Pediatr Emerg Med J.
2023 Apr;10(2):68-71. 10.22470/pemj.2023.00668.
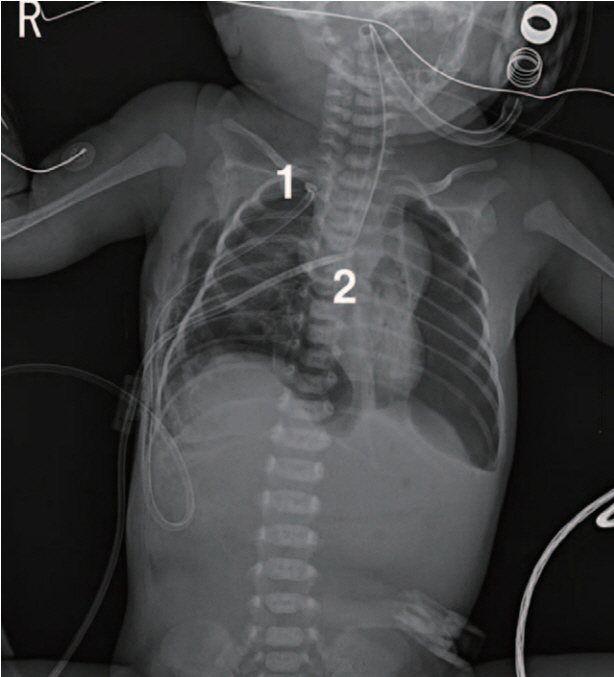
Bilateral tension pneumothoraces in a preterm low-birthweight newborn: tube thoracostomy using four 7-French latex catheters performed by an emergency physician
- Affiliations
-
- 1Department of Pediatrics, Daegu Fatima Hospital, Daegu, Republic of Korea
- 2Department of Emergency Medicine, CHA Gumi Medical Center, CHA University School of Medicine, Gumi-si, Republic of Korea
- 3Department of Thoracic Surgery, School of Medicine, Kyungpook National University, Daegu, Republic of Korea
- 4Current affiliation: Department of Emergency Medicine, Daegu Fatima Hospital, Daegu, Republic of Korea
- KMID: 2540911
- DOI: http://doi.org/10.22470/pemj.2023.00668
Abstract
- Neonatal tension pneumothorax is life-threatening. A tension pneumothorax on the right side was detected on a newborn boy weighing 2,380 g, who was born at 35 weeks of gestation. Given the unavailability of an on-duty thoracic surgeon and appropriately sized chest tubes in the neonatal intensive care unit, an emergency physician performed closed thoracostomy using two 7-French latex catheters. Immediately after the re-expansion of the right lung, left tension pneumothorax was newly detected. Two more 7-French latex catheters were inserted, relieving the left lesion. We consider that the right pneumothorax occurred due to the mixture of spontaneous rupture of the subpleural blebs and barotrauma during the initial positive pressure ventilation, while the left lesion did due to the high-flow oscillatory ventilation. Despite the limited availability of devices in the present case, a favorable outcome was achieved by the use of alternative catheters, which were chosen by the emergency physician.
Keyword
Figure
Reference
-
References
1. Kim SK, Kim WH. Tension pneumothorax in a newborn after Cesarean-section delivery: a case report. Korean J Anesthesiol. 2010; 59:420–4.2. Vibede L, Vibede E, Bendtsen M, Pedersen L, Ebbesen F. Neonatal pneumothorax: a descriptive regional Danish study. Neonatology. 2017; 111:303–8.3. Smith J, Schumacher RE, Donn SM, Sarkar S. Clinical course of symptomatic spontaneous pneumothorax in term and late preterm newborns: report from a large cohort. Am J Perinatol. 2011; 28:163–8.4. Kim EA, Jung JH, Lee SY, Park SH, Kim JS. Neonatal pneumothorax in late preterm and full-term newborns with respiratory distress: a single-center experience. Neonatal Med. 2022; 29:18–27.5. Panza R, Prontera G, Ives KN, Zivanovic S, Roehr CC, Quercia M, et al. Pigtail catheters versus traditional chest drains for pneumothorax treatment in two NICUs. Eur J Pediatr. 2020; 179:73–9.6. Arda IS, Gürakan B, Alíefendío˘glu D, Tüzün M. Treatment of pneumothorax in newborns: use of venous catheter versus chest tube. Pediatr Int. 2002; 44:78–82.7. Bruschettini M, Romantsik O, Ramenghi LA, Zappettini S, O’Donnell CP, Calevo MG. Needle aspiration versus intercostal tube drainage for pneumothorax in the newborn. Cochrane Database Syst Rev. 2016; CD011724.8. Liu J, Cao HY, Sorantin E. Pneumothorax of the newborn. In: Liu J, Cao HY, Sorantin E, editors. Neonatal lung ultrasonography. Dordrecht: Springer Nature; 2018. p. 111-22.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Long-term Follow-up Study of Therapeutic Effects of 8 French Catheter for Spontaneous Pneumothorax
- Neonatal outcomes of very low birthweight infants from spontaneous and indicated preterm delivery
- Spontaneous Resolution of Pulmonary Artery Pseudoaneurysm after Tube Thoracostomy
- Complications of a Tube Thoracostomy Performed by Emergency Medicine Residents
- Tension pneumothorax in a newborn after Cesarean-section delivery: A case report