J Korean Med Sci.
2023 Mar;38(9):e66. 10.3346/jkms.2023.38.e66.
Use of Antibiotics Within the Last 14 Days of Life in Korean Patients: A Nationwide Study
- Affiliations
-
- 1Department of Internal Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 2Division of Infectious Diseases, Department of Internal Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 3Division of Infectious Diseases, Department of Internal Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 4Division of Infectious Diseases, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Department of Internal Medicine, Pusan National University School of Medicine and Medical Research Institute, Pusan National University Hospital, Busan, Korea
- 6Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea
- 7Department of Internal Medicine, School of Medicine, Chungnam National University, Daejeon, Korea
- 8Division of Infectious Diseases, Department of Internal Medicine, Inje University College of Medicine, Busan, Korea
- 9Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, Jeju National University, Jeju, Korea
- 10Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- 11Division of Infectious Diseases, Department of Internal Medicine, Kyung Hee University Hospital, Kyung Hee University College of Medicine, Seoul, Korea
- 12Department of Internal Medicine, Yeungnam University Medical Center, Daegu, Korea
- 13Division of Infectious Diseases, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- KMID: 2540124
- DOI: http://doi.org/10.3346/jkms.2023.38.e66
Abstract
- Background
Antimicrobial prescriptions for serious chronic or acute illness nearing its end stages raise concerns about the potential for futile use, adverse events, increased multidrugresistant organisms, and significant patient and social cost burdens. This study investigated the nationwide situation of how antibiotics are prescribed to patients during the last 14 days of life to guide future actions.
Methods
This nationwide multicenter retrospective cohort study was conducted at 13 hospitals in South Korea from November 1 to December 31, 2018. All decedents were included in the study. Antibiotic use during the last two weeks of their lives was investigated.
Results
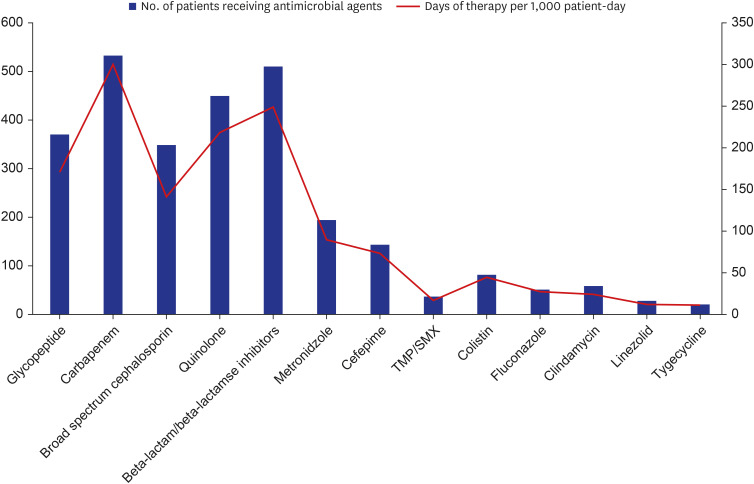
A total of 1,201 (88.9%) patients received a median of two antimicrobial agents during the last two weeks of their lives. Carbapenems were prescribed to approximately half of the patients (44.4%) in the highest amount (301.2 days of therapy per 1,000 patient-days).Among the patients receiving antimicrobial agents, 63.6% were inappropriate and only 327 patients (27.2%) were referred by infectious disease specialists. The use of carbapenem (odds ratio [OR], 1.51; 95% confidence interval [CI], 1.13–2.03; P = 0.006), underlying cancer (OR, 1.56; 95% CI, 1.20–2.01, P = 0.047), underlying cerebrovascular disease (OR, 1.88; 95% CI, 1.23–2.89, P = 0.004), and no microbiological testing (OR, 1.79; 95% CI, 1.15–2.73; P = 0.010) were independent predictors for inappropriate antibiotic prescribing.
Conclusion
A considerable number of antimicrobial agents are administered to patients with chronic or acute illnesses nearing their end-of-life, a high proportion of which are prescribed inappropriately. Consultation with an infectious disease specialist, in addition to an antimicrobial stewardship program, may be necessary to induce the optimal use of antibiotics.
Keyword
Figure
Reference
-
1. Kwon KT. Implementation of antimicrobial stewardship programs in end-of-life care. Infect Chemother. 2019; 51(2):89–97. PMID: 31270988.2. Tagashira Y, Kawahara K, Takamatsu A, Honda H. Antimicrobial prescribing in patients with advanced-stage illness in the antimicrobial stewardship era. Infect Control Hosp Epidemiol. 2018; 39(9):1023–1029. PMID: 30070197.3. Taverner J, Ross L, Bartlett C, Luthe M, Ong J, Irving L, et al. Antimicrobial prescription in patients dying from chronic obstructive pulmonary disease. Intern Med J. 2019; 49(1):66–73. PMID: 29740931.4. Wilder-Smith A, Gillespie T, Taylor DR. Antimicrobial use and misuse at the end of life: a retrospective analysis of a treatment escalation/limitation plan. J R Coll Physicians Edinb. 2019; 49(3):188–192. PMID: 31497784.5. Fedorowsky R, Bachner YG, Borer A, Ciobotaro P, Kushnir T. Use of antibiotics among end-of-life hospitalized patients with advanced directives: status examination and association with infectious disease consultation and physician burnout. Infect Control Hosp Epidemiol. 2019; 40(11):1222–1228. PMID: 31455445.6. Dyer J, Vaux L, Broom A, Broom J. Antimicrobial use in patients at the end of life in an Australian hospital. Infect Dis Health. 2019; 24(2):92–97. PMID: 30655096.7. Servid SA, Noble BN, Fromme EK, Furuno JP. Clinical intentions of antibiotics prescribed upon discharge to hospice care. J Am Geriatr Soc. 2018; 66(3):565–569. PMID: 29345756.8. Merel SE, Meier CA, McKinney CM, Pottinger PS. Antimicrobial use in patients on a comfort care protocol: a retrospective cohort study. J Palliat Med. 2016; 19(11):1210–1214. PMID: 27309999.9. Kwak YG, Moon C, Kim ES, Kim BN. Frequent prescription of antibiotics and high burden of antibiotic resistance among deceased patients in general medical wards of acute care hospitals in Korea. PLoS One. 2016; 11(1):e0146852. PMID: 26761461.10. Levin PD, Simor AE, Moses AE, Sprung CL. End-of-life treatment and bacterial antibiotic resistance: a potential association. Chest. 2010; 138(3):588–594. PMID: 20472860.11. Barlam TF, Cosgrove SE, Abbo LM, MacDougall C, Schuetz AN, Septimus EJ, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016; 62(10):e51–e77. PMID: 27080992.12. Albers G, Van den Block L, Vander Stichele R. The burden of caring for people with dementia at the end of life in nursing homes: a postdeath study among nursing staff. Int J Older People Nurs. 2014; 9(2):106–117. PMID: 24813859.13. van der Steen JT. Prolonged life and increased symptoms vs prolonged dying and increased comfort after antibiotic treatment in patients with dementia and pneumonia. Arch Intern Med. 2011; 171(1):93–94.14. Van Der Steen JT, Pasman HR, Ribbe MW, Van Der Wal G, Onwuteaka-Philipsen BD. Discomfort in dementia patients dying from pneumonia and its relief by antibiotics. Scand J Infect Dis. 2009; 41(2):143–151. PMID: 19065450.15. Givens JL, Jones RN, Shaffer ML, Kiely DK, Mitchell SL. Survival and comfort after treatment of pneumonia in advanced dementia. Arch Intern Med. 2010; 170(13):1102–1107. PMID: 20625013.16. Juthani-Mehta M, Malani PN, Mitchell SL. Antimicrobials at the end of life: an opportunity to improve palliative care and infection management. JAMA. 2015; 314(19):2017–2018. PMID: 26426830.17. Thompson AJ, Silveira MJ, Vitale CA, Malani PN. Antimicrobial use at the end of life among hospitalized patients with advanced cancer. Am J Hosp Palliat Care. 2012; 29(8):599–603. PMID: 22218916.18. Reinbolt RE, Shenk AM, White PH, Navari RM. Symptomatic treatment of infections in patients with advanced cancer receiving hospice care. J Pain Symptom Manage. 2005; 30(2):175–182. PMID: 16125033.19. Oh DY, Kim JH, Kim DW, Im SA, Kim TY, Heo DS, et al. Antibiotic use during the last days of life in cancer patients. Eur J Cancer Care (Engl). 2006; 15(1):74–79. PMID: 16441680.20. National Law Information Center. Act on Decisions on life-sustaining treatment for patients in hospice and palliative care or at the end of life. Updated 2016. Accessed April 17, 2020. http://www.law.go.kr/LSW/eng/engLsSc.do?menuId=2§ion=lawNm&query=life-sustaining+treatment+&x=0&y=0#liBgcolor0 .21. Kates OS, Krantz EM, Lee J, Klaassen J, Morris J, Mezheritsky I, et al. Association of physician orders for life-sustaining treatment with inpatient antimicrobial use at end of life in patients with cancer. Open Forum Infect Dis. 2021; 8(8):ofab361. PMID: 34395710.22. Yoon YK, Yang KS, Lee SE, Kim HJ, Sohn JW, Kim MJ. Effects of Group 1 versus Group 2 carbapenems on the susceptibility of Acinetobacter baumannii to carbapenems: a before and after intervention study of carbapenem-use stewardship. PLoS One. 2014; 9(6):e99101. PMID: 24911244.23. Horikoshi Y, Suwa J, Higuchi H, Kaneko T, Furuichi M, Aizawa Y, et al. Sustained pediatric antimicrobial stewardship program with consultation to infectious diseases reduced carbapenem resistance and infection-related mortality. Int J Infect Dis. 2017; 64:69–73. PMID: 28941633.24. McLaughlin M, Advincula MR, Malczynski M, Qi C, Bolon M, Scheetz MH. Correlations of antibiotic use and carbapenem resistance in enterobacteriaceae. Antimicrob Agents Chemother. 2013; 57(10):5131–5133. PMID: 23836188.25. Stocker H, Mehlhorn C, Jordan K, Eckholt L, Jefferys L, Arastéh K. Clinical and economic effects of an antimicrobial stewardship intervention in a surgical intensive care unit. Infection. 2020; 48(4):509–519. PMID: 32277409.26. Hung KC, Lee LW, Liew YX, Krishna L, Chlebicki MP, Chung SJ, et al. Antibiotic stewardship program (ASP) in palliative care: antibiotics, to give or not to give. Eur J Clin Microbiol Infect Dis. 2022; 41(1):29–36. PMID: 34414518.27. Gaw CE, Hamilton KW, Gerber JS, Szymczak JE. Physician perceptions regarding antimicrobial use in end-of-life care. Infect Control Hosp Epidemiol. 2018; 39(4):383–390. PMID: 29428002.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Meaning and Impact of Appropriate Use of Antibiotics
- Use of Prophylactic Antibiotics in Glaucoma Surgery: A Single Center's Experience
- The Effects of Intracameral Injection of Various Antibiotics on Rabbit Corneal Endothelium
- Microbiology and Antimicrobial Therapy for Diabetic Foot Infections
- Supplemental knowledge on survival of Thelohanellus kitauei spores in vitro