J Korean Med Sci.
2023 May;38(18):e136. 10.3346/jkms.2023.38.e136.
Weight Changes and Unhealthy Weight Control Behaviors Are Associated With Dysmenorrhea in Young Women
- Affiliations
-
- 1Division of Population Health Research, Department of Precision Medicine, Korea National Institute of Health, Korea Disease Control and Prevention Agency, Cheongju, Korea
- 2Department of Precision Medicine, Korea National Institute of Health, Korea Disease Control and Prevention Agency, Cheongju, Korea
- KMID: 2542028
- DOI: http://doi.org/10.3346/jkms.2023.38.e136
Abstract
- Background
This study aimed to evaluate the prevalence of dysmenorrhea and to investigate the effect of weight changes or unhealthy weight control behaviors on dysmenorrhea in young Korean women.
Methods
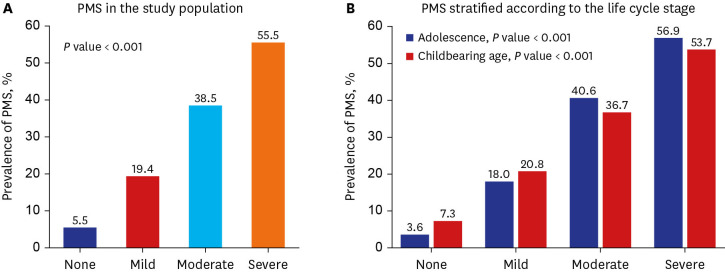
We used large-scale data of women, aged 14 to 44 years, who participated in the Korean Study of Women’s Health-Related Issues. Dysmenorrhea was measured using a visual analog scale and was categorized as none, mild, moderate, and severe according to the severity. Weight changes and unhealthy weight control behaviors (any of the behaviors, fasting/meal skipping, drugs, the use of unapproved dietary supplements, and one-food diets) over the past year were self-reported. We used multinomial logistic regression to investigate the association between weight changes or unhealthy weight control behaviors and dysmenorrhea.
Results
Of the 5,829 young women participating in the study, 5,245 (90.0%) participants experienced dysmenorrhea [2,184 (37.5%) had moderate and 1,358 (23.3%) had severe]. After adjusting for confounders, the odds ratios for moderate and severe dysmenorrhea in participants with weight changes ≥ 3 kg (vs. < 3 kg) were 1.19 (95% confidence interval: 1.05–1.35) and 1.25 (95% confidence interval: 1.08–1.45), respectively. The odds ratios in participants with any unhealthy weight control behaviors were 1.22 (95% confidence interval: 1.04–1.42) and 1.41 (95% confidence interval: 1.19–1.67) for those with moderate and severe dysmenorrhea, respectively.
Conclusion
Weight changes (≥ 3 kg) or unhealthy weight control behaviors are common among young women, which may adversely affect dysmenorrhea. Therefore, attention needs to be paid to excessive weight changes and unhealthy weight control behaviors to improve dysmenorrhea in young women.
Figure
Reference
-
1. The American College of Obstetricians and Gynecologists (ACOG). Dysmenorrhea: painful periods. Update 2020. Accessed June 13, 2022. https://www.acog.org/womens-health/faqs/dysmenorrhea-painful-periods .2. Armour M, Parry K, Manohar N, Holmes K, Ferfolja T, Curry C, et al. The prevalence and academic impact of dysmenorrhea in 21,573 young women: a systematic review and meta-analysis. J Womens Health (Larchmt). 2019; 28(8):1161–1171. PMID: 31170024.
Article3. Banikarim C, Chacko MR, Kelder SH. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch Pediatr Adolesc Med. 2000; 154(12):1226–1229. PMID: 11115307.
Article4. Iacovides S, Avidon I, Baker FC. What we know about primary dysmenorrhea today: a critical review. Hum Reprod Update. 2015; 21(6):762–778. PMID: 26346058.
Article5. Kim J. Factors affecting dysmenorrhea in undergraduate students. J Korean Acad Soc Nurs Educ. 2014; 20(2):350–357.
Article6. Hu Z, Tang L, Chen L, Kaminga AC, Xu H. Prevalence and risk factors associated with primary dysmenorrhea among Chinese female university students: a cross-sectional study. J Pediatr Adolesc Gynecol. 2020; 33(1):15–22. PMID: 31539615.
Article7. Pejčić A, Janković S. Risk factors for dysmenorrhea among young adult female university students. Ann Ist Super Sanita. 2016; 52(1):98–103. PMID: 27033624.8. Çaltekin İ, Hamamcı M, Demir Çaltekin M, Onat T. Evaluation of sleep disorders, anxiety and depression in women with dysmenorrhea. Sleep Biol Rhythms. 2021; 19(1):13–21.
Article9. Qin LL, Hu Z, Kaminga AC, Luo BA, Xu HL, Feng XL, et al. Association between cigarette smoking and the risk of dysmenorrhea: a meta-analysis of observational studies. PLoS One. 2020; 15(4):e0231201. PMID: 32294123.
Article10. Laxy M, Holle R, Döring A, Peters A, Hunger M. The longitudinal association between weight change and health-related quality of life: the KORA S4/F4 cohort study. Int J Public Health. 2014; 59(2):279–288. PMID: 23999627.
Article11. Nanri A, Mizoue T, Takahashi Y, Noda M, Inoue M, Tsugane S, et al. Weight change and all-cause, cancer and cardiovascular disease mortality in Japanese men and women: the Japan Public Health Center-Based Prospective Study. Int J Obes. 2010; 34(2):348–356.
Article12. Greenberg BS, Eastin M, Hofschire L, Lachlan K, Brownell KD. Portrayals of overweight and obese individuals on commercial television. Am J Public Health. 2003; 93(8):1342–1348. PMID: 12893625.
Article13. Yates A, Edman J, Aruguete M. Ethnic differences in BMI and body/self-dissatisfaction among Whites, Asian subgroups, Pacific Islanders, and African-Americans. J Adolesc Health. 2004; 34(4):300–307. PMID: 15040999.
Article14. Wardle J, Haase AM, Steptoe A. Body image and weight control in young adults: international comparisons in university students from 22 countries. Int J Obes. 2006; 30(4):644–651.
Article15. Noh JW, Kwon YD, Yang Y, Cheon J, Kim J. Relationship between body image and weight status in east Asian countries: comparison between South Korea and Taiwan. BMC Public Health. 2018; 18(1):814. PMID: 29970058.
Article16. Talamayan KS, Springer AE, Kelder SH, Gorospe EC, Joye KA. Prevalence of overweight misperception and weight control behaviors among normal weight adolescents in the United States. Sci World J. 2006; 6:365–373.
Article17. Park B, Cho HN, Choi E, Seo DH, Kim NS, Park E, et al. Weight control behaviors according to body weight status and accuracy of weight perceptions among Korean women: a nationwide population-based survey. Sci Rep. 2019; 9(1):9127. PMID: 31235742.
Article18. Cho HN, Choi E, Seo DH, Suh M, Lee HY, Park B, et al. The Korean Study of Women’s Health-Related Issues (K-Stori): rationale and study design. BMC Public Health. 2017; 17(1):609. PMID: 28662652.
Article19. Statistics Korea. Korean Standard Classification of Diseases and Causes of Death (KCD-7). Updated 2016. Accessed November 3, 2022. https://kssc.kostat.go.kr:8443/ksscNew_web/ekssc/main/main.do .20. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res (Hoboken). 2011; 63(Suppl 11):S240–S252. PMID: 22588748.21. Aubrun F, Langeron O, Quesnel C, Coriat P, Riou B. Relationships between measurement of pain using visual analog score and morphine requirements during postoperative intravenous morphine titration. Anesthesiology. 2003; 98(6):1415–1421. PMID: 12766651.
Article22. Kazama M, Maruyama K, Nakamura K. Prevalence of dysmenorrhea and its correlating lifestyle factors in Japanese female junior high school students. Tohoku J Exp Med. 2015; 236(2):107–113. PMID: 26027596.
Article23. Korea Disease Control and Prevention Agency. The Korea National Health and Nutrition Examination Survey VI (2013–2015) Analysis Guideline. Cheongju, Korea: Korea Disease Control and Prevention Agency;2015.24. Jang HJ, Kim BS, Won CW, Kim SY, Seo MW. The relationship between psychological factors and weight gain. Korean J Fam Med. 2020; 41(6):381–386. PMID: 32403901.
Article25. Neumark-Sztainer D, Croll J, Story M, Hannan PJ, French SA, Perry C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: findings from Project EAT. J Psychosom Res. 2002; 53(5):963–974. PMID: 12445586.
Article26. Regier DA, Kuhl EA, Kupfer DJ. The DSM-5: classification and criteria changes. World Psychiatry. 2013; 12(2):92–98. PMID: 23737408.
Article27. CDC. Sleep and sleep disorders: how much sleep do I need? Updated 2017. Accessed June 8, 2022. https://www.cdc.gov/sleep/about_sleep/how_much_sleep.html .28. Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989; 28(2):193–213. PMID: 2748771.
Article29. The American College of Obstetricians and Gynecologists (ACOG). Guidelines for Women’s Health Care: A Resource Manual. 4th ed. Washington, D.C., USA: American College of Obstetricians and Gynecologists;2014. p. 607–613. .30. WHO. World Health Survey 2002: Individual Questionnaire. Geneva, Switzerland: World Health Organization;2002.31. Lee EH, Chung BY, Suh CH, Jung JY. Korean versions of the Perceived Stress Scale (PSS-14, 10 and 4): psychometric evaluation in patients with chronic disease. Scand J Caring Sci. 2015; 29(1):183–192. PMID: 24660854.
Article32. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–613. PMID: 11556941.34. Pickles VR, Hall WJ, Best FA, Smith GN. Prostaglandins in endometrium and menstrual fluid from normal and dysmenorrhoeic subjects. J Obstet Gynaecol Br Commonw. 1965; 72(2):185–192. PMID: 14273094.
Article35. Fajrin I, Alam G, Usman AN. Prostaglandin level of primary dysmenorrhea pain sufferers. Enferm Clin. 2020; 30(2):5–9.
Article36. Strömberg P, Åkerlund M, Forsling ML, Granström E, Kindahl H. Vasopressin and prostaglandins in premenstrual pain and primary dysmenorrhea. Acta Obstet Gynecol Scand. 1984; 63(6):533–538. PMID: 6542295.
Article37. Neumark-Sztainer D, Wall M, Story M, Standish AR. Dieting and unhealthy weight control behaviors during adolescence: associations with 10-year changes in body mass index. J Adolesc Health. 2012; 50(1):80–86. PMID: 22188838.
Article38. Bougoulia M, Triantos A, Koliakos G. Plasma interleukin-6 levels, glutathione peroxidase and isoprostane in obese women before and after weight loss. Association with cardiovascular risk factors. Hormones (Athens). 2006; 5(3):192–199. PMID: 16950753.
Article39. Campión J, Milagro FI, Goyenechea E, Martínez JA. TNF-α promoter methylation as a predictive biomarker for weight-loss response. Obesity (Silver Spring). 2009; 17(6):1293–1297. PMID: 19584886.
Article40. Morris FL, Payne WR, Wark JD. Prospective decrease in progesterone concentrations in female lightweight rowers during the competition season compared with the off season: a controlled study examining weight loss and intensive exercise. Br J Sports Med. 1999; 33(6):417–422. PMID: 10597853.
Article41. Falsetti L, Pasinetti E, Mazzani MD, Gastaldi A. Weight loss and menstrual cycle: clinical and endocrinological evaluation. Gynecol Endocrinol. 1992; 6(1):49–56. PMID: 1580168.
Article42. Grulović B, Pucelj MR, Krnić M, Kokić V. Impact of prostaglandin F2-alpha and tumor necrosis factor-alpha (TNF-alpha) on pain in patients undergoing thermal balloon endometrial ablation. Coll Antropol. 2013; 37(4):1185–1190. PMID: 24611332.43. Whitcomb BW, Mumford SL, Perkins NJ, Wactawski-Wende J, Bertone-Johnson ER, Lynch KE, et al. Urinary cytokine and chemokine profiles across the menstrual cycle in healthy reproductive-aged women. Fertil Steril. 2014; 101(5):1383–1391. PMID: 24581581.44. Maybin JA, Critchley HO. Progesterone: a pivotal hormone at menstruation. Ann N Y Acad Sci. 2011; 1221(1):88–97. PMID: 21401635.
Article45. Kannan P, Cheung KK, Lau BW. Does aerobic exercise induced-analgesia occur through hormone and inflammatory cytokine-mediated mechanisms in primary dysmenorrhea? Med Hypotheses. 2019; 123:50–54. PMID: 30696591.
Article46. Tavallaee M, Joffres MR, Corber SJ, Bayanzadeh M, Rad MM. The prevalence of menstrual pain and associated risk factors among Iranian women. J Obstet Gynaecol Res. 2011; 37(5):442–451. PMID: 21208343.
Article47. Wolfson JA, Bleich SN. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutr. 2015; 18(8):1397–1406. PMID: 25399031.
Article48. Bianco V, Cestari AM, Casati D, Cipriani S, Radici G, Valente I. Premenstrual syndrome and beyond: lifestyle, nutrition, and personal facts. Minerva Ginecol. 2014; 66(4):365–375. PMID: 25020055.49. Wang L, Wang X, Wang W, Chen C, Ronnennberg AG, Guang W, et al. Stress and dysmenorrhoea: a population based prospective study. Occup Environ Med. 2004; 61(12):1021–1026. PMID: 15550609.
Article50. Bajalan Z, Moafi F, MoradiBaglooei M, Alimoradi Z. Mental health and primary dysmenorrhea: a systematic review. J Psychosom Obstet Gynaecol. 2019; 40(3):185–194. PMID: 29745745.
Article51. Kitamura M, Takeda T, Koga S, Nagase S, Yaegashi N. Relationship between premenstrual symptoms and dysmenorrhea in Japanese high school students. Arch Women Ment Health. 2012; 15(2):131–133.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Analysis of Weight Control Behaviors by Body Image Perception among Korean Women in Different Age Groups: Using the 2010 Korea National Health and Nutrition Examination Survey Data
- The Relationship between Smoking and Unhealthy Weight Control Behaviors among Korean Adolescents: The Tenth Korea Youth Risk Behavior Web-Based Survey, 2014
- Weight Control Behaviors in Female College Students
- Effects of Body Weight Control Behaviors on Bone Mineral Density in Korean Young Adult Women
- The Effects of Actual and Perceived Body Weight on Unhealthy Weight Control Behaviors and Depressed Mood among Adult Women in Seoul, Korea