Brain Tumor Res Treat.
2023 Apr;11(2):153-157. 10.14791/btrt.2023.0006.
Pituitary Apoplexy After Leuprolide Therapy in a Breast Cancer Patient: A Case Report
- Affiliations
-
- 1Department of Radiology, Soonchunghyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 2Department of Neurosurgery, Soonchunghyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea
- 3Department of Radiology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- KMID: 2542078
- DOI: http://doi.org/10.14791/btrt.2023.0006
Abstract
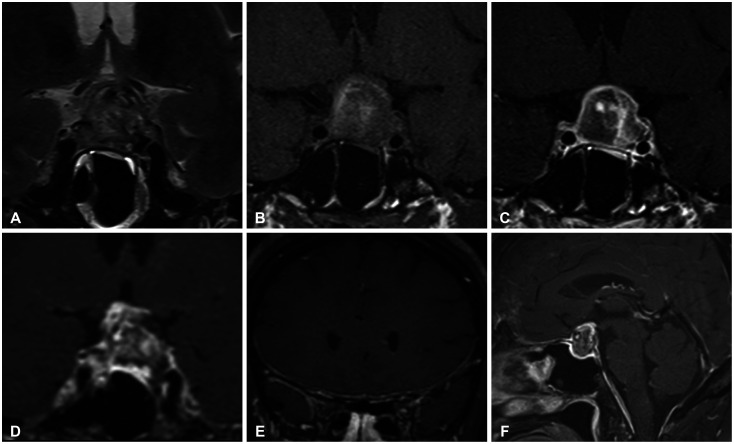
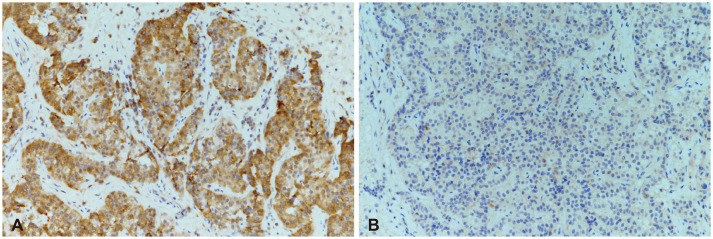
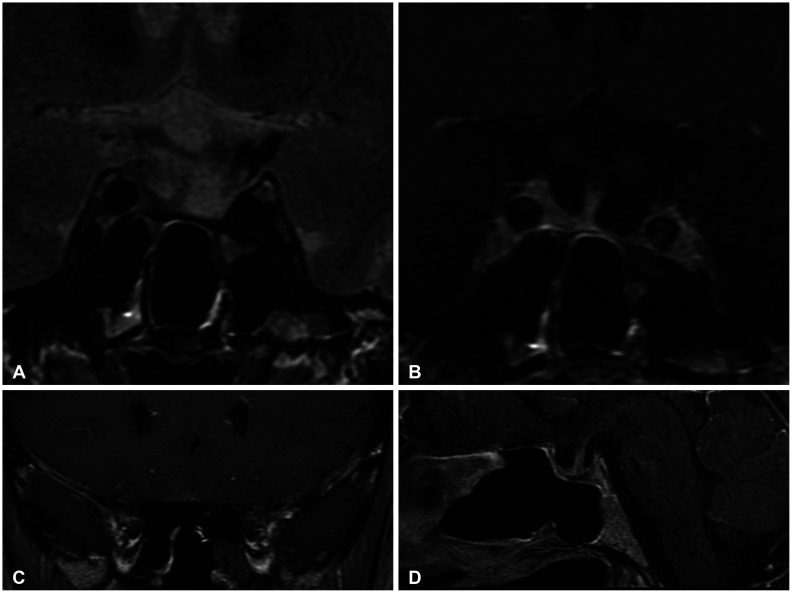
- Pituitary apoplexy (PA) is a clinical syndrome resulting from sudden hemorrhage and/or infarction of the pituitary gland. Recent reports documented the development of PA secondary to treatment with gonadotropin-releasing hormone (GnRH) agonists for prostate cancer. A 52-year-old woman visited our emergency room with a severe headache, occurred 1 day prior. She underwent breast-conserving surgery for breast cancer 1 month prior. She was currently undergoing radiation and hormone therapy, consisting of leuprorelin. Brain contrast-enhanced MRI revealed a pituitary adenoma with internal hemorrhage in the sellar and suprasellar areas. Pachymeningeal enhancement was observed along the retroclival and bilateral frontal areas. The patient was diagnosed with PA and aseptic meningitis. The patient underwent total excision via transsphenoidal surgery 8 days after admission. The patient was pathologically diagnosed with a pituitary adenoma with necrosis. On immunochemical staining, the tumor was positive for follicle-stimulating hormone. The follow-up MRI revealed no evidence of residual tumor or an improved pachymeningeal enhancement. She is currently undergoing follow-up at the neurosurgery and endocrinology outpatient departments with no noted complications. In breast cancer patients receiving GnRH agonist therapy, PA may be rare complication.
Keyword
Figure
Reference
-
1. Briet C, Salenave S, Bonneville JF, Laws ER, Chanson P. Pituitary apoplexy. Endocr Rev. 2015; 36:622–645. PMID: 26414232.2. Fernandez A, Karavitaki N, Wass JA. Prevalence of pituitary adenomas: a community-based, cross-sectional study in Banbury (Oxfordshire, UK). Clin Endocrinol (Oxf). 2010; 72:377–382. PMID: 19650784.3. Laws ER. Pituitary tumor apoplexy: a review. J Intensive Care Med. 2008; 23:146–147. PMID: 18372353.4. Raj R, Elshimy G, Jacob A, Arya PVA, Unnikrishnan DC, Correa R, et al. Pituitary apoplexy induced by gonadotropin-releasing hormone (GnRH) agonist administration for treatment of prostate cancer: a systematic review. J Cancer Res Clin Oncol. 2021; 147:2337–2347. PMID: 34156518.5. Tanios G, Mungo NA, Kapila A, Bajaj K. Pituitary apoplexy: a rare complication of leuprolide therapy in prostate cancer treatment. BMJ Case Rep. 2017; 2017:bcr2016218514.6. Elshimy G, Raj R, Jacob A, Correa R. Late onset of pituitary apoplexy following gonadotropin-releasing hormone agonist for prostate cancer treatment. BMJ Case Rep. 2022; 15:e248523.7. Barbosa M, Paredes S, Machado MJ, Almeida R, Marques O. Pituitary apoplexy induced by gonadotropin-releasing hormone agonist administration: a rare complication of prostate cancer treatment. Endocrinol Diabetes Metab Case Rep. 2020; 2020:20-0018.8. Voica M, Tetlay M, Hasan F. Abstract# 993208: pituitary apoplexy secondary to GnRH agonist, leuprolide, for breast cancer: a case study and review of the literature. Endocr Pract. 2021; 27(supplement):S108–S109.9. Sasagawa Y, Tachibana O, Nakagawa A, Koya D, Iizuka H. Pituitary apoplexy following gonadotropin-releasing hormone agonist administration with gonadotropin-secreting pituitary adenoma. J Clin Neurosci. 2015; 22:601–603. PMID: 25455737.10. Chen Z, Xu L, Shi W, Zeng F, Zhuo R, Hao X, et al. Trends of female and male breast cancer incidence at the global, regional, and national levels, 1990-2017. Breast Cancer Res Treat. 2020; 180:481–490. PMID: 32056055.11. Poggio F, Lambertini M, Bighin C, Conte B, Blondeaux E, D’Alonzo A, et al. Potential mechanisms of ovarian protection with gonadotropin-releasing hormone agonist in breast cancer patients: a review. Clin Med Insights Reprod Health. 2019; 13:1179558119864584. PMID: 31391786.12. Berghoff AS, Schur S, Fureder LM, Gatterbauer B, Dieckmann K, Widhalm G, et al. Descriptive statistical analysis of a real life cohort of 2419 patients with brain metastases of solid cancers. ESMO Open. 2016; 1:e000024. PMID: 27843591.13. Hadjipanteli A, Doolan P, Kyriacou E, Constantinidou A. Breast cancer brain metastasis: the potential role of MRI beyond current clinical applications. Cancer Manag Res. 2020; 12:9953–9964. PMID: 33116852.14. Smirniotopoulos JG, Murphy FM, Rushing EJ, Rees JH, Schroeder JW. Patterns of contrast enhancement in the brain and meninges. Radiographics. 2007; 27:525–551. PMID: 17374867.15. Wolansky LJ, Gallagher JD, Heary RF, Malantic GP, Dasmahapatra A, Shaderowfsky PD, et al. MRI of pituitary abscess: two cases and review of the literature. Neuroradiology. 1997; 39:499–503. PMID: 9258927.16. Colli ML, Migowski W Jr, Czepielewski MA, Ferreira N, Gross JL. [Pituitary abscess simulating apoplexy]. Arq Bras Endocrinol Metabol. 2006; 50:1122–1126. Portuguese. PMID: 17221121.17. Bjerre P, Lindholm J. Pituitary apoplexy with sterile meningitis. Acta Neurol Scand. 1986; 74:304–307. PMID: 3811836.