J Korean Med Sci.
2023 Apr;38(15):e119. 10.3346/jkms.2023.38.e119.
Participation and Prognostic Impact of Cardiac Rehabilitation After Acute Coronary Syndrome: Big-Data Study of the Korean National Health Insurance Service
- Affiliations
-
- 1Department of Rehabilitation Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 2Department of Rehabilitation Medicine, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea
- 3Data Science Team, Hanmi Pharm. Co., Ltd., Seoul, Korea
- KMID: 2541557
- DOI: http://doi.org/10.3346/jkms.2023.38.e119
Abstract
- Background
To investigate the actual rate and quality of cardiac rehabilitation (CR) participation in South Korea and its short-term impact on clinical outcomes after acute coronary syndrome (ACS).
Methods
Data, including confirmed ACS diagnosis, socio-demographics, comorbidities, clinical outcomes, and CR claim codes, were collected from the Korean National Health Insurance Service claims database and compared between the CR and non-CR groups.
Results
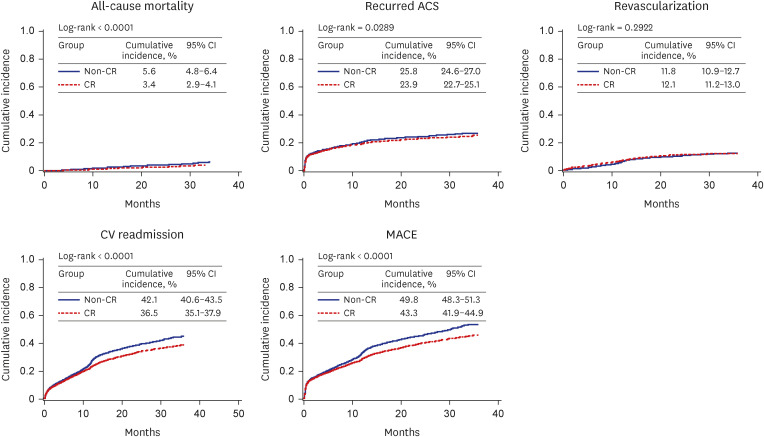
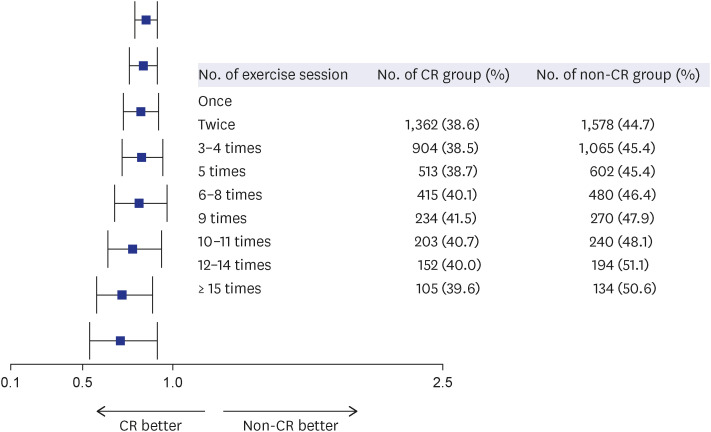
Overall, 102,544 patients were included in the study, of which only 5.8% attended CR. Regarding testing, 83.6% of CR patients performed the cardiopulmonary exercise test, but follow-up testing was infrequently performed; in addition, 53.1% of them participated in an electrocardiogram monitoring exercise, but over half participated in only one session. After 1:1 propensity score matching, post-ACS cardiovascular events were significantly lower in the CR group than in the non-CR group. The cumulative 3-year hazard ratio for all-cause death was 0.612 (95% confidence interval [CI], 0.495–0.756), recurrent ACS was 0.92 (95% CI, 0.853–0.993), CR readmission was 0.817 (95% CI, 0.768–0.868), and major adverse cardiovascular events (MACE) was 0.827 (95% CI, 0.781–0.874) in the CR group. CR was associated with a significant dose-response effect on MACE, with a reduction in incidence from 0.854 to 0.711.
Conclusion
The actual rate of CR participation in South Korea remains low, and participation quality was not outstanding despite National Health Insurance coverage. Nevertheless, the impact of CR on cardiovascular outcomes after ACS was significantly superior. Efforts to increase CR participation should be increased by establishing new CR facilities and strategies to resolve associated barriers.
Figure
Reference
-
1. World Health Organization. WHO reveals leading causes of death and disability worldwide; 2000–2019. Updated 2020. Accessed January 7, 2022. https://www.who.int/news/item/09-12-2020-who-reveals-leading-causes-of-death-and-disability-worldwide-2000-2019 .2. Lee SW, Kim HC, Lee HS, Suh I. Thirty-year trends in mortality from cardiovascular diseases in Korea. Korean Circ J. 2015; 45(3):202–209. PMID: 26023308.3. Korean Statistical Information Service. Cause of death statistics. Updated 2020. Accessed September 9, 2021. https://kostat.go.kr/board.es?mid=a10301060200&bid=218 .4. Lee HH, Cho SM, Lee H, Baek J, Bae JH, Chung WJ, et al. Korea heart disease fact sheet 2020: analysis of nationwide data. Korean Circ J. 2021; 51(6):495–503. PMID: 34085422.5. Lewanczuk R, Suskin N, Arthur HM. Principles of chronic disease care. Stone JA, Arthur HM, Suskin NG, Austford L, Carlson J, Cupper L, editors. Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention: Translating Knowledge Into Action. 3rd ed. Winnipeg, Canada: Canadian Association of Cardiac Rehabilitation;2009. p. 63–68.6. Ades PA, Keteyian SJ, Wright JS, Hamm LF, Lui K, Newlin K, et al. Increasing cardiac rehabilitation participation from 20% to 70%: a road map from the Million Hearts Cardiac Rehabilitation Collaborative. Mayo Clin Proc. 2017; 92(2):234–242. PMID: 27855953.7. Kim SH, Ro JS, Kim Y, Leigh JH, Kim WS. Underutilization of hospital-based cardiac rehabilitation after acute myocardial infarction in Korea. J Korean Med Sci. 2020; 35(30):e262. PMID: 32743992.8. Kim C, Sung J, Han JY, Jee S, Lee JW, Lee JH, et al. Current status of cardiac rehabilitation in the Regional Cardiocerebrovascular Centers in Korea. J Clin Med. 2021; 10(21):5079. PMID: 34768598.9. National Health Insurance Service. Population coverage of National Health Insurance Service. Updated 2020. Accessed April 30, 2022. https://www.nhis.or.kr/nhis/policy/wbhada01700m01.do .10. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the Korean National Health Insurance system. Diabetes Metab J. 2014; 38(5):395–403. PMID: 25349827.11. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the national health information database of the National Health Insurance Service in South Korea. Int J Epidemiol. 2017; 46(3):799–800. PMID: 27794523.12. Kwon CH, Kim W, Shin JH, Lee CJ, Kim HC, Kang SH, et al. Office blood pressure range and cardiovascular events in patients with hypertension: a nationwide cohort study in South Korea. J Am Heart Assoc. 2021; 10(7):e017890. PMID: 33739126.13. Kim C, Choi IS, Cho SH, Park EJ, Shim JI, Choi JA, et al. Impact of Cardiac Rehabilitation on Event-Free Survival Rates in Acute Myocardial Infarction. Seoul, Korea: National Evidence-based Healthcare Collaborating Agency (NECA);2018.14. Scottish Intercollegiate Guidelines Network (SIGN). Cardiac rehabilitation: a national clinical guideline. Updated 2017. Accessed July 2017. http://www.sign.ac.uk .15. National Institute for Health and Care Excellence (NICE). Surveillance report 2017: myocardial infarction: cardiac rehabilitation and prevention of further cardiovascular disease. NICE guideline CG172. Updated 2013. Accessed November 2013. https://www.nice.org.uk/guidance/cg172 .16. Smith SC Jr, Benjamin EJ, Bonow RO, Braun LT, Creager MA, Franklin BA, et al. AHA/ACCF secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation. 2011; 124(22):2458–2473. PMID: 22052934.17. Stone JA, Arthur HM, Suskin NG, Austford L, Carlson J, Cupper L, et al. Canadian Guidelines for Cardiac Rehabilitation and Cardiovascular Disease Prevention: Translating Knowledge Into Action. Winnipeg, Canada: Canadian Association of Cardiac Rehabilitation;2009.18. JCS Joint Working Group. Guidelines for rehabilitation in patients with cardiovascular disease (JCS 2012). Circ J. 2014; 78(8):2022–2093. PMID: 25047729.19. Kim C, Sung J, Lee JH, Kim WS, Lee GJ, Jee S, et al. Clinical practice guideline for cardiac rehabilitation in Korea: recommendations for cardiac rehabilitation and secondary prevention after acute coronary syndrome. Korean Circ J. 2019; 49(11):1066–1111. PMID: 31646772.20. Goto Y. Current state of cardiac rehabilitation in Japan. Prog Cardiovasc Dis. 2014; 56(5):557–562. PMID: 24607022.21. Humphrey R, Guazzi M, Niebauer J. Cardiac rehabilitation in Europe. Prog Cardiovasc Dis. 2014; 56(5):551–556. PMID: 24607021.22. Beatty AL, Truong M, Schopfer DW, Shen H, Bachmann JM, Whooley MA. Geographic variation in cardiac rehabilitation participation in Medicare and Veterans Affairs populations: opportunity for improvement. Circulation. 2018; 137(18):1899–1908. PMID: 29305529.23. Turk-Adawi K, Supervia M, Lopez-Jimenez F, Pesah E, Ding R, Britto RR, et al. Cardiac rehabilitation availability and density around the globe. EClinicalMedicine. 2019; 13:31–45. PMID: 31517261.24. Grace SL, Shanmugasegaram S, Gravely-Witte S, Brual J, Suskin N, Stewart DE. Barriers to cardiac rehabilitation: does age make a difference? J Cardiopulm Rehabil Prev. 2009; 29(3):183–187. PMID: 19471138.25. Thomas RJ, Beatty AL, Beckie TM, Brewer LC, Brown TM, Forman DE, et al. Home-based cardiac rehabilitation: a scientific statement from the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. J Cardiopulm Rehabil Prev. 2019; 39(4):208–225. PMID: 31082934.26. Hammill BG, Curtis LH, Schulman KA, Whellan DJ. Relationship between cardiac rehabilitation and long-term risks of death and myocardial infarction among elderly Medicare beneficiaries. Circulation. 2010; 121(1):63–70. PMID: 20026778.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pediatric Cancer Research using Healthcare Big Data
- Introducing big data analysis using data from National Health Insurance Service
- Barriers to Outpatient Hospital-Based Cardiac Rehabilitation in Korean Patients With Acute Coronary Syndrome
- Underutilization of Hospital-based Cardiac Rehabilitation after Acute Myocardial Infarction in Korea
- The Reasons That Cardiac Patients Did Not Participate in and Drop out from the Cardiac Rehabilitation Program