J Korean Med Sci.
2023 Apr;38(16):e124. 10.3346/jkms.2023.38.e124.
Gender Difference of Blood Pressure Control Rate and Clinical Prognosis in Patients With Resistant Hypertension: Real-World Observation Study
- Affiliations
-
- 1Department of Medical Informatics, Korea University College of Medicine, Seoul, Korea
- 2Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea
- 3Department of Biostatistics, Korea University College of Medicine, Seoul, Korea
- 4Division of Cardiology, Department of Internal Medicine, Korea University Ansan Hospital, Ansan, Korea
- 5Department of Cardiology, Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 6Division of Cardiology, Department of Internal Medicine, Konkuk University Medical Center, Seoul, Korea
- 7Division of Cardiology, Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea
- 8Division of Cardiology, Hallym University Dongtan Sacred Heart Hospital, Hallym University College of Medicine, Hwaseong, Korea
- 9Division of Cardiology, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 10Division of Cardiology, Department of Internal Medicine, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea
- 11Division of Cardiology, Department of Internal Medicine, Korea University Guro Hospital, Seoul, Korea
- KMID: 2541749
- DOI: http://doi.org/10.3346/jkms.2023.38.e124
Abstract
- Background
There are several differences in the clinical course of hypertension due to the biological and social differences between men and women. Resistant hypertension is an advanced disease state, and significant gender difference could be expected, but much has not been revealed yet. The purpose of this study was to compare gender differences on the current status of blood pressure (BP) control and clinical prognosis in patients with resistant hypertension.
Methods
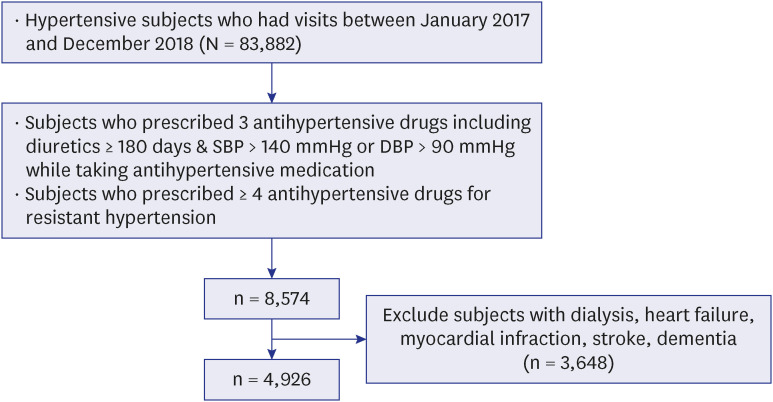
This is a multicenter, retrospective cohort study using common data model databases of 3 tertiary hospitals in Korea. Total 4,926 patients with resistant hypertension were selected from January 2017 to December 2018. Occurrence of dialysis, heart failure (HF) hospitalization, myocardial infarction, stroke, dementia or all-cause mortality was followed up for 3 years.
Results
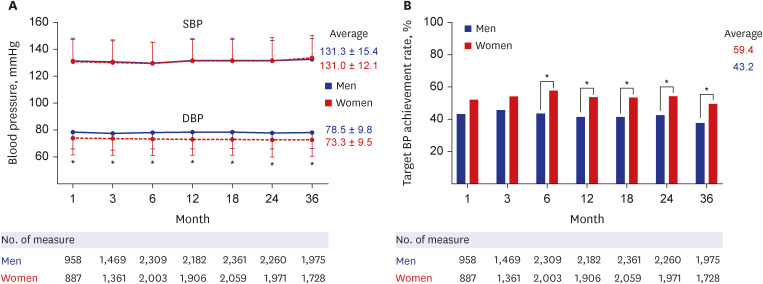
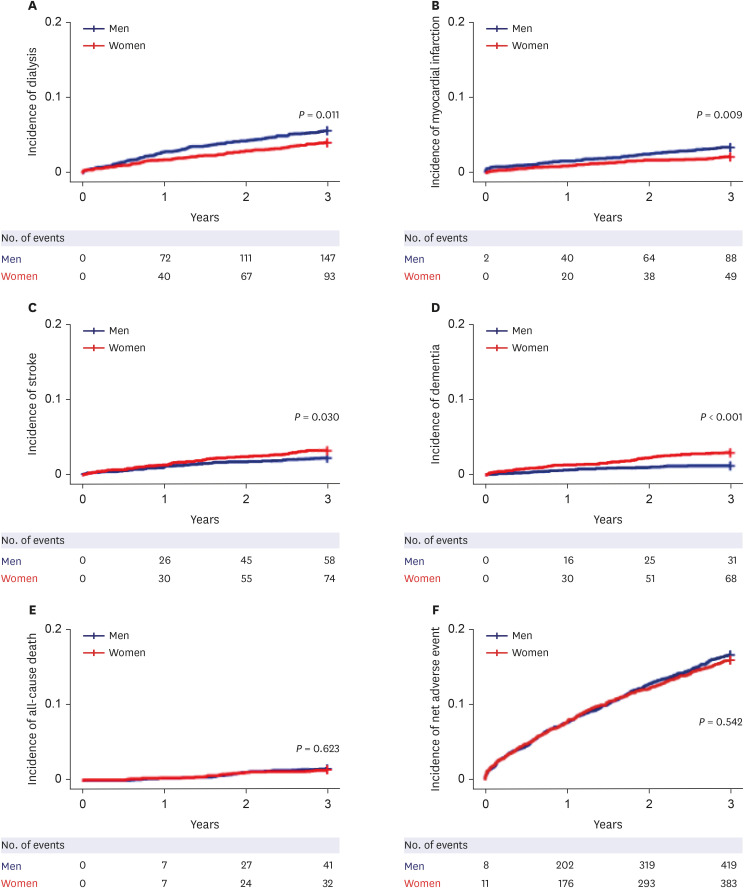
Male patients with resistant hypertension were younger but had a higher cardiovascular risk than female patients. Prevalence of left ventricular hypertrophy and proteinuria was higher in men than in women. On-treatment diastolic BP was lower in women than in men and target BP achievement rate was higher in women than in men. During 3 years, the incidence of dialysis and myocardial infarction was higher in men, and the incidence of stroke and dementia was higher in women. After adjustment, male sex was an independent risk factor for HF hospitalization, myocardial infarction, and all-cause death.
Conclusion
In resistant hypertension, men were younger than women, but end-organ damage was more common and the risk of cardiovascular event was higher. More intensive cardiovascular prevention strategies may be required in male patients with resistant hypertension.
Keyword
Figure
Reference
-
1. Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension. 2020; 75(2):285–292. PMID: 31865786.2. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International Society of Hypertension global hypertension practice guidelines. Hypertension. 2020; 75(6):1334–1357. PMID: 32370572.3. Noubiap JJ, Nansseu JR, Nyaga UF, Sime PS, Francis I, Bigna JJ. Global prevalence of resistant hypertension: a meta-analysis of data from 3.2 million patients. Heart. 2019; 105(2):98–105. PMID: 30087099.4. Pimenta E, Calhoun DA. Resistant hypertension: incidence, prevalence, and prognosis. Circulation. 2012; 125(13):1594–1596. PMID: 22379111.5. Achelrod D, Wenzel U, Frey S. Systematic review and meta-analysis of the prevalence of resistant hypertension in treated hypertensive populations. Am J Hypertens. 2015; 28(3):355–361. PMID: 25156625.6. Lee KN, Na JO, Choi CU, Lim HE, Kim JW, Kim EJ, et al. Prevalence and characteristics of resistant hypertension at primary clinics in Korea: a nationwide cross-sectional study. Clin Hypertens. 2016; 22(1):4. PMID: 26893938.7. Smith SM, Gong Y, Handberg E, Messerli FH, Bakris GL, Ahmed A, et al. Predictors and outcomes of resistant hypertension among patients with coronary artery disease and hypertension. J Hypertens. 2014; 32(3):635–643. PMID: 24299915.8. Kaczmarski KR, Sozio SM, Chen J, Sang Y, Shafi T. Resistant hypertension and cardiovascular disease mortality in the US: results from the National Health and Nutrition Examination Survey (NHANES). BMC Nephrol. 2019; 20(1):138. PMID: 31023262.9. Zhao M, Woodward M, Vaartjes I, Millett ER, Klipstein-Grobusch K, Hyun K, et al. Sex differences in cardiovascular medication prescription in primary care: a systematic review and meta-analysis. J Am Heart Assoc. 2020; 9(11):e014742. PMID: 32431190.10. Brugts JJ, Arima H, Remme W, Bertrand M, Ferrari R, Fox K, et al. The incidence and clinical predictors of ACE-inhibitor induced dry cough by perindopril in 27,492 patients with vascular disease. Int J Cardiol. 2014; 176(3):718–723. PMID: 25189490.11. Na SH, Lee JH, Lee HY, Lee SY, Kim HS, Chae IH, et al. Risk factors of angiotensin-converting enzyme inhibitor-induced cough in patients with hypertension. Korean Circ J. 2000; 30(12):1540–1545.12. Os I, Franco V, Kjeldsen SE, Manhem K, Devereux RB, Gerdts E, et al. Effects of losartan in women with hypertension and left ventricular hypertrophy: results from the Losartan Intervention for Endpoint Reduction in Hypertension Study. Hypertension. 2008; 51(4):1103–1108. PMID: 18259029.13. SPRINT Research Group. Wright JT Jr, Williamson JD, Whelton PK, Snyder JK, Sink KM, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373(22):2103–2116. PMID: 26551272.14. Hermida RC, Crespo JJ, Domínguez-Sardiña M, Otero A, Moyá A, Ríos MT, et al. Bedtime hypertension treatment improves cardiovascular risk reduction: the Hygia Chronotherapy Trial. Eur Heart J. 2020; 41(48):4565–4576. PMID: 31641769.15. SCORE2 Working Group and ESC Cardiovascular Risk Collaboration. SCORE2 risk prediction algorithms: new models to estimate 10-year risk of cardiovascular disease in Europe. Eur Heart J. 2021; 42(25):2439–2454. PMID: 34120177.16. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension: the task force for the management of arterial hypertension of the European Society of Cardiology and the European Society of Hypertension. J Hypertens. 2018; 36(10):1953–2041. PMID: 30234752.17. Bozkurt B, Coats AJ, Tsutsui H, Abdelhamid CM, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure: Endorsed by the Canadian Heart Failure Society, Heart Failure Association of India, Cardiac Society of Australia and New Zealand, and Chinese Heart Failure Association. Eur J Heart Fail. 2021; 23(3):352–380. PMID: 33605000.18. Brambilla G, Bombelli M, Seravalle G, Cifkova R, Laurent S, Narkiewicz K, et al. Prevalence and clinical characteristics of patients with true resistant hypertension in central and Eastern Europe: data from the BP-CARE study. J Hypertens. 2013; 31(10):2018–2024. PMID: 23838657.19. Kumbhani DJ, Steg PG, Cannon CP, Eagle KA, Smith SC Jr, Crowley K, et al. Resistant hypertension: a frequent and ominous finding among hypertensive patients with atherothrombosis. Eur Heart J. 2013; 34(16):1204–1214. PMID: 23144048.20. Redfern A, Peters SA, Luo R, Cheng Y, Li C, Wang J, et al. Sex differences in the awareness, treatment, and control of hypertension in China: a systematic review with meta-analyses. Hypertens Res. 2019; 42(2):273–283. PMID: 30518984.21. Smith SM, Gurka MJ, Calhoun DA, Gong Y, Pepine CJ, Cooper-DeHoff RM. Optimal systolic blood pressure target in resistant and non-resistant hypertension: a pooled analysis of patient-level data from SPRINT and ACCORD. Am J Med. 2018; 131(12):1463–1472.e7. PMID: 30142317.22. Tsujimoto T, Kajio H. Intensive blood pressure treatment for resistant hypertension. Hypertension. 2019; 73(2):415–423. PMID: 30580680.23. Oh JS, Lee CH, Park JI, Park HK, Hwang JK. Hypertension-mediated organ damage and long-term cardiovascular outcomes in Asian hypertensive patients without prior cardiovascular disease. J Korean Med Sci. 2020; 35(48):e400. PMID: 33316856.24. Muiesan ML, Salvetti M, Rizzoni D, Paini A, Agabiti-Rosei C, Aggiusti C, et al. Resistant hypertension and target organ damage. Hypertens Res. 2013; 36(6):485–491. PMID: 23595044.25. Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic impact of baseline and serial changes in electrocardiographic left ventricular hypertrophy in resistant hypertension. Am Heart J. 2010; 159(5):833–840. PMID: 20435193.26. Cuspidi C, Sala C, Negri F, Mancia G, Morganti A. Italian Society of Hypertension. Prevalence of left-ventricular hypertrophy in hypertension: an updated review of echocardiographic studies. J Hum Hypertens. 2012; 26(6):343–349. PMID: 22113443.27. Papazafiropoulou A, Skliros E, Sotiropoulos A, Papafragos C, Gikas A, Apostolou O, et al. Prevalence of target organ damage in hypertensive subjects attending primary care: C.V.P.C. study (epidemiological cardio-vascular study in primary care). BMC Fam Pract. 2011; 12(1):75. PMID: 21756310.28. da Costa PM, Cortez AF, de Souza F, Mares GS, Dos Santos BD, Muxfeldt ES. Prognostic impact of baseline urinary albumin excretion rate in patients with resistant hypertension: a prospective cohort study. J Hum Hypertens. 2018; 32(2):139–149. PMID: 29230004.29. Salles GF, Cardoso CR, Fiszman R, Muxfeldt ES. Prognostic importance of baseline and serial changes in microalbuminuria in patients with resistant hypertension. Atherosclerosis. 2011; 216(1):199–204. PMID: 21315356.30. Salles GF, Cardoso CR, Pereira VS, Fiszman R, Muxfeldt ES. Prognostic significance of a reduced glomerular filtration rate and interaction with microalbuminuria in resistant hypertension: a cohort study. J Hypertens. 2011; 29(10):2014–2023. PMID: 21873887.31. Daugherty SL, Powers JD, Magid DJ, Tavel HM, Masoudi FA, Margolis KL, et al. Incidence and prognosis of resistant hypertension in hypertensive patients. Circulation. 2012; 125(13):1635–1642. PMID: 22379110.32. Muntner P, Davis BR, Cushman WC, Bangalore S, Calhoun DA, Pressel SL, et al. Treatment-resistant hypertension and the incidence of cardiovascular disease and end-stage renal disease: results from the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). Hypertension. 2014; 64(5):1012–1021. PMID: 25259745.33. Quan H, Chen G, Walker RL, Wielgosz A, Dai S, Tu K, et al. Incidence, cardiovascular complications and mortality of hypertension by sex and ethnicity. Heart. 2013; 99(10):715–721. PMID: 23403406.34. Leung AA, Williams JV, Tran KC, Padwal RS. Epidemiology of resistant hypertension in Canada. Can J Cardiol. 2022; 38(5):681–687. PMID: 35122938.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nighttime administration of antihypertensive medication: a review of chronotherapy in hypertension
- A Clinical Observation on Antihypertensive Effect of Tripamide(Normonal(R))
- Importance of Clinical Evaluations Related to Secondary Hypertension in Patients with Resistant Hypertension
- Cardiovascular Response to Insertion of Laryngeal Mask in Hypertensive Patients
- Clinical Observation on Antihypertensive Effect of Acebutolol Hydrochloride(Sectral(R))