the ICU: a systematic review. Crit Care. 2009; 13(6):R204. PMID: 20015357.15. Luetz A, Balzer F, Radtke FM, Jones C, Citerio G, Walder B, et al. Delirium, sedation and analgesia in the intensive care unit: a multinational, two-part survey among intensivists. PLoS One. 2014; 9(11):e110935. PMID: 25398099.16. García-Sánchez M, Caballero-López J, Ceniceros-Rozalén I, Giménez-Esparza Vich C, Romera-Ortega MA, Pardo-Rey C, et al. Management of analgesia, sedation and delirium in Spanish Intensive Care Units: a national two-part survey. Med Intensiva (Engl Ed). 2019; 43(4):225–233. PMID: 30704803.17. Lee H, Choi S, Jang EJ, Lee J, Kim D, Yoo S, et al. Effect of sedatives on in-hospital and long-term mortality of critically ill patients requiring extended mechanical ventilation for ≥ 48 hours. J Korean Med Sci. 2021; 36(34):e221. PMID: 34463064.18. Ely EW, Truman B, Shintani A, Thomason JW, Wheeler AP, Gordon S, et al. Monitoring sedation status over time in ICU patients: reliability and validity of the Richmond Agitation-Sedation Scale (RASS). JAMA. 2003; 289(22):2983–2991. PMID: 12799407.19. Stephens RJ, Ablordeppey E, Drewry AM, Palmer C, Wessman BT, Mohr NM, et al. Analgosedation practices and the impact of sedation depth on clinical outcomes among patients requiring mechanical ventilation in the ED: a cohort study. Chest. 2017; 152(5):963–971. PMID: 28645462.20. Fuller BM, Roberts BW, Mohr NM, Knight WA 4th, Adeoye O, Pappal RD, et al. The ED-SED study: a multicenter, prospective cohort study of practice patterns and clinical outcomes associated with emergency department sedation for mechanically ventilated patients. Crit Care Med. 2019; 47(11):1539–1548. PMID: 31393323.21. Strøm T, Martinussen T, Toft P. A protocol of no sedation for critically ill patients receiving mechanical ventilation: a randomised trial. Lancet. 2010; 375(9713):475–480. PMID: 20116842.22. Shehabi Y, Chan L, Kadiman S, Alias A, Ismail WN, Tan MA, et al. Sedation depth and long-term mortality in mechanically ventilated critically ill adults: a prospective longitudinal multicentre cohort study. Intensive Care Med. 2013; 39(5):910–918. PMID: 23344834.23. Tanaka LM, Azevedo LC, Park M, Schettino G, Nassar AP Jr, Réa-Neto A, et al. Early sedation and clinical outcomes of mechanically ventilated patients: a prospective multicenter cohort study. Crit Care. 2014; 18(4):R156. PMID: 25047960.24. Shehabi Y, Bellomo R, Reade MC, Bailey M, Bass F, Howe B, et al. Early goal-directed sedation versus standard sedation in mechanically ventilated critically ill patients: a pilot study. Crit Care Med. 2013; 41(8):1983–1991. PMID: 23863230.25. Bugedo G, Tobar E, Aguirre M, Gonzalez H, Godoy J, Lira MT, et al. The implementation of an analgesia-based sedation protocol reduced deep sedation and proved to be safe and feasible in patients on mechanical ventilation. Rev Bras Ter Intensiva. 2013; 25(3):188–196. PMID: 24213081.26. Finkielman JD. Randomized trial of light versus deep sedation on mental health after critical illness. Crit Care Med. 2010; 38(1):349. PMID: 20023512.27. Samuelson KA, Lundberg D, Fridlund B. Light vs. heavy sedation during mechanical ventilation after oesophagectomy--a pilot experimental study focusing on memory. Acta Anaesthesiol Scand. 2008; 52(8):1116–1123. PMID: 18840113.28. Muller L, Chanques G, Bourgaux C, Louart G, Jaber S, Fabbro-Peray P, et al. Impact of the use of propofol remifentanil goal-directed sedation adapted by nurses on the time to extubation in mechanically ventilated ICU patients: the experience of a French ICU. Ann Fr Anesth Reanim. 2008; 27(6):481.e1–481.e8.29. Pandharipande PP, Pun BT, Herr DL, Maze M, Girard TD, Miller RR, et al. Effect of sedation with dexmedetomidine vs lorazepam on acute brain dysfunction in mechanically ventilated patients: the MENDS randomized controlled trial. JAMA. 2007; 298(22):2644–2653. PMID: 18073360.30. Azevedo LC, Park M, Salluh JI, Rea-Neto A, Souza-Dantas VC, Varaschin P, et al. Clinical outcomes of patients requiring ventilatory support in Brazilian intensive care units: a multicenter, prospective, cohort study. Crit Care. 2013; 17(2):R63. PMID: 23557378.31. Guérin C. Calming down about sedation in critically ill patients. N Engl J Med. 2020; 382(12):1162–1164. PMID: 32068367.32. Kiekkas P, Aretha D, Panteli E, Baltopoulos GI, Filos KS. Unplanned extubation in critically ill adults: clinical review. Nurs Crit Care. 2013; 18(3):123–134. PMID: 23577947.33. Aydoğan S, Kaya N. The assessment of the risk of unplanned extubation in an adult intensive care unit. Dimens Crit Care Nurs. 2017; 36(1):14–21. PMID: 27902657.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Early Sedation Depth and Clinical Outcomes in Mechanically Ventilated Patients in a Hospital: Retrospective Cohort Study
- Continuous Infusion of Midazolam for Short-term Sedation in Critically III Patients
- Comparison of salivary and serum cortisol levels in mechanically ventilated patients and non-critically ill patients
- Comparison of Propofol and Midazolam for Sedation of Mechanically Ventilated Patients
- The Administration Patterns of Sedatives for Sedation of Mechanically Ventilated Patients and Patient Assessment by Nurses