J Korean Med Sci.
2023 Apr;38(16):e128. 10.3346/jkms.2023.38.e128.
Differential Expression of NME4 in Trophoblast Stem-Like Cells and Peripheral Blood Mononuclear Cells of Normal Pregnancy and Preeclampsia
- Affiliations
-
- 1Division of Maternal Fetal Medicine, Department of Obstetrics and Gynecology, Severance Hospital, Yonsei University Medical College, Seoul, Korea
- 2Department of Rehabilitation Medicine and Research Institute of Rehabilitation Medicine, Severance Hospital, Yonsei University Medical College, Seoul, Korea
- KMID: 2541752
- DOI: http://doi.org/10.3346/jkms.2023.38.e128
Abstract
- Background
Preeclampsia (PE) is known to arise from insufficient trophoblast invasion as uterine spiral arteries lack remodeling. A significant reduction in placental perfusion induces an ischemic placental microenvironment due to reduced oxygen delivery to the placenta and fetus, leading to oxidative stress. Mitochondria are involved in the regulation of cellular metabolism and the production of reactive oxygen species (ROS). NME/NM23 nuceloside diphosphate kinase 4 (NME4) gene is known to have the ability to supply nucleotide triphosphate and deoxynucleotide triphosphate for replication and transcription of mitochondria. Our study aimed to investigate changes in NME4 expression in PE using trophoblast stem-like cells (TSLCs) from induced pluripotent stem cells (iPSCs) as a model of early pregnancy and peripheral blood mononuclear cells (PBMNCs) as a model of late preterm pregnancy.
Methods
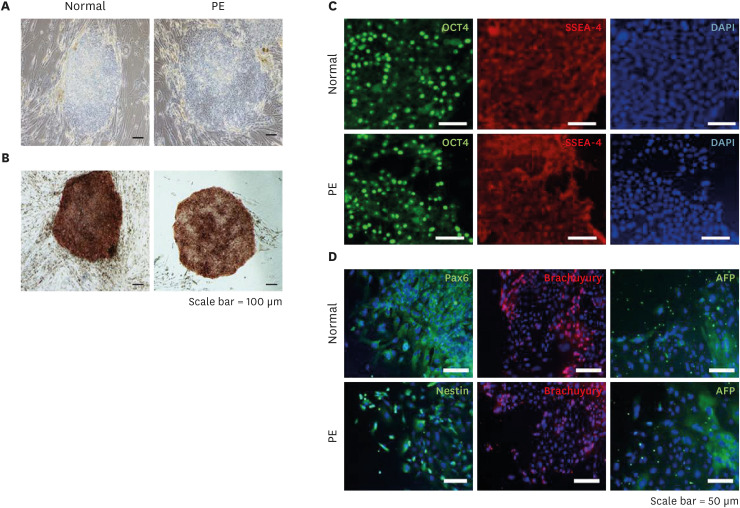
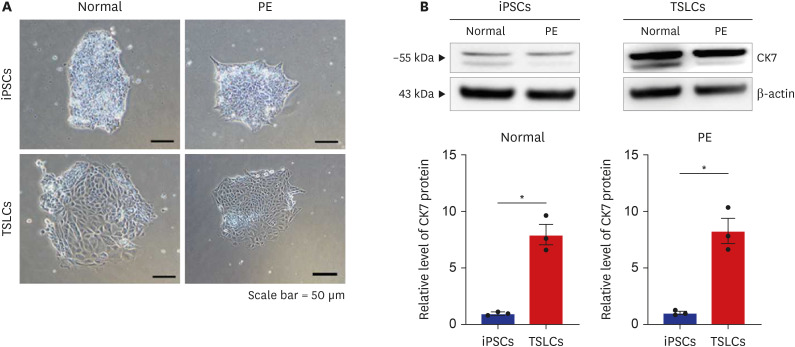
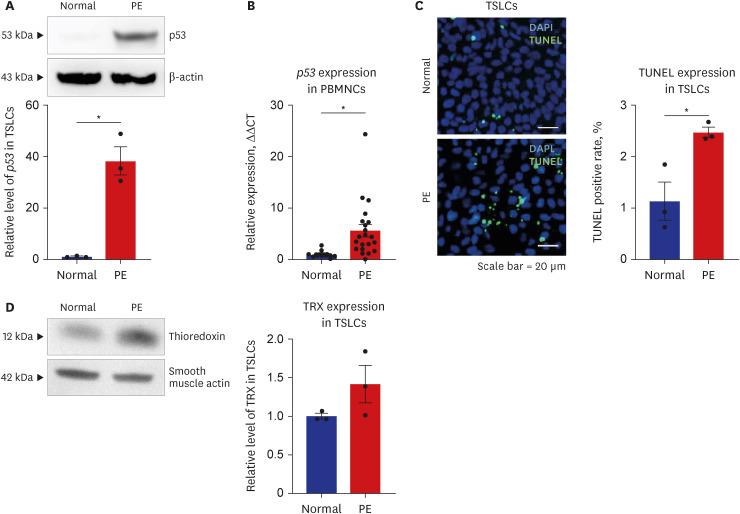
Transcriptome analysis using TSLCs was performed to identify the candidate gene associated with the possible pathophysiology of PE. Then, the expression of NME4 associated with mitochondrial function, p53 associated with cell death, and thioredoxin (TRX) linked to ROS were investigated through qRT-PCR, western blotting and deoxynucleotidyl transferase (TdT)-mediated deoxyuridine triphosphate (dUTP) nick end labelling (TUNEL) assay.
Results
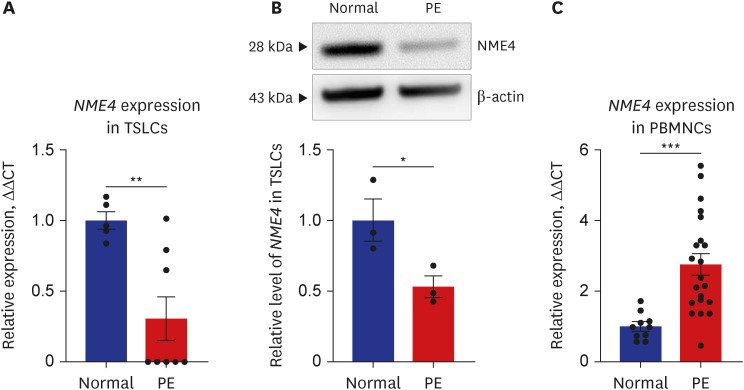
In patients with PE, NME4 was significantly downregulated in TSLCs but upregulated in PBMNCs. p53 was shown to be upregulated in TSLCs and PBMNCs of PE. In addition, western blot analysis confirmed that TRX expression had the tendency to increase in TSLCs of PE. Similarly, TUNEL analysis confirmed that the dead cells were higher in PE than in normal pregnancy.
Conclusion
Our study showed that the expression of the NME4 differed between models of early and late preterm pregnancy of PE, and suggests that this expression pattern may be a potential biomarker for early diagnosis of PE.
Keyword
Figure
Reference
-
1. Kim MS, Yu JH, Lee MY, Kim AL, Jo MH, Kim M, et al. Differential expression of extracellular matrix and adhesion molecules in fetal-origin amniotic epithelial cells of preeclamptic pregnancy. PLoS One. 2016; 11(5):e0156038. PMID: 27218821.2. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013; 122(5):1122–1131. PMID: 24150027.3. Wang D, Liu N, Tian Y, Li Y, Shen X, Chen Y, et al. Expression profile of Let-7s in peripheral blood mononuclear cells of normal and severe preeclampsia pregnant women. Exp Mol Pathol. 2019; 110:104263. PMID: 31128089.4. Say L, Chou D, Gemmill A, Tunçalp Ö, Moller AB, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob Health. 2014; 2(6):e323–e333. PMID: 25103301.5. Zuo Q, Zou Y, Huang S, Wang T, Xu Y, Zhang T, et al. Aspirin reduces sFlt-1-mediated apoptosis of trophoblast cells in preeclampsia. Mol Hum Reprod. 2021; 27(1):gaaa089. PMID: 33493277.6. Raymond D, Peterson E. A critical review of early-onset and late-onset preeclampsia. Obstet Gynecol Surv. 2011; 66(8):497–506. PMID: 22018452.7. Horii M, Morey R, Bui T, Touma O, Nelson KK, Cho HY, et al. Modeling preeclampsia using human induced pluripotent stem cells. Sci Rep. 2021; 11(1):5877. PMID: 33723311.8. Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R. Pre-eclampsia. Lancet. 2010; 376(9741):631–644. PMID: 20598363.9. Wadhwani P, Saha PK, Kalra JK, Gainder S, Sundaram V. A study to compare maternal and perinatal outcome in early vs. late onset preeclampsia. Obstet Gynecol Sci. 2020; 63(3):270–277. PMID: 32489971.10. Jang YJ, Kim M, Lee BK, Kim J. Induction of human trophoblast stem-like cells from primed pluripotent stem cells. Proc Natl Acad Sci U S A. 2022; 119(20):e2115709119. PMID: 35537047.11. Kojima J, Fukuda A, Taira H, Kawasaki T, Ito H, Kuji N, et al. Efficient production of trophoblast lineage cells from human induced pluripotent stem cells. Lab Invest. 2017; 97(10):1188–1200. PMID: 28287635.12. Sheridan MA, Yang Y, Jain A, Lyons AS, Yang P, Brahmasani SR, et al. Early onset preeclampsia in a model for human placental trophoblast. Proc Natl Acad Sci U S A. 2019; 116(10):4336–4345. PMID: 30787190.13. Rajakumar A, Chu T, Handley DE, Bunce KD, Burke B, Hubel CA, et al. Maternal gene expression profiling during pregnancy and preeclampsia in human peripheral blood mononuclear cells. Placenta. 2011; 32(1):70–78. PMID: 21075447.14. Okazaki S, Sekizawa A, Purwosunu Y, Farina A, Wibowo N, Okai T. Placenta-derived, cellular messenger RNA expression in the maternal blood of preeclamptic women. Obstet Gynecol. 2007; 110(5):1130–1136. PMID: 17978129.15. Sun CJ, Zhang L, Zhang WY. Gene expression profiling of maternal blood in early onset severe preeclampsia: identification of novel biomarkers. J Perinat Med. 2009; 37(6):609–616. PMID: 19681734.16. Chaiworapongsa T, Chaemsaithong P, Yeo L, Romero R. Pre-eclampsia part 1: current understanding of its pathophysiology. Nat Rev Nephrol. 2014; 10(8):466–480. PMID: 25003615.17. Burton GJ, Redman CW, Roberts JM, Moffett A. Pre-eclampsia: pathophysiology and clinical implications. BMJ. 2019; 366:l2381. PMID: 31307997.18. Wang Z, Zhao G, Zibrila AI, Li Y, Liu J, Feng W. Acetylcholine ameliorated hypoxia-induced oxidative stress and apoptosis in trophoblast cells via p38 MAPK/NF-κB pathway. Mol Hum Reprod. 2021; 27(8):gaab045. PMID: 34245298.19. Marín R, Chiarello DI, Abad C, Rojas D, Toledo F, Sobrevia L. Oxidative stress and mitochondrial dysfunction in early-onset and late-onset preeclampsia. Biochim Biophys Acta Mol Basis Dis. 2020; 1866(12):165961. PMID: 32916282.20. Levy R. The role of apoptosis in preeclampsia. Isr Med Assoc J. 2005; 7(3):178–181. PMID: 15792265.21. Tomas SZ, Prusac IK, Roje D, Tadin I. Trophoblast apoptosis in placentas from pregnancies complicated by preeclampsia. Gynecol Obstet Invest. 2011; 71(4):250–255. PMID: 21266791.22. ACOG Committee on Practice Bulletins--Obstetrics. ACOG practice bulletin. Diagnosis and management of preeclampsia and eclampsia. Number 33, January 2002. Obstet Gynecol. 2002; 99(1):159–167. PMID: 16175681.23. Lee JK, Jang HL, Kang BH, Lee KS, Choi YS, Shim KS, et al. Percentile distributions of birth weight according to gestational ages in Korea (2010-2012). J Korean Med Sci. 2016; 31(6):939–949. PMID: 27247504.24. Vogelstein B, Lane D, Levine AJ. Surfing the p53 network. Nature. 2000; 408(6810):307–310. PMID: 11099028.25. Gao Q, Zhu X, Chen J, Mao C, Zhang L, Xu Z. Upregulation of P53 promoted G1 arrest and apoptosis in human umbilical cord vein endothelial cells from preeclampsia. J Hypertens. 2016; 34(7):1380–1388. PMID: 27115339.26. Kobayashi F, Sagawa N, Nanbu Y, Kitaoka Y, Mori T, Fujii S, et al. Biochemical and topological analysis of adult T-cell leukaemia-derived factor, homologous to thioredoxin, in the pregnant human uterus. Hum Reprod. 1995; 10(6):1603–1608. PMID: 7593543.27. Takagi Y, Nikaido T, Toki T, Kita N, Kanai M, Ashida T, et al. Levels of oxidative stress and redox-related molecules in the placenta in preeclampsia and fetal growth restriction. Virchows Arch. 2004; 444(1):49–55. PMID: 14574573.28. Mogami H, Yura S, Kondoh E, Masutani H, Yodoi J, Konishi I. Differential expression of thioredoxin binding protein-2/Txnip in human placenta: Possible involvement of hypoxia in its suppression during early pregnancy. J Obstet Gynaecol Res. 2017; 43(1):50–56. PMID: 27762463.29. Martinez-Fierro ML, Hernández-Delgadillo GP, Flores-Morales V, Cardenas-Vargas E, Mercado-Reyes M, Rodriguez-Sanchez IP, et al. Current model systems for the study of preeclampsia. Exp Biol Med (Maywood). 2018; 243(6):576–585. PMID: 29415560.30. Tsuchida N, Kojima J, Fukuda A, Oda M, Kawasaki T, Ito H, et al. Transcriptomic features of trophoblast lineage cells derived from human induced pluripotent stem cells treated with BMP 4. Placenta. 2020; 89:20–32. PMID: 31675487.31. Shanklin DR, Sibai BM. Ultrastructural aspects of preeclampsia. II. Mitochondrial changes. Am J Obstet Gynecol. 1990; 163(3):943–953. PMID: 2403173.32. Sulbarán TA, Castellano A, Chacín L, Vergel C, Portillo MA, Urbina E, et al. Electron microscopy of umbilical cord endothelial cells in preeclampsia. J Submicrosc Cytol Pathol. 2002; 34(4):389–395. PMID: 12585229.33. Salgado SS. M K R Salgado. Structural changes in pre-eclamptic and eclamptic placentas--an ultrastructural study. J Coll Physicians Surg Pak. 2011; 21(8):482–486. PMID: 21798135.34. Vaka VR, McMaster KM, Cunningham MW Jr, Ibrahim T, Hazlewood R, Usry N, et al. Role of mitochondrial dysfunction and reactive oxygen species in mediating hypertension in the reduced uterine perfusion pressure rat model of preeclampsia. Hypertension. 2018; 72(3):703–711. PMID: 30012871.35. Boveris A, Chance B. The mitochondrial generation of hydrogen peroxide. General properties and effect of hyperbaric oxygen. Biochem J. 1973; 134(3):707–716. PMID: 4749271.36. Nohl H, Jordan W. The metabolic fate of mitochondrial hydrogen peroxide. Eur J Biochem. 1980; 111(1):203–210. PMID: 7439185.37. Turrens JF, Beconi M, Barilla J, Chavez UB, McCord JM. Mitochondrial generation of oxygen radicals during reoxygenation of ischemic tissues. Free Radic Res Commun. 1991; 12-13 Pt 2:681–689.38. Furui T, Kurauchi O, Tanaka M, Mizutani S, Ozawa T, Tomoda Y. Decrease in cytochrome c oxidase and cytochrome oxidase subunit I messenger RNA levels in preeclamptic pregnancies. Obstet Gynecol. 1994; 84(2):283–288. PMID: 8041548.39. Smith AN, Wang X, Thomas DG, Tatum RE, Booz GW, Cunningham MW Jr. The role of mitochondrial dysfunction in preeclampsia: causative factor or collateral damage? Am J Hypertens. 2021; 34(5):442–452. PMID: 33417666.40. Davidson SM, Yellon DM. Mitochondrial DNA damage, oxidative stress, and atherosclerosis: where there is smoke there is not always fire. Circulation. 2013; 128(7):681–683. PMID: 23841982.41. Zhang R, Du J, Xiao Z, Jiang Y, Jin L, Weng Q. Association between the peripartum maternal and fetal telomere lengths and mitochondrial DNA copy numbers and preeclampsia: a prospective case-control study. BMC Pregnancy Childbirth. 2022; 22(1):483. PMID: 35698093.42. Lee HC, Wei YH. Mitochondrial biogenesis and mitochondrial DNA maintenance of mammalian cells under oxidative stress. Int J Biochem Cell Biol. 2005; 37(4):822–834. PMID: 15694841.43. Lee HC, Yin PH, Lu CY, Chi CW, Wei YH. Increase of mitochondria and mitochondrial DNA in response to oxidative stress in human cells. Biochem J. 2000; 348 Pt 2(Pt 2):425–432. PMID: 10816438.44. Wang X, Hart JE, Liu Q, Wu S, Nan H, Laden F. Corrigendum to “Association of particulate matter air pollution with leukocyte mitochondrial DNA copy number” [Environ. Int. 141 (2020) 105761]. Environ Int. 2020; 143:106069. PMID: 32854974.45. Milon L, Meyer P, Chiadmi M, Munier A, Johansson M, Karlsson A, et al. The human Nm23-H4 gene product is a mitochondrial nucleoside diphosphate kinase. J Biol Chem. 2000; 275(19):14264–14272. PMID: 10799505.46. Tokarska-Schlattner M, Boissan M, Munier A, Borot C, Mailleau C, Speer O, et al. The nucleoside diphosphate kinase D (Nm23-H4) binds the inner mitochondrial membrane with high affinity to cardiolipin and couples nucleotide transfer with respiration. J Biol Chem. 2008; 283(38):26198–26207. PMID: 18635542.47. Yang JI, Kong TW, Kim HS, Kim HY. The proteomic analysis of human placenta with pre-eclampsia and normal pregnancy. J Korean Med Sci. 2015; 30(6):770–778. PMID: 26028931.48. Hawfield A, Freedman BI. Pre-eclampsia: the pivotal role of the placenta in its pathophysiology and markers for early detection. Ther Adv Cardiovasc Dis. 2009; 3(1):65–73. PMID: 19124387.49. Roberts JM, Hubel CA. The two stage model of preeclampsia: variations on the theme. Placenta. 2009; 30 Suppl A(Suppl A):S32–S37. PMID: 19070896.50. Rose S, Carvalho E, Diaz EC, Cotter M, Bennuri SC, Azhar G, et al. A comparative study of mitochondrial respiration in circulating blood cells and skeletal muscle fibers in women. Am J Physiol Endocrinol Metab. 2019; 317(3):E503–E512. PMID: 31211617.51. Petrus AT, Lighezan DL, Danila MD, Duicu OM, Sturza A, Muntean DM, et al. Assessment of platelet respiration as emerging biomarker of disease. Physiol Res. 2019; 68(3):347–363. PMID: 30904011.52. Ost M, Doerrier C, Gama-Perez P, Moreno-Gomez S. Analysis of mitochondrial respiratory function in tissue biopsies and blood cells. Curr Opin Clin Nutr Metab Care. 2018; 21(5):336–342. PMID: 29939971.53. Kramer PA, Ravi S, Chacko B, Johnson MS, Darley-Usmar VM. A review of the mitochondrial and glycolytic metabolism in human platelets and leukocytes: implications for their use as bioenergetic biomarkers. Redox Biol. 2014; 2:206–210. PMID: 24494194.54. Maestraggi Q, Lebas B, Clere-Jehl R, Ludes PO, Chamaraux-Tran TN, Schneider F, et al. Skeletal muscle and lymphocyte mitochondrial dysfunctions in septic shock trigger ICU-acquired weakness and sepsis-induced immunoparalysis. BioMed Res Int. 2017; 2017:7897325. PMID: 28589148.55. Weiss SL, Selak MA, Tuluc F, Perales Villarroel J, Nadkarni VM, Deutschman CS, et al. Mitochondrial dysfunction in peripheral blood mononuclear cells in pediatric septic shock. Pediatr Crit Care Med. 2015; 16(1):e4–12. PMID: 25251517.56. Maynard S, Keijzers G, Gram M, Desler C, Bendix L, Budtz-Jørgensen E, et al. Relationships between human vitality and mitochondrial respiratory parameters, reactive oxygen species production and dNTP levels in peripheral blood mononuclear cells. Aging (Albany NY). 2013; 5(11):850–864. PMID: 24304678.57. Alfatni A, Riou M, Charles AL, Meyer A, Barnig C, Andres E, et al. Peripheral blood mononuclear cells and platelets mitochondrial dysfunction, oxidative stress, and circulating mtDNA in cardiovascular diseases. J Clin Med. 2020; 9(2):311. PMID: 31979097.58. Castejón O. Mithocondrial disfunction and apoptosis in trophoblast cells during preeclampsia: an ultrastructural study. Revista Electrónica de Biomedicina. 2011; 2:30–38.59. Robinson NJ, Wareing M, Hudson NK, Blankley RT, Baker PN, Aplin JD, et al. Oxygen and the liberation of placental factors responsible for vascular compromise. Lab Invest. 2008; 88(3):293–305. PMID: 18227808.60. Li G, Wang Y, Cao G, Ma Y, Li YX, Zhao Y, et al. Hypoxic stress disrupts HGF/Met signaling in human trophoblasts: implications for the pathogenesis of preeclampsia. J Biomed Sci. 2022; 29(1):8. PMID: 35114998.61. Guerby P, Tasta O, Swiader A, Pont F, Bujold E, Parant O, et al. Role of oxidative stress in the dysfunction of the placental endothelial nitric oxide synthase in preeclampsia. Redox Biol. 2021; 40:101861. PMID: 33548859.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Expressions of Neural Cell Adhesion Molecule ( NCAM ) in the Endovascular Trophoblasts ; Comparison of Normal Pregnancy and Recurrent Abortion
- Comparison of Placental Apoptosis in Normal Pregnancy, Preeclampsia and Intrauterine Growth Restriction
- Expression of Immortalization-upregulated Proteins-2 (IMUP-2) in Placenta
- Effect of Hypoxia-induced XIAP Expression on Apoptosis of Trophoblast Cells in Placenta
- Mixed Mononuclear Cell Culture of Cord Blood and Adult Peripheral Blood