J Korean Med Sci.
2023 Mar;38(9):e68. 10.3346/jkms.2023.38.e68.
Association Between Air Pollution and Viral Infection in Severe Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- Affiliations
-
- 1Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 2Division of Pulmonary, Allergy, and Critical Care Medicine, Department of Internal Medicine, Hallym University Chuncheon Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- 3Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 6Division of Pulmonary and Critical Care Medicine, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 7Department of Internal Medicine and Environmental Health Center, Kangwon National University College of Medicine, Chuncheon, Korea
- 8Division of Respiratory Medicine, Department of Internal Medicine, Dong-A University College of Medicine, Dong-A University Medical Center, Busan, Korea
- 9Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2540126
- DOI: http://doi.org/10.3346/jkms.2023.38.e68
Abstract
- Background
Respiratory pathogen infections and air pollution are main causes of acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Air pollution has a direct effect on the airway epithelial barrier and the immune system, which can have an influence on infection. However, studies on the relationship between respiratory infections and air pollutants in severe AECOPD are limited. Thus, the objective of this study was to investigate the correlation between air pollution and respiratory pathogen in severe AECOPD.
Methods
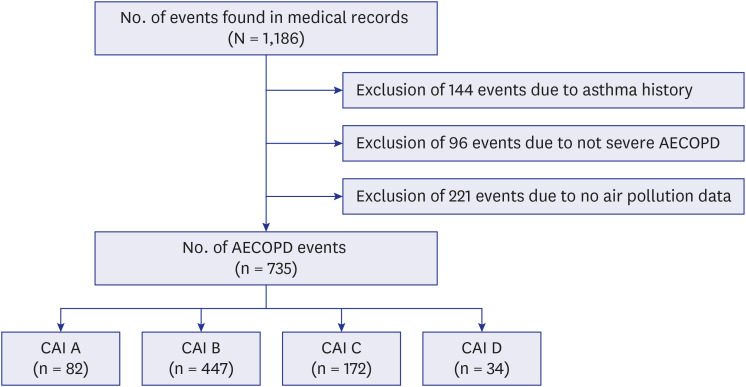
This multicenter observational study was conducted by reviewing electronic medical records of patients with AECOPD at 28 hospitals in South Korea. Patients were divided into four groups according to the comprehensive air-quality index (CAI) used in Korea. Identification rates of bacteria and viruses of each group were analyzed.
Results
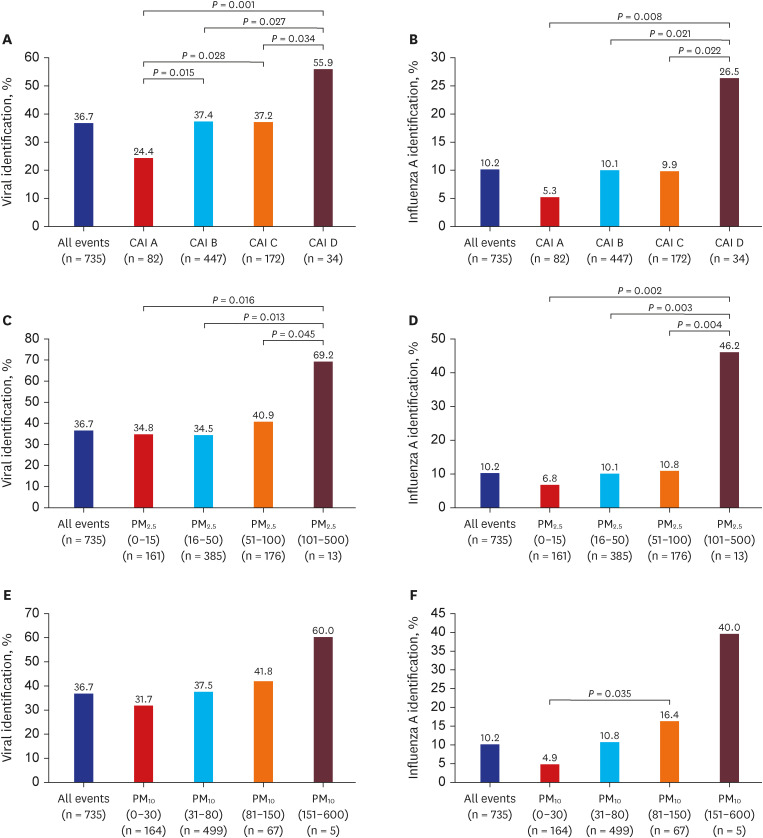
Viral pathogens were identified in 270 (36.7%) of 735 patients. Viral identification rate was different (P = 0.012) according to air pollution. Specifically, the virus detection rate was 55.9% in the group of CAI ‘D’ with the highest air pollution. It was 24.4% in the group of CAI ‘A’ with the lowest air pollution. This pattern was clearly seen for influenza virus A (P = 0.042). When further analysis was performed with particulate matter (PM), the higher/lower the PM level, the higher/lower the virus detection rate. However, no significant difference was found in the analysis related to bacteria.
Conclusion
Air pollution may make COPD patients more susceptible to respiratory viral infections, especially influenza virus A. Thus, on days with poor air quality, COPD patients need to be more careful about respiratory infections.
Keyword
Figure
Reference
-
1. Adeloye D, Song P, Zhu Y, Campbell H, Sheikh A, Rudan I, et al. Global, regional, and national prevalence of, and risk factors for, chronic obstructive pulmonary disease (COPD) in 2019: a systematic review and modelling analysis. Lancet Respir Med. 2022; 10(5):447–458. PMID: 35279265.2. Yawn BP, Thomashow B. Management of patients during and after exacerbations of chronic obstructive pulmonary disease: the role of primary care physicians. Int J Gen Med. 2011; 4:665–676. PMID: 21941453.3. Ritchie AI, Wedzicha JA. Definition, causes, pathogenesis, and consequences of chronic obstructive pulmonary disease exacerbations. Clin Chest Med. 2020; 41(3):421–438. PMID: 32800196.4. Hansel NN, McCormack MC, Kim V. The effects of air pollution and temperature on COPD. COPD. 2016; 13(3):372–379. PMID: 26683097.5. Jung EJ, Na W, Lee KE, Jang JY. Elderly mortality and exposure to fine particulate matter and ozone. J Korean Med Sci. 2019; 34(48):e311. PMID: 31833266.6. Han C, Kim S, Lim YH, Bae HJ, Hong YC. Spatial and temporal trends of number of deaths attributable to ambient PM2.5 in the Korea. J Korean Med Sci. 2018; 33(30):e193. PMID: 30034305.7. Choi J, Oh JY, Lee YS, Min KH, Hur GY, Lee SY, et al. Harmful impact of air pollution on severe acute exacerbation of chronic obstructive pulmonary disease: particulate matter is hazardous. Int J Chron Obstruct Pulmon Dis. 2018; 13:1053–1059. PMID: 29681728.8. Yang L, Li C, Tang X. The impact of PM2.5 on the host defense of respiratory system. Front Cell Dev Biol. 2020; 8:91. PMID: 32195248.9. Loaiza-Ceballos MC, Marin-Palma D, Zapata W, Hernandez JC. Viral respiratory infections and air pollutants. Air Qual Atmos Health. 2022; 15(1):105–114. PMID: 34539932.10. Lee HW, Sim YS, Jung JY, Seo H, Park JW, Min KH, et al. A multicenter study to identify the respiratory pathogens associated with exacerbation of chronic obstructive pulmonary disease in Korea. Tuberc Respir Dis (Seoul). 2022; 85(1):37–46. PMID: 34666427.11. Choi J, Oh JY, Lee YS, Min KH, Hur GY, Lee SY, et al. Harmful impact of air pollution on severe acute exacerbation of chronic obstructive pulmonary disease: particulate matter is hazardous. Int J Chron Obstruct Pulmon Dis. 2018; 13:1053–1059. PMID: 29681728.12. Li J, Sun S, Tang R, Qiu H, Huang Q, Mason TG, et al. Major air pollutants and risk of COPD exacerbations: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2016; 11:3079–3091. PMID: 28003742.13. Song B, Zhang H, Jiao L, Jing Z, Li H, Wu S. Effect of high-level fine particulate matter and its interaction with meteorological factors on AECOPD in Shijiazhuang, China. Sci Rep. 2022; 12(1):8711. PMID: 35610290.14. Morantes-Caballero JA, Fajardo Rodriguez HA. Effects of air pollution on acute exacerbation of chronic obstructive pulmonary disease: a descriptive retrospective study (pol-AECOPD). Int J Chron Obstruct Pulmon Dis. 2019; 14:1549–1557. PMID: 31371940.15. Xia X, Yao L, Lu J, Liu Y, Jing W, Li Y. A comparison analysis of causative impact of PM2. 5 on acute exacerbation of chronic obstructive pulmonary disease (COPD) in two typical cities in China. Atmosphere (Basel). 2021; 12(8):970.16. Aghapour M, Ubags ND, Bruder D, Hiemstra PS, Sidhaye V, Rezaee F, et al. Role of air pollutants in airway epithelial barrier dysfunction in asthma and COPD. Eur Respir Rev. 2022; 31(163):210112. PMID: 35321933.17. Bayram H, Devalia JL, Sapsford RJ, Ohtoshi T, Miyabara Y, Sagai M, et al. The effect of diesel exhaust particles on cell function and release of inflammatory mediators from human bronchial epithelial cells in vitro. Am J Respir Cell Mol Biol. 1998; 18(3):441–448. PMID: 9490663.18. Takizawa H, Ohtoshi T, Kawasaki S, Abe S, Sugawara I, Nakahara K, et al. Diesel exhaust particles activate human bronchial epithelial cells to express inflammatory mediators in the airways: a review. Respirology. 2000; 5(2):197–203. PMID: 10894110.19. Montgomery MT, Sajuthi SP, Cho SH, Everman JL, Rios CL, Goldfarbmuren KC, et al. Genome-wide analysis reveals mucociliary remodeling of the nasal airway epithelium induced by urban PM2.5 . Am J Respir Cell Mol Biol. 2020; 63(2):172–184. PMID: 32275839.20. Jia J, Xia J, Zhang R, Bai Y, Liu S, Dan M, et al. Investigation of the impact of PM2.5 on the ciliary motion of human nasal epithelial cells. Chemosphere. 2019; 233:309–318. PMID: 31176132.21. Li J, Hu Y, Liu L, Wang Q, Zeng J, Chen C. PM2.5 exposure perturbs lung microbiome and its metabolic profile in mice. Sci Total Environ. 2020; 721:137432. PMID: 32169651.22. Li N, He F, Liao B, Zhou Y, Li B, Ran P. Exposure to ambient particulate matter alters the microbial composition and induces immune changes in rat lung. Respir Res. 2017; 18(1):143. PMID: 28743263.23. Mariani J, Favero C, Spinazzè A, Cavallo DM, Carugno M, Motta V, et al. Short-term particulate matter exposure influences nasal microbiota in a population of healthy subjects. Environ Res. 2018; 162:119–126. PMID: 29291434.24. Niemeier-Walsh C, Ryan PH, Meller J, Ollberding NJ, Adhikari A, Reponen T. Exposure to traffic-related air pollution and bacterial diversity in the lower respiratory tract of children. PLoS One. 2021; 16(6):e0244341. PMID: 34166366.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Relationship between Airway Inflammation and Exacerbation in Chronic Obstructive Pulmonary Disease
- Adverse Effects of Air Pollution on Pulmonary Diseases
- Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea
- The Clinical Study of Clarithromycin for the Treatment of Acute Exacerbation of Chronic Obstructive Pulmonary Disease
- Pulmonary Strongyloidiasis Masquerading as Exacerbation of Chronic Obstructive Pulmonary Disease