Ann Surg Treat Res.
2023 May;104(5):258-268. 10.4174/astr.2023.104.5.258.
The influence of the extent of lymph node metastasis on the prognosis for patients with intrahepatic cholangiocarcinoma
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 2Department of Pathology, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 3Center of Hepato‑Pancreato‑Biliary Surgery, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- 4State Key Laboratory of Oncology in Southern China, Department of Medical Imaging, Sun Yat-sen University Cancer Center, Guangzhou, China
- 5Department of Oncology, The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China
- KMID: 2542232
- DOI: http://doi.org/10.4174/astr.2023.104.5.258
Abstract
- Purpose
Reports showed that some of intrahepatic cholangiocarcinoma (ICC) patients with lymph node metastasis (LNM) may also gain survival benefit undergone resection. However, the effect of the extent of LNM on prognosis and surgical indication is barely discussed.
Methods
From September 1994 to November 2018, primary ICC patients undergone initial curable surgery were enrolled. Based on the extent of LNM, we divided these patients into 4 groups, including patients with no LNM (group N0), LNM to hepatoduodenal ligament or common hepatic artery (region A, group A), LNM to gastrohepatic lymph nodes for left liver ICC and periduodenal and peripancreatic lymph node for right liver ICC (region B, group B), or LNM beyond these regions (region C, group C). Multivariable Cox regression analysis was performed to identify the prognostic factors for recurrencefree survival (RFS) and overall survival (OS) in all groups.
Results
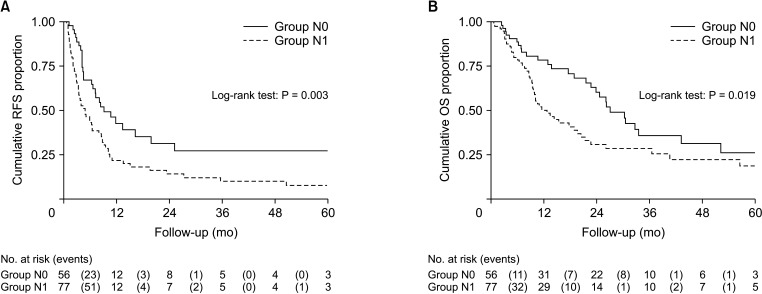
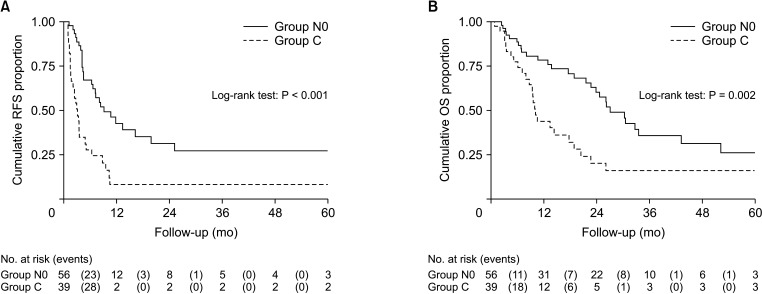
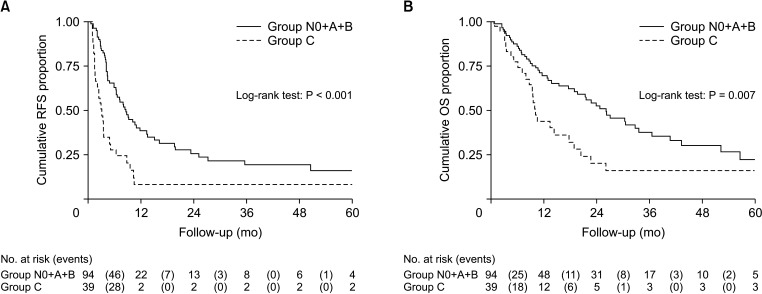
A total of 133 patients were enrolled. There were 56, 21, 17, and 39 patients in groups N0, A, B, and C, respectively. There was significant difference between groups N0 and C in RFS (P < 0.001) and OS (P = 0.002). When we compared group N0 + A + B with group C, we also found that RFS (P < 0.001) and OS (P = 0.007) were significantly different. In multivariable analysis, the extent of LNM was an independent risk factor for RFS (P < 0.050).
Conclusion
ICC patients with the LNM to regions A and B could still achieve good prognosis with resection. Surgery should be carefully considered when LNM to region C.
Keyword
Figure
Reference
-
1. Rizvi S, Khan SA, Hallemeier CL, Kelley RK, Gores GJ. Cholangiocarcinoma: evolving concepts and therapeutic strategies. Nat Rev Clin Oncol. 2018; 15:95–111. PMID: 28994423.2. Sirica AE, Gores GJ, Groopman JD, Selaru FM, Strazzabosco M, Wei Wang X, et al. Intrahepatic cholangiocarcinoma: continuing challenges and translational advances. Hepatology. 2019; 69:1803–1815. PMID: 30251463.3. Shaib Y, El-Serag HB. The epidemiology of cholangiocarcinoma. Semin Liver Dis. 2004; 24:115–125. PMID: 15192785.4. Bagante F, Spolverato G, Weiss M, Alexandrescu S, Marques HP, Aldrighetti L, et al. Assessment of the lymph node status in patients undergoing liver resection for intrahepatic cholangiocarcinoma: the new eighth edition AJCC staging system. J Gastrointest Surg. 2018; 22:52–59. PMID: 28424987.5. de Jong MC, Nathan H, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol. 2011; 29:3140–3145. PMID: 21730269.6. Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and prognosis for patients with intrahepatic cholangiocarcinoma: systematic review and meta-analysis. JAMA Surg. 2014; 149:565–574. PMID: 24718873.7. Wang Y, Li J, Xia Y, Gong R, Wang K, Yan Z, et al. Prognostic nomogram for intrahepatic cholangiocarcinoma after partial hepatectomy. J Clin Oncol. 2013; 31:1188–1195. PMID: 23358969.8. Choi SB, Kim KS, Choi JY, Park SW, Choi JS, Lee WJ, et al. The prognosis and survival outcome of intrahepatic cholangiocarcinoma following surgical resection: association of lymph node metastasis and lymph node dissection with survival. Ann Surg Oncol. 2009; 16:3048–3056. PMID: 19626372.9. National Comprehensive Cancer Network (NCCN). NCCN clinical practice guidelines in oncology: hepatobiliary cancers, version 2.2022 [Internet]. NCCN;2022. updated 2022 Jul 15. cited 2022 Aug 31. Available from: https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf .10. Nagino M, Hirano S, Yoshitomi H, Aoki T, Uesaka K, Unno M, et al. Clinical practice guidelines for the management of biliary tract cancers 2019: the 3rd English edition. J Hepatobiliary Pancreat Sci. 2021; 28:26–54. PMID: 33259690.11. Trutmann M, Sasse D. The lymphatics of the liver. Anat Embryol (Berl). 1994; 190:201–209. PMID: 7818092.12. Morine Y, Shimada M. The value of systematic lymph node dissection for intrahepatic cholangiocarcinoma from the viewpoint of liver lymphatics. J Gastroenterol. 2015; 50:913–927. PMID: 25833009.13. Pupulim LF, Vilgrain V, Ronot M, Becker CD, Breguet R, Terraz S. Hepatic lymphatics: anatomy and related diseases. Abdom Imaging. 2015; 40:1997–2011. PMID: 25579171.14. Tsuji T, Hiraoka T, Kanemitsu K, Takamori H, Tanabe D, Tashiro S. Lymphatic spreading pattern of intrahepatic cholangiocarcinoma. Surgery. 2001; 129:401–407. PMID: 11283529.15. Okami J, Dono K, Sakon M, Tsujie M, Hayashi N, Fujiwara Y, et al. Patterns of regional lymph node involvement in intrahepatic cholangiocarcinoma of the left lobe. J Gastrointest Surg. 2003; 7:850–856. PMID: 14592657.16. Noji T, Kondo S, Hirano S, Tanaka E, Ambo Y, Kawarada Y, et al. CT evaluation of paraaortic lymph node metastasis in patients with biliary cancer. J Gastroenterol. 2005; 40:739–743. PMID: 16082591.17. Grobmyer SR, Wang L, Gonen M, Fong Y, Klimstra D, D’Angelica M, et al. Perihepatic lymph node assessment in patients undergoing partial hepatectomy for malignancy. Ann Surg. 2006; 244:260–264. PMID: 16858189.18. Noji T, Kondo S, Hirano S, Tanaka E, Suzuki O, Shichinohe T. Computed tomography evaluation of regional lymph node metastases in patients with biliary cancer. Br J Surg. 2008; 95:92–96. PMID: 17853509.19. Ercolani G, Vetrone G, Grazi GL, Aramaki O, Cescon M, Ravaioli M, et al. Intrahepatic cholangiocarcinoma: primary liver resection and aggressive multimodal treatment of recurrence significantly prolong survival. Ann Surg. 2010; 252:107–114. PMID: 20531002.20. Nakagawa T, Kamiyama T, Kurauchi N, Matsushita M, Nakanishi K, Kamachi H, et al. Number of lymph node metastases is a significant prognostic factor in intrahepatic cholangiocarcinoma. World J Surg. 2005; 29:728–733. PMID: 15880276.21. Kim Y, Spolverato G, Amini N, Margonis GA, Gupta R, Ejaz A, et al. Surgical management of intrahepatic cholangiocarcinoma: defining an optimal prognostic lymph node stratification schema. Ann Surg Oncol. 2015; 22:2772–2778. PMID: 25663595.22. Jutric Z, Johnston WC, Hoen HM, Newell PH, Cassera MA, Hammill CW, et al. Impact of lymph node status in patients with intrahepatic cholangiocarcinoma treated by major hepatectomy: a review of the National Cancer Database. HPB (Oxford). 2016; 18:79–87. PMID: 26776855.23. Guglielmi A, Ruzzenente A, Campagnaro T, Valdegamberi A, Bagante F, Bertuzzo F, et al. Patterns and prognostic significance of lymph node dissection for surgical treatment of perihilar and intrahepatic cholangiocarcinoma. J Gastrointest Surg. 2013; 17:1917–1928. PMID: 24048613.24. Ohtsuka M, Ito H, Kimura F, Shimizu H, Togawa A, Yoshidome H, et al. Results of surgical treatment for intrahepatic cholangiocarcinoma and clinicopathological factors influencing survival. Br J Surg. 2002; 89:1525–1531. PMID: 12445060.25. Weber SM, Jarnagin WR, Klimstra D, DeMatteo RP, Fong Y, Blumgart LH. Intrahepatic cholangiocarcinoma: resectability, recurrence pattern, and outcomes. J Am Coll Surg. 2001; 193:384–391. PMID: 11584966.26. Tajima Y, Kuroki T, Fukuda K, Tsuneoka N, Furui J, Kanematsu T. An intraductal papillary component is associated with prolonged survival after hepatic resection for intrahepatic cholangiocarcinoma. Br J Surg. 2004; 91:99–104. PMID: 14716802.27. Shimada M, Yamashita Y, Aishima S, Shirabe K, Takenaka K, Sugimachi K. Value of lymph node dissection during resection of intrahepatic cholangiocarcinoma. Br J Surg. 2001; 88:1463–1466. PMID: 11683741.28. Yamamoto M, Takasaki K, Yoshikawa T. Lymph node metastasis in intrahepatic cholangiocarcinoma. Jpn J Clin Oncol. 1999; 29:147–150. PMID: 10225697.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intrahepatic Cholangiocarcinoma Initially Presented as a Distant Metastatic Lymph Node without Demonstrable Hepatic Mass: A Case Report
- Analysis of 50 Consecutive Hepatic Resection Cases for Intrahepatic Cholangiocarcinoma
- Prognostic Factors for Intrahepatic Cholangiocarcinoma Treated with Surgical Resection
- Review: Analysis of Survival Rate and Prognostic Factors of Intrahepatic Cholangiocarcinoma: 318 Cases in Single Institute
- Optimal Neck Dissection Extent for Metastatic Lymph Nodes in Papillary Thyroid Cancer