Kosin Med J.
2023 Mar;38(1):43-49. 10.7180/kmj.22.133.
Comparison of the prevalence and histology between primary benign bladder tumors and recurrent benign lesions after transurethral resection of malignant bladder tumors
- Affiliations
-
- 1Department of Urology, Kosin University Gospel Hospital, Busan, Korea
- 2Department of Pathology, Kosin University Gospel Hospital, Busan, Korea
- KMID: 2540761
- DOI: http://doi.org/10.7180/kmj.22.133
Abstract
- Background
Benign bladder tumors are rare disease entities, and insufficient studies have assessed their epidemiological characteristics. The authors investigated the prevalence of benign bladder tumors by retrospectively investigating pathology reports of transurethral resection of bladder tumor (TURBT) procedures over the past 20 years.
Methods
We analyzed 1,674 pathology reports of TURBT conducted in 1,160 patients from January 1, 2000, to April 30, 2022. The prevalence of benign tumors and histological classification according to the presence of primary (group 1) and recurrent (group 2) bladder lesions were retrospectively investigated.
Results
The mean age of patients was 65.2±11.5 years, and 1,284 cases (79.1%) were in men. Benign bladder tumors comprised 278 cases (248 patients) accounting for about 17.1% of the total TURBT cases (278/1,624). Furthermore, 184 patients (16.0%, 184/1,147) belonged to group 1 and 78 patients (27.4%, 78/285) belonged to group 2. Among all benign lesions that underwent TURBT, cystitis was the most common (41.0%, 114/278), and this rate was higher in group 2 (64/184 [34.8%] vs. 50/94 [53.2%], p<0.001). The prevalence of non-neoplastic lesions was higher in group 1 (44/184 [23.9] vs. 11/94 [11.7%], p<0.001). There was no difference in the prevalence of noninvasive urothelial neoplasms between the two groups (22/184 [12.0%] vs. 8/94 [8.5%], p=0.86).
Conclusions
The probability of benign lesions in TURBT was 17.1%, among which cystitis was the most common. When TURBT was performed for recurrent lesions, the frequency of benign tumors was higher than that of primary benign bladder tumors.
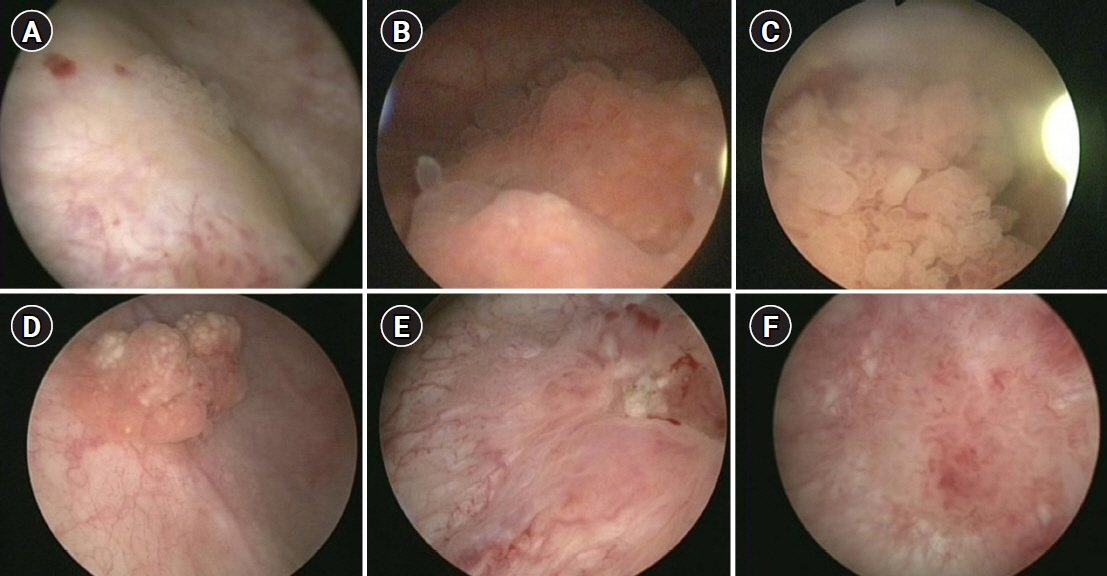
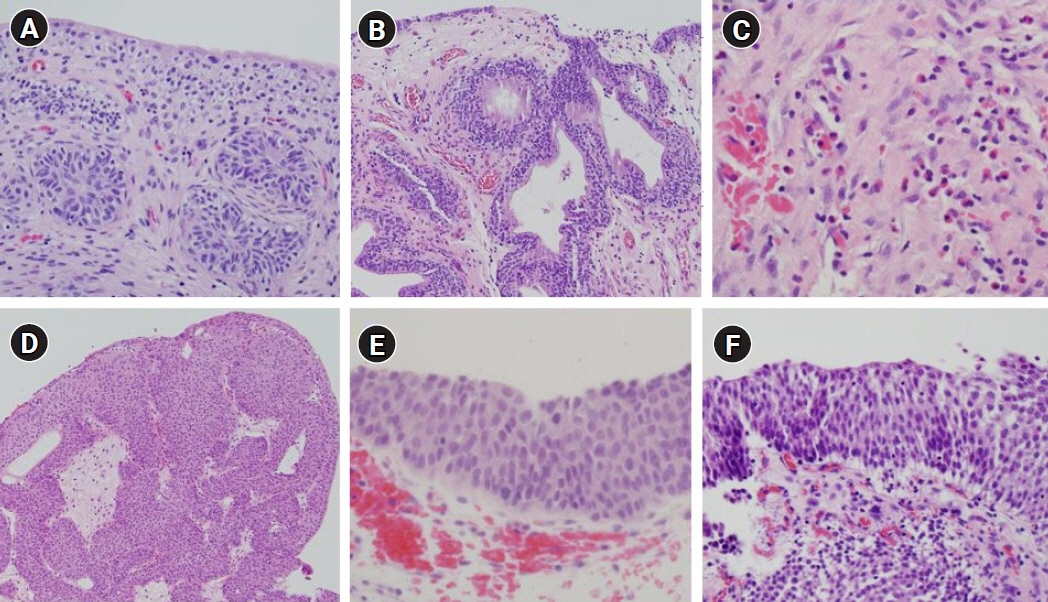
Figure
Reference
-
References
1. Mendes JE, Ferreira AV, Coelho SA, Gil C. Bladder leiomyoma. Urol Ann. 2017; 9:275–7.2. Monappa V, Jaiprakash P, Thomas J, Hegde P. Bladder paraganglioma: a report of two cases. Afr J Urol. 2018; 24:70–2.3. Picozzi S, Casellato S, Bozzini G, Ratti D, Macchi A, Rubino B, et al. Inverted papilloma of the bladder: a review and an analysis of the recent literature of 365 patients. Urol Oncol. 2013; 31:1584–90.4. Sweeney MK, Rais-Bahrami S, Gordetsky J. Inverted urothelial papilloma: a review of diagnostic pitfalls and clinical management. Can Urol Assoc J. 2017; 11:66–9.5. Paciotti M, Contieri R, Fasulo V, Casale P, Saita A, Buffi NM, et al. Active surveillance for recurrent non-muscle invasive bladder cancer: which lessons have we learned during COVID-19 pandemic? Minerva Urol Nephrol. 2022; 74:1–4.6. Hurle R, Colombo P, Lazzeri M, Lughezzani G, Buffi NM, Saita A, et al. Pathological outcomes for patients who failed to remain under active surveillance for low-risk non-muscle-invasive bladder cancer: update and results from the Bladder Cancer Italian Active Surveillance Project. Eur Urol Oncol. 2018; 1:437–42.7. Ribeiro A, Pereira M, Reis A, Ferreira G. Urothelial papilloma: a rare cause of gross haematuria in childhood. BMJ Case Rep. 2017; 2017:bcr2017219341.8. Humphrey PA, Moch H, Cubilla AL, Ulbright TM, Reuter VE. The 2016 WHO classification of tumours of the urinary system and male genital organs: Part B: prostate and bladder tumours. Eur Urol. 2016; 70:106–19.9. Lane Z, Epstein JI. Polypoid/papillary cystitis: a series of 41 cases misdiagnosed as papillary urothelial neoplasia. Am J Surg Pathol. 2008; 32:758–64.10. Hodges KB, Lopez-Beltran A, Davidson DD, Montironi R, Cheng L. Urothelial dysplasia and other flat lesions of the urinary bladder: clinicopathologic and molecular features. Hum Pathol. 2010; 41:155–62.11. Abdel Gawad AM, Rabie A, Abdelwahed MS, Hasan A. Urothelial papilloma of the urinary bladder: a case report and literature review of a rare entity. Cureus. 2022; 14:e22046.12. Bobjer J, Hagberg O, Aljabery F, Gardmark T, Jahnson S, Jerlstrom T, et al. Bladder cancer recurrence in papillary urothelial neoplasm of low malignant potential (PUNLMP) compared to G1 WHO 1999: a population-based study. Scand J Urol. 2022; 56:14–8.13. Maxwell JP, Wang C, Wiebe N, Yilmaz A, Trpkov K. Long-term outcome of primary papillary urothelial neoplasm of low malignant potential (PUNLMP) including PUNLMP with inverted growth. Diagn Pathol. 2015; 10:3.14. Jones TD, Cheng L. Reappraisal of the papillary urothelial neoplasm of low malignant potential (PUNLMP). Histopathology. 2020; 77:525–35.15. Jones TD, Cheng L. Noninvasive papillary urothelial neoplasia (NIPUN): renaming cancer. Urol Oncol. 2021; 39:286–90.16. Hernandez V, Llorente C, de la Pena E, Perez-Fernandez E, Guijarro A, Sola I. Long-term oncological outcomes of an active surveillance program in recurrent low grade Ta bladder cancer. Urol Oncol. 2016; 34:165.e19-23.17. Soloway MS. Active surveillance or office fulguration for low grade ta bladder tumors: a win-win for patients and urologists. J Urol. 2018; 199:1120–2.18. Seo WT, Kang SH. Postoperative recurrent bladder tumors detection by narrow-band imaging cystoscopy. Korean J Urol Oncol. 2020; 18:209–14.19. Contieri R, Paciotti M, Lughezzani G, Buffi NM, Frego N, Diana P, et al. Long-term follow-up and factors associated with active surveillance failure for patients with non-muscle-invasive bladder cancer: the Bladder Cancer Italian Active Surveillance (BIAS) experience. Eur Urol Oncol. 2022; 5:251–5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intraoperative ventilation and hemodynamic change due to bladder perforation during transurethral resection of a bladder tumor: A case report
- A Case of Inflammatory Pseudotumor of the Bladder
- Sudden hypothermia after bladder perforation during transurethral bladder tumor resection: A case report
- Non-transitional Cell Bladder Tumors
- Clinical Results of Transurethral Resection for the Benign Prostatic Hypertrophy -Significance of Suprapubic Cystostomy before Transurethral Resection-