J Korean Med Sci.
2023 Apr;38(16):e130. 10.3346/jkms.2023.38.e130.
Relevance Index Regional Variation by Each Disease and Its Essential Medical Field: A Retrospective Data Analysis From 2016-2020 in Korea
- Affiliations
-
- 1Department of Big Data Strategy, National Health Insurance Service, Wonju, Korea
- 2Task Forces to Support Public Health and Medical Services in Ulsan Metropolitan City, Ulsan, Korea
- 3Department of Preventive Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 4Prevention and Management Center, Ulsan University Hospital, Ulsan, Korea
- 5Public Health and Medical Services Team, Ulsan University Hospital, Ulsan, Korea
- 6Department of Preventive Medicine, University of Ulsan College of Medicine, Seoul, Korea
- 7Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea
- KMID: 2541754
- DOI: http://doi.org/10.3346/jkms.2023.38.e130
Abstract
- Background
To precisely build a healthcare delivery system at regional levels, local patients’ healthcare service utilization patterns must be examined. Hence, this study utilized trend analysis of the relevance index of each disease of each essential medical service field at the municipal and provincial levels.
Methods
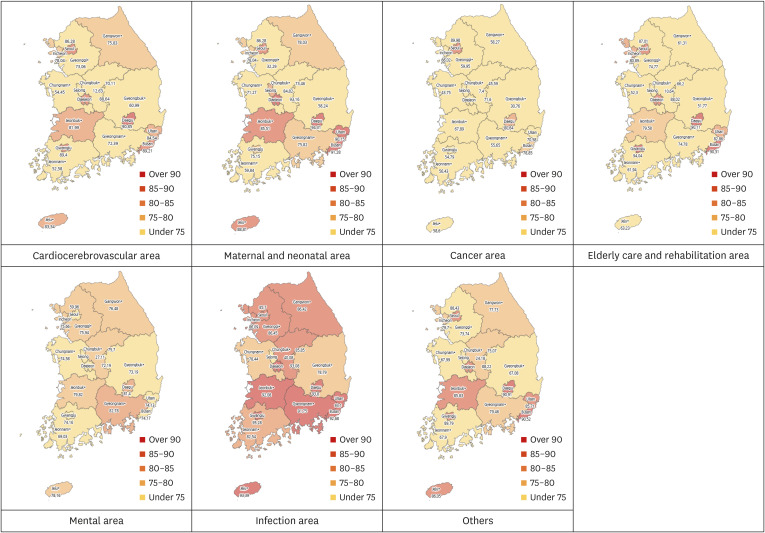
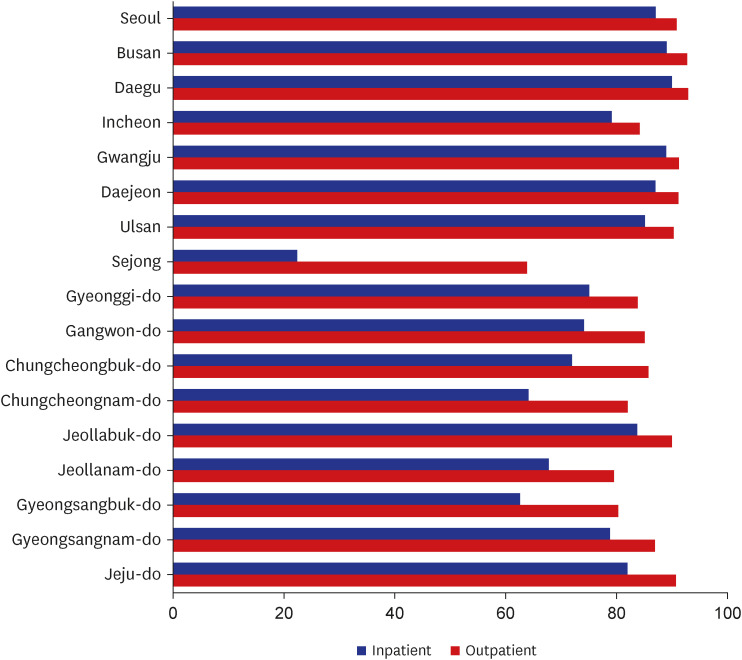
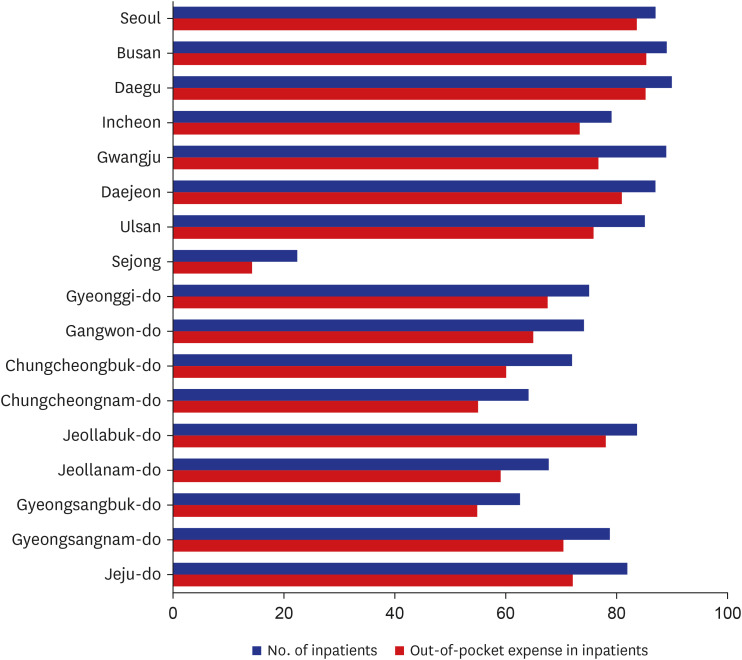
This study analyzed customized databases released by the National Health Insurance Service from 2016–2020. Diseases defined in the Korean National Burden of Disease (KNBD) study were categorized into the following essential medical service fields: trauma care, cardiocerebrovascular, maternal and neonatal, mental health, infection, cancer, older adults’ care and rehabilitation, and others. Relevance index, the percentage of medical service utilization in a region by the residents of that region relative to their total medical service utilization, was examined by region (17 municipal and provincial regions) and disease area. The relevance index was determined based on the number of patients and the total outof-pocket expenses. Result: Eight of the 17 regions showed over a 90.0% relevance index in the infection area. In the cancer area, 14 regions (not including Seoul, Daegu, and Busan) had a relevance index lower than 75.0%. Throughout the analysis period (2016–2020), there were no significant variations in the relevance index. Diseases such as bone and connective tissue cancer (39.0%), neural tube defects (16.7%), and autism (57.1%) had low relevance index in the essential medical service fields. In all 17 regions, the relevance index of inpatients was lower than that of outpatients, and that for out-of-pocket expenses was lower than that based on the number of patients.
Conclusion
The relevance index of major diseases of each essential medical service field calculated in this study can provide good indicators for monitoring the level of an independent regional healthcare delivery system.
Figure
Reference
-
1. Korean Statistical Information Service. Updated 2021. Accessed May 24, 2022. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B34E13&vw_cd=MT_ETITLE&list_id=F_27&scrId=&seqNo=&language=en&obj_var_id=&itm_id=&conn_path=A6&path=%252Feng%252Fsearch%252FsearchList.do .2. Kim YE, Jung YS, Ock M, Yoon SJ. A review of the types and characteristics of healthy life expectancy and methodological issues. J Prev Med Public Health. 2022; 55(1):1–9. PMID: 35135043.3. Lee JY, Ock M, Kim SH, Go DS, Kim HJ, Jo MW. Health-adjusted life expectancy (HALE) in Korea: 2005-2011. J Korean Med Sci. 2016; 31(Suppl 2):S139–S145. PMID: 27775251.4. Jo MW, Seo W, Lim SY, Ock M. The trends in health life expectancy in Korea according to age, gender, education level, and subregion: using quality-adjusted life expectancy method. J Korean Med Sci. 2018; 34(Suppl 1):e88. PMID: 30923491.5. Kim YE, Jung YS, Ock M, Park H, Kim KB, Go DS, et al. The gaps in health-adjusted life years (HALE) by income and region in Korea: a national representative bigdata analysis. Int J Environ Res Public Health. 2021; 18(7):3473. PMID: 33801588.6. World Health Organization. Essential medicines and pharmaceutical policies. Accessed May 24, 2022. http://www.emro.who.int/entity/essential-medicines/index.html .7. Ministry of Health and Welfare. Press release: eliminate regional gaps in essential medical services by strengthening public health care. Updated 2018. Accessed May 24, 2022. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=346233&page=1 .8. Ministry of Health and Welfare. Press release: receive essential hospital care in our area. Updated 2019. Accessed May 24, 2022. https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=351474 .9. Ministry of Health and Welfare. Press release: designated 8 additional responsible medical institutions for regional essential medical cooperation. Updated 2022. Accessed May 24, 2022. http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=371174 .10. Lee HY, Park MY. Analysis of the emergency medical service area using GIS: the case of Seoul. J GIS Assoc Korea. 2004; 12(2):193–209.11. Oh M, Lee JH, Jeon BU, Jeong TO, Heo T, Lee S. Usage patterns of emergency medical services in Korea: analysis of patient flow. Chin Med J (Engl). 2019; 132(3):259–268. PMID: 30681491.12. Oh MR, Jeon BG, Lee JH, Jeong TO, Heo T. Inflow and outflow type analysis of emergency department patients of the Honam region. J Korean Soc Emerg Med. 2019; 30(4):348–354.13. Park YK, Pyo J, Kim YE, Ock M, Yoon SJ. Analysis of relevance index by essential medical service field: a preliminary study on Ulsan metropolitan city. Korean Public Health Res. 2021; 47(2):133–148.14. Lee SM. Essential health care. J Korean Med Assoc. 2019; 62(4):231–237.15. Public Health and Medical Services Act. Accessed May 24, 2022. https://elaw.klri.re.kr/kor_service/lawView.do?hseq=53992&lang=ENG .16. Global Burden of Disease (GBD) 2020. Accessed May 24, 2022. https://www.healthdata.org/gbd/2019 .17. Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2019; 34(Suppl 1):e75. PMID: 30923488.18. National Health Insurance Sharing Service. Customized DB. Accessed May 24, 2022. https://nhiss.nhis.or.kr/bd/ab/bdaba032eng.do .19. The Korean Society for Preventive Medicine. Preventive Medicine and Public Health. 3rd ed. Seoul, Korea: Gyechuck Press;2019. p. 866.20. Health Map. Accessed May 24, 2022. http://www.healthmap.or.kr/ .21. Jung YS, Kim YE, Park H, Oh IH, Jo MW, Ock M, et al. Measuring the burden of disease in Korea, 2008-2018. J Prev Med Public Health. 2021; 54(5):293–300. PMID: 34649391.22. Basch E, Deal AM, Kris MG, Scher HI, Hudis CA, Sabbatini P, et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J Clin Oncol. 2016; 34(6):557–565. PMID: 26644527.23. Chang I, Kim BH. Regional disparity of medical resources and its effect on age-standardized mortality rates in Korea. Ann Reg Sci. 2019; 62(2):305–325.24. Regional Cancer Center Support Program. Accessed October 15, 2022. https://ncc.re.kr/main.ncc?uri=english/sub04_ControlPrograms05 .25. Bae JY, Hong SY. Program for obstetric care supporting underserved areas in Korea: outcome and evaluation standards. J Korean Med Assoc. 2016; 59(6):424–428.26. Lim K, Moon H, Park JS, Cho YR, Park K, Park TH, et al. The Busan Regional CardioCerebroVascular Center Project’s experience over a decade in the treatment of ST-segment elevation myocardial infarction. J Prev Med Public Health. 2022; 55(4):351–359. PMID: 35940190.27. Cho SG, Kim Y, Choi Y, Chung W. Impact of Regional CardioCerebroVascular Centers on myocardial infarction patients in Korea: a fixed-effects model. J Prev Med Public Health. 2019; 52(1):21–29. PMID: 30742758.28. Jang SY, Seon JY, Oh IH. Influencing factors of transportation costs regarding healthcare service utilization in Korea. J Korean Med Sci. 2020; 35(35):e290. PMID: 32893520.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Erratum: Correction of Authors in the Article “Relevance Index Regional Variation by Each Disease and Its Essential Medical Field: A Retrospective Data Analysis From 2016–2020 in Korea”
- Pattern of Regional Emergency Medical Service Utilization and Its Determinants
- Inflow and outflow type analysis of emergency department patients of the Honam region
- Imbalance in Cardiovascular Surgery Medical Service Use Between Regions
- Regional Variation of EQ-5D Index and Related Factors in Community Health Survey: Major Role of Psychosocial Factors in Korea