J Korean Foot Ankle Soc.
2023 Mar;27(1):24-29. 10.14193/jkfas.2023.27.1.24.
Two-Stage Operation Over a Period of 7 Years for a Patient with Macrodactyly: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Inje University Busan Paik Hospital, Busan, Korea
- 2Department of Pediatrics, Inha University Hospital, Incheon, Korea
- KMID: 2540403
- DOI: http://doi.org/10.14193/jkfas.2023.27.1.24
Abstract
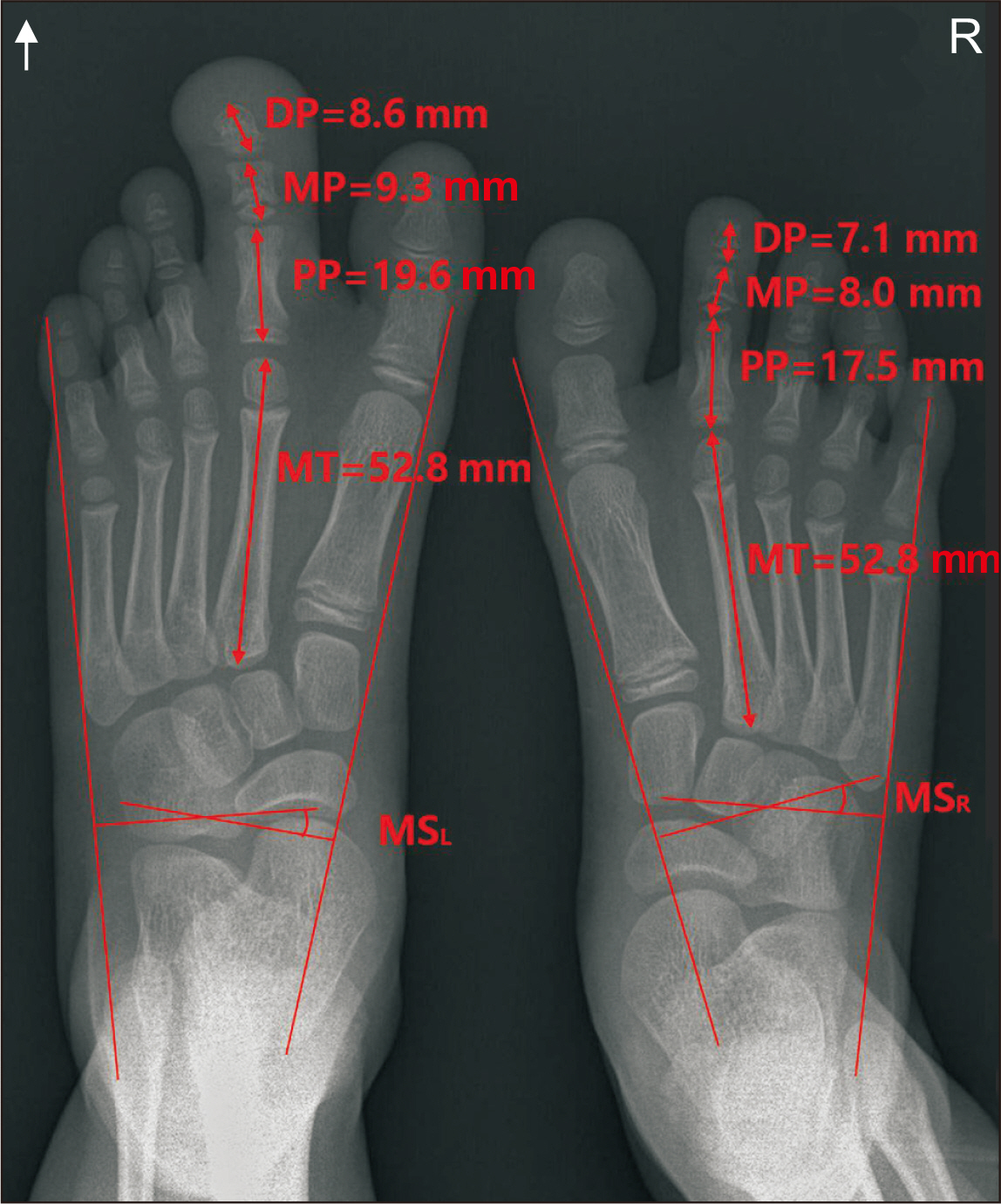
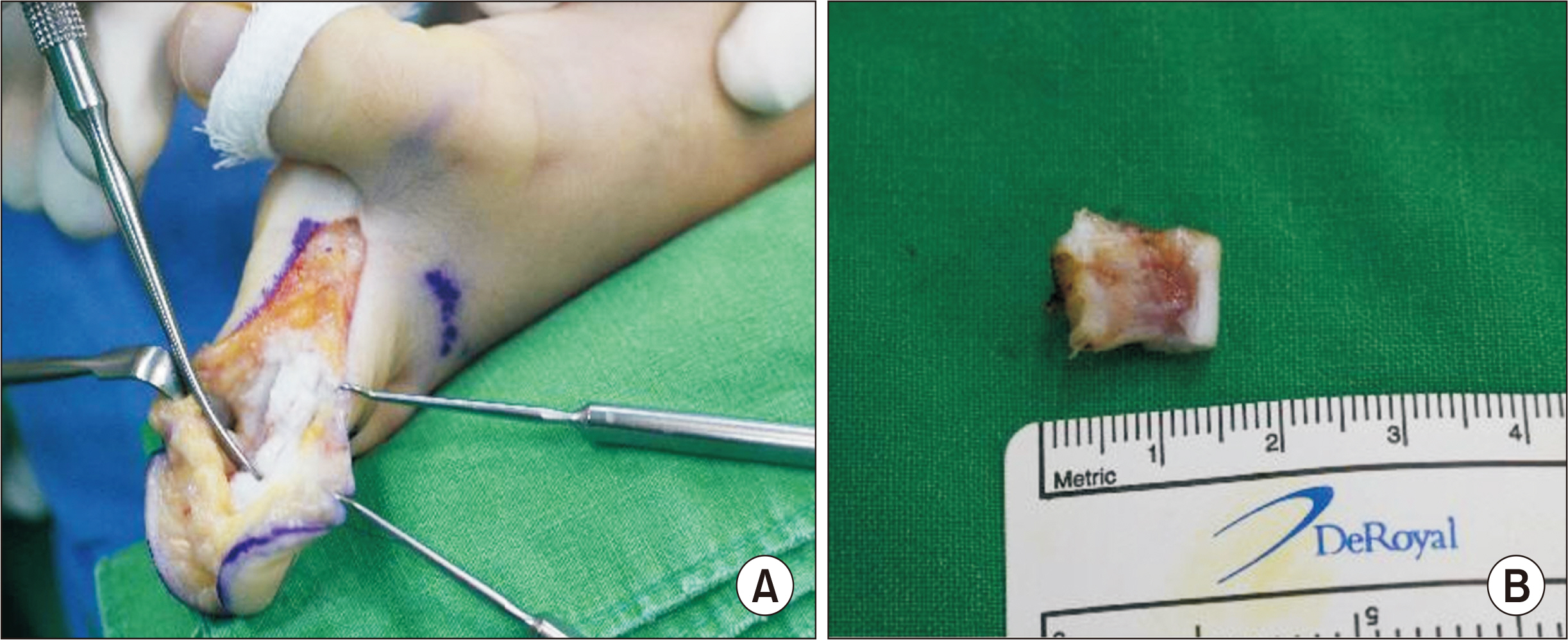
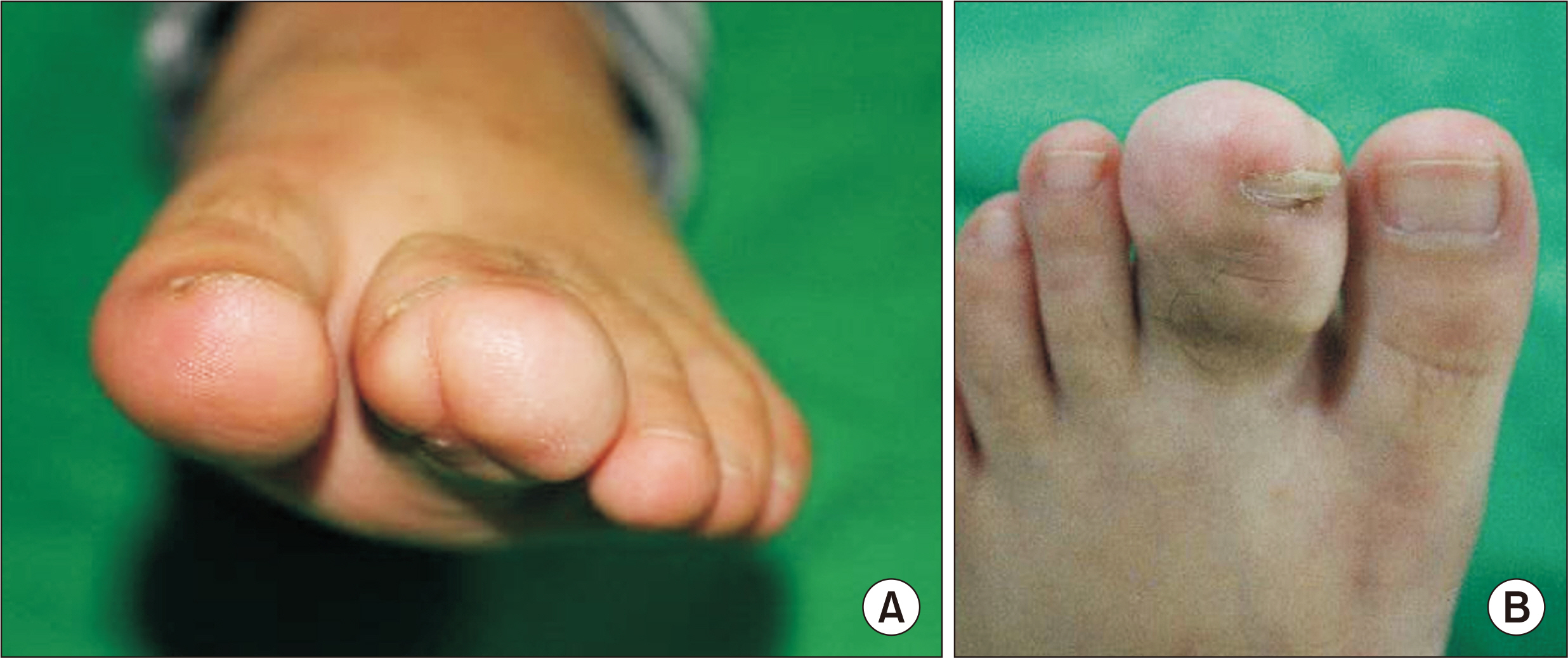
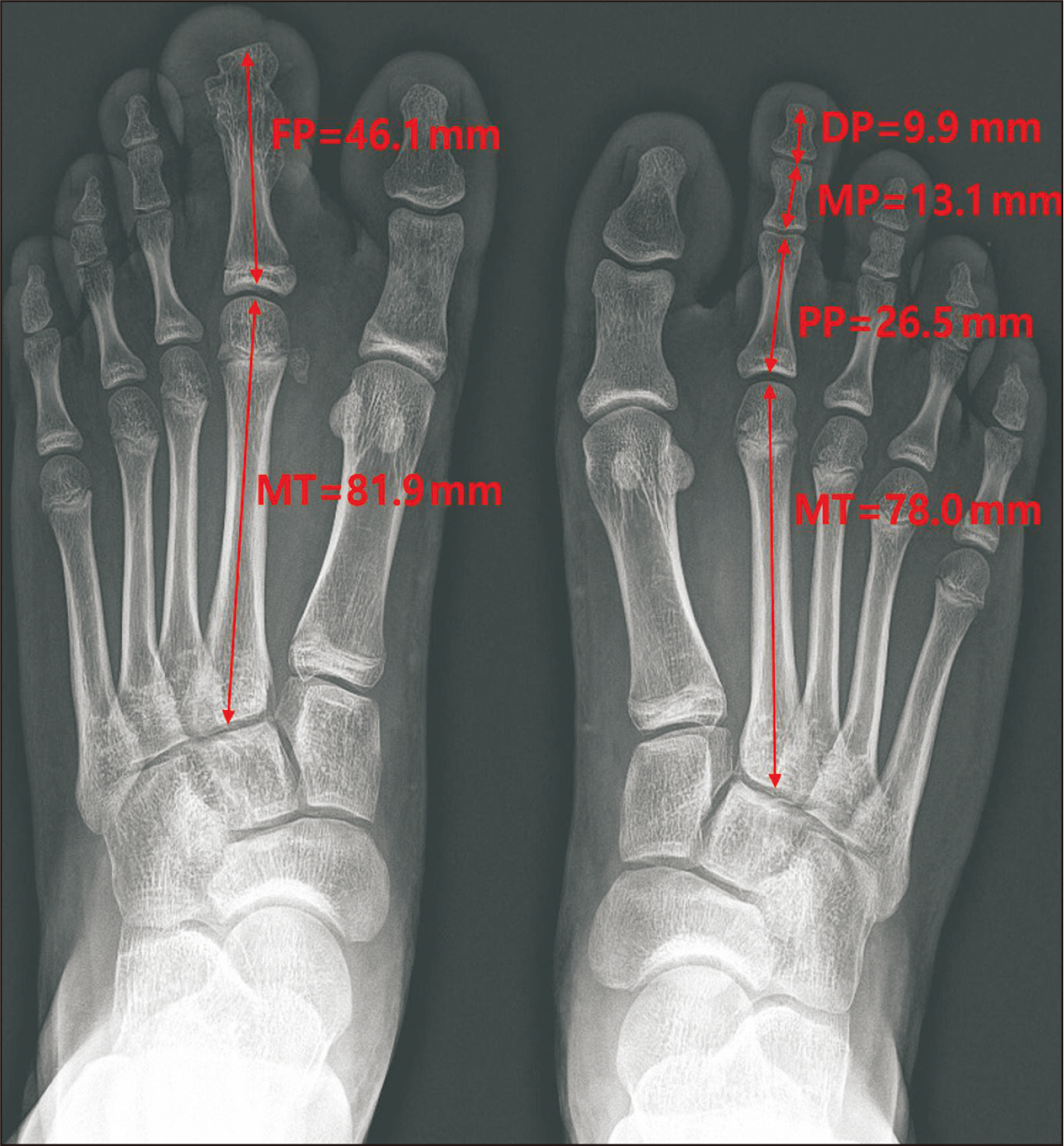
- Macrodactyly of the toe is a rare congenital anomaly characterized by the overgrowth of a digit/digits in the foot and is one of the most difficult conditions to treat. Since the condition alters functionality and appearance, the treatment goal is to restore function and cosmetically enhance the appearance. Various surgical techniques are used for toe macrodactyly, including amputation, debulking, and epiphysiodesis. Herein, we present a case of a six-year-old patient with a second toe macrodactyly who was successfully treated with a twostage operation over a seven-year period. We initially performed an ostectomy of the middle phalanx with a fusion of the proximal and distal phalanges and then performed a soft tissue debulking procedure.
Keyword
Figure
Reference
-
1. Barsky AJ. 1967; Macrodactyly. J Bone Joint Surg Am. 49:1255–66. DOI: 10.2106/00004623-196749070-00001. PMID: 4293291.
Article2. Kotwal PP, Farooque M. 1998; Macrodactyly. J Bone Joint Surg Br. 80:651–3. doi: 10.1302/0301-620x.80b4.8489. DOI: 10.1302/0301-620X.80B4.8489. PMID: 9699830.
Article3. Flatt AE. 1994. The care of congenital hand anomalies. 2nd ed. Quality Medical;St. Louis:4. Hardwicke J, Khan MA, Richards H, Warner RM, Lester R. 2013; Macrodactyly - options and outcomes. J Hand Surg Eur Vol. 38:297–303. doi: 10.1177/1753193412451232. DOI: 10.1177/1753193412451232. PMID: 22736742.
Article5. Lee SJ, Lee HJ, Kim PT. 2016; Single stage reduction operation for treatment of toe macrodactyly in skeletally immature patients. J Korean Orthop Assoc. 51:260–5. doi: 10.4055/jkoa.2016.51.3.260. DOI: 10.4055/jkoa.2016.51.3.260.
Article6. Topoleski TA, Ganel A, Grogan DP. 1997; Effect of proximal phalangeal epiphysiodesis in the treatment of macrodactyly. Foot Ankle Int. 18:500–3. doi: 10.1177/107110079701800807. DOI: 10.1177/107110079701800807. PMID: 9278744.
Article7. Tsuge K. 1967; Treatment of macrodactyly. Plast Reconstr Surg. 39:590–9. doi: 10.1097/00006534-196706000-00008. DOI: 10.1097/00006534-196706000-00008. PMID: 6025687.
Article8. Chang CH, Kumar SJ, Riddle EC, Glutting J. 2002; Macrodactyly of the foot. J Bone Joint Surg Am. 84:1189–94. doi: 10.2106/00004623-200207000-00015. DOI: 10.2106/00004623-200207000-00015. PMID: 12107320.
Article9. Kim J, Park JW, Hong SW, Jeong JY, Gong HS, Baek GH. Ray amputation for the treatment of foot macrodactyly in children. Bone Joint J. 2015; 97-B:1364–9. doi: 10.1302/0301-620X.97B10.35660. DOI: 10.1302/0301-620X.97B10.35660. PMID: 26430011.
Article10. Kelly DM. Canale ST, Beaty JH, editors. 2013. Congenital anomalies of the lower extremity. Campbell’s operative orthopaedics. 12th ed. Philadelphia: Elsevier Mosby;p. 980–1078.
Article