J Korean Med Sci.
2023 Apr;38(16):e127. 10.3346/jkms.2023.38.e127.
Twenty-Five Year Trend Change in the Etiology of Pediatric Invasive Bacterial Infections in Korea, 1996–2020
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Hospital, Seoul, Korea
- 2Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Pediatrics, Chonnam National University Medical School, Gwangju, Korea
- 5Department of Pediatrics, Severance Children’s Hospital, Yonsei University College of Medicine, Seoul, Korea
- 6Department of Pediatrics, Pusan National University College of Medicine, Yangsan, Korea
- 7Department of Pediatrics, CHA Bundang Medical Center, CHA University, Seongnam, Korea
- 8Department of Pediatrics, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 9Department of Pediatrics, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea
- 10Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 11Department of Pediatrics, Jeonbuk National University Medical School, Jeonju, Korea
- 12Department of Pediatrics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 13Department of Pediatrics, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea
- 14Department of Pediatrics, Keimyung University School of Medicine, Daegu, Korea
- 15Department of Pediatrics, Inha University College of Medicine, Incheon, Korea
- 16Department of Pediatrics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 17Department of Pediatrics, Jeju National University School of Medicine, Jeju, Korea
- 18Department of Pediatrics, Eulji University School of Medicine, Nowon Eulji University Hospital, Seoul, Korea
- 19Department of Pediatrics, Inje University Ilsan Paik Hospital, Goyang, Korea
- 20Department of Pediatrics, Chungnam National University Hospital, Daejeon, Korea
- 21Department of Pediatrics, Korea University College of Medicine, Seoul, Korea
- 22Department of Pediatrics, Kosin University Gospel Hospital, Busan, Korea
- 23Department of Pediatrics, College of Medicine, Ewha Womans University, Seoul, Korea
- 24Department of Pediatrics, Fatima Hospital, Changwon, Korea
- 25Department of Pediatrics, Ajou University Hospital, Ajou University School of Medicine, Suwon, Korea
- 26Department of Pediatrics, Dankook University College of Medicine, Cheonan, Korea
- 27Department of Pediatrics, Hallym University Sacred Heart Hospital, Anyang, Korea
- KMID: 2541751
- DOI: http://doi.org/10.3346/jkms.2023.38.e127
Abstract
- Background
The coronavirus disease-2019 (COVID-19) pandemic has contributed to the change in the epidemiology of many infectious diseases. This study aimed to establish the pre-pandemic epidemiology of pediatric invasive bacterial infection (IBI).
Methods
A retrospective multicenter-based surveillance for pediatric IBIs has been maintained from 1996 to 2020 in Korea. IBIs caused by eight bacteria (Streptococcus pneumoniae, Haemophilus influenzae, Neisseria meningitidis, Staphylococcus aureus, Streptococcus agalactiae, Streptococcus pyogenes, Listeria monocytogenes, and Salmonella species) in immunocompetent children > 3 months of age were collected at 29 centers. The annual trend in the proportion of IBIs by each pathogen was analyzed.
Results
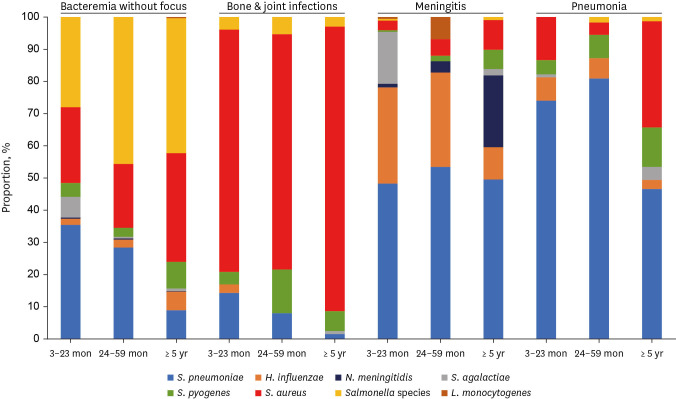
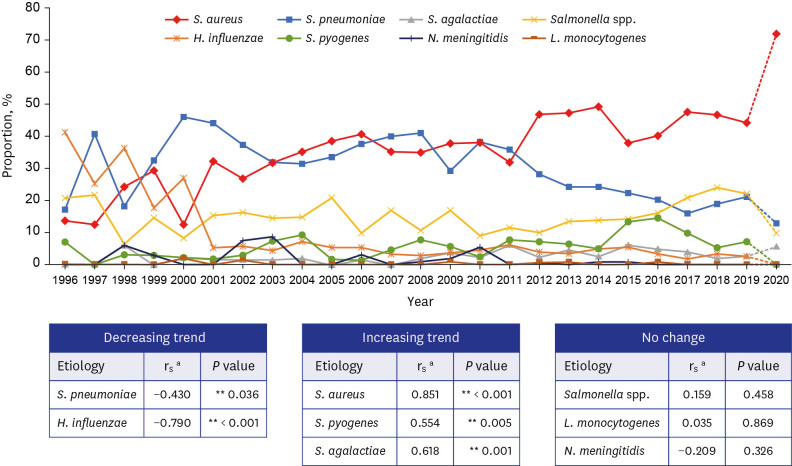
A total of 2,195 episodes were identified during the 25-year period between 1996 and 2020. S. pneumoniae (42.4%), S. aureus (22.1%), and Salmonella species (21.0%) were common in children 3 to 59 months of age. In children ≥ 5 years of age, S. aureus (58.1%), followed by Salmonella species (14.8%) and S. pneumoniae (12.2%) were common. Excluding the year 2020, there was a trend toward a decrease in the relative proportions of S. pneumoniae (rs = −0.430, P = 0.036), H. influenzae (rs = −0.922, P < 0.001), while trend toward an increase in the relative proportion of S. aureus (rs = 0.850, P < 0.001), S. agalactiae (rs = 0.615, P = 0.001), and S. pyogenes (rs = 0.554, P = 0.005).
Conclusion
In the proportion of IBIs over a 24-year period between 1996 and 2019, we observed a decreasing trend for S. pneumoniae and H. influenzae and an increasing trend for S. aureus, S. agalactiae, and S. pyogenes in children > 3 months of age. These findings can be used as the baseline data to navigate the trend in the epidemiology of pediatric IBI in the post COVID-19 era.
Figure
Reference
-
1. Lee JH, Cho HK, Kim KH, Kim CH, Kim DS, Kim KN, et al. Etiology of invasive bacterial infections in immunocompetent children in Korea (1996–2005): a retrospective multicenter study. J Korean Med Sci. 2011; 26(2):174–183. PMID: 21286006.2. Rhie K, Choi EH, Cho EY, Lee J, Kang JH, Kim DS, et al. Etiology of invasive bacterial infections in immunocompetent children in Korea (2006–2010): a retrospective multicenter study. J Korean Med Sci. 2018; 33(6):e45. PMID: 29349940.3. Hatoun J, Correa ET, Donahue SM, Vernacchio L. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics. 2020; 146(4):e2020006460. PMID: 32879032.4. Huh K, Jung J, Hong J, Kim M, Ahn JG, Kim JH, et al. Impact of non-pharmaceutical interventions on the incidence of respiratory infections during the COVID-19 outbreak in Korea: a nationwide surveillance study. Clin Infect Dis. 2021; 72(7):e184–e191. PMID: 33150393.5. Lee H, Lee H, Song KH, Kim ES, Park JS, Jung J, et al. Impact of public health interventions on seasonal influenza activity during the COVID-19 outbreak in Korea. Clin Infect Dis. 2021; 73(1):e132–e140. PMID: 32472687.6. Nolen LD, Seeman S, Bruden D, Klejka J, Desnoyers C, Tiesinga J, et al. Impact of social distancing and travel restrictions on non–coronavirus disease 2019 (non–COVID-19) respiratory hospital admissions in young children in Rural Alaska. Clin Infect Dis. 2021; 72(12):2196–2198. PMID: 32888007.7. Brueggemann AB, Jansen van Rensburg MJ, Shaw D, McCarthy ND, Jolley KA, Maiden MC, et al. Changes in the incidence of invasive disease due to Streptococcus pneumoniae, Haemophilus influenzae, and Neisseria meningitidis during the COVID-19 pandemic in 26 countries and territories in the Invasive Respiratory Infection Surveillance Initiative: a prospective analysis of surveillance data. Lancet Digit Health. 2021; 3(6):e360–e370. PMID: 34045002.8. Smith DR, Opatowski L. COVID-19 containment measures and incidence of invasive bacterial disease. Lancet Digit Health. 2021; 3(6):e331–e332. PMID: 34044998.9. Lee JH, Song EK, Lee JA, Kim NH, Kim DH, Park KW, et al. Clinical entities and etiology of invasive bacterial infections in apparently healthy children. Korean J Pediatr. 2005; 48(11):1193–1200.10. Nam SG, Lee HJ. Etiology of invasive bacterial infections in apparently healthy children. Korean J Infect Dis. 1998; 30(3):227–234.11. Morris SK, Moss WJ, Halsey N. Haemophilus influenzae type b conjugate vaccine use and effectiveness. Lancet Infect Dis. 2008; 8(7):435–443. PMID: 18582836.12. Suga S, Ishiwada N, Sasaki Y, Akeda H, Nishi J, Okada K, et al. A nationwide population-based surveillance of invasive Haemophilus influenzae diseases in children after the introduction of the Haemophilus influenzae type b vaccine in Japan. Vaccine. 2018; 36(38):5678–5684. PMID: 30122645.13. Choi EH, Park SE, Kim YJ, Jo DS, Kim YK, Eun BW, et al. Recommended immunization schedule for children and adolescents: Committee on Infectious Diseases of the Korean Pediatric Society, 2018. Korean J Pediatr. 2019; 62(7):252–256. PMID: 31163961.14. Lee J, Jeong H, Kim S, Yu J, Kim G. National childhood vaccination coverage among children aged 1–3 and 6 years in Korea, 2018. Public Health Wkly Rep. 2019; 12(39):1548–1558.15. Cho EY, Kang HM, Lee J, Kang JH, Choi EH, Lee HJ. Changes in serotype distribution and antibiotic resistance of nasopharyngeal isolates of Streptococcus pneumoniae from children in Korea, after optional use of the 7-valent conjugate vaccine. J Korean Med Sci. 2012; 27(7):716–722. PMID: 22787364.16. Lee JK, Yun KW, Choi EH, Kim SJ, Lee SY, Lee HJ. Changes in the serotype distribution among antibiotic resistant carriage Streptococcus pneumoniae isolates in children after the introduction of the extended-valency pneumococcal conjugate vaccine. J Korean Med Sci. 2017; 32(9):1431–1439. PMID: 28776337.17. Korea Centers for Disease Control and Prevention (KCDC). National Childhood Vaccination Coverage Among Children Aged 1–3 Years in Korea, 2017. Cheongju, Korea: KCDC;2018.18. Savulescu C, Krizova P, Lepoutre A, Mereckiene J, Vestrheim DF, Ciruela P, et al. Effect of high-valency pneumococcal conjugate vaccines on invasive pneumococcal disease in children in SpIDnet countries: an observational multicentre study. Lancet Respir Med. 2017; 5(8):648–656. PMID: 28359798.19. Lai CC, Lin SH, Liao CH, Sheng WH, Hsueh PR. Decline in the incidence of invasive pneumococcal disease at a medical center in Taiwan, 2000–2012. BMC Infect Dis. 2014; 14(1):76. PMID: 24512501.20. Tan TQ. Pediatric invasive pneumococcal disease in the United States in the era of pneumococcal conjugate vaccines. Clin Microbiol Rev. 2012; 25(3):409–419. PMID: 22763632.21. Waight PA, Andrews NJ, Ladhani SN, Sheppard CL, Slack MP, Miller E. Effect of the 13-valent pneumococcal conjugate vaccine on invasive pneumococcal disease in England and Wales 4 years after its introduction: an observational cohort study. Lancet Infect Dis. 2015; 15(5):535–543. PMID: 25801458.22. McMullan BJ, Bowen A, Blyth CC, Van Hal S, Korman TM, Buttery J, et al. Epidemiology and mortality of Staphylococcus aureus bacteremia in Australian and New Zealand children. JAMA Pediatr. 2016; 170(10):979–986. PMID: 27533601.23. Ochoa TJ, Mohr J, Wanger A, Murphy JR, Heresi GP. Community-associated methicillin-resistant Staphylococcus aureus in pediatric patients. Emerg Infect Dis. 2005; 11(6):966–968. PMID: 15963299.24. Sutter DE, Milburn E, Chukwuma U, Dzialowy N, Maranich AM, Hospenthal DR. Changing susceptibility of Staphylococcus aureus in a US pediatric population. Pediatrics. 2016; 137(4):e20153099. PMID: 26933211.25. Park DA, Lee SM, Peck KR, Joo EJ, Oh EG. Impact of methicillin-resistance on mortality in children and neonates with Staphylococcus aureus bacteremia: a meta-analysis. Infect Chemother. 2013; 45(2):202–210. PMID: 24265968.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Entities and Etiology of Invasive Bacterial Infections in Apparently Healthy Children
- Population-Based Epidemiologic Studies of Invasive Bacterial Infections in Korea
- Group A Streptococcal Meningitis Occurring in a Heathy 43-day-old Infant
- Trends in Childhood Bacterial Infectious Diseases in the Republic of Korea
- Trends of the Bacterial Skin Infections of Dermatology Outpatients in 1996, 2001 and 2006