J Korean Neurosurg Soc.
2023 Mar;66(2):190-198. 10.3340/jkns.2021.0278.
A Study from a Highly Populated Country : Risk Factors Associated with Lower Back Pain in Middle-Aged Adults
- Affiliations
-
- 1Department of Neurosurgery, Faculty of Medicine UPN Veteran Jakarta, Jakarta, Indonesia
- 2Undergraduate Program, Faculty of Medicine UPN Veteran Jakarta, Jakarta, Indonesia
- KMID: 2539880
- DOI: http://doi.org/10.3340/jkns.2021.0278
Abstract
Objective
: Low back pain (LBP) is a global health problem that affects the productivity of the patients. Several factors such as individual, occupational, and psychosocial factors increase the risk of LBP. However, only a few studies investigated those factors, especially in middle adulthood in Indonesia. Indonesia is a country with a young population that has been rapidly developing in recent years. This study was conducted to find out the factors associated with LBP in middle adulthood.
Methods
: This study is a cross-sectional observational analytic study using a convenience sampling method with a total sample of 3005 respondents. Data were collected using a questionnaire which was then analyzed using the chi-square test, Kolmogorovsmirnov, Spearman’s Rank, and logistic regression test.
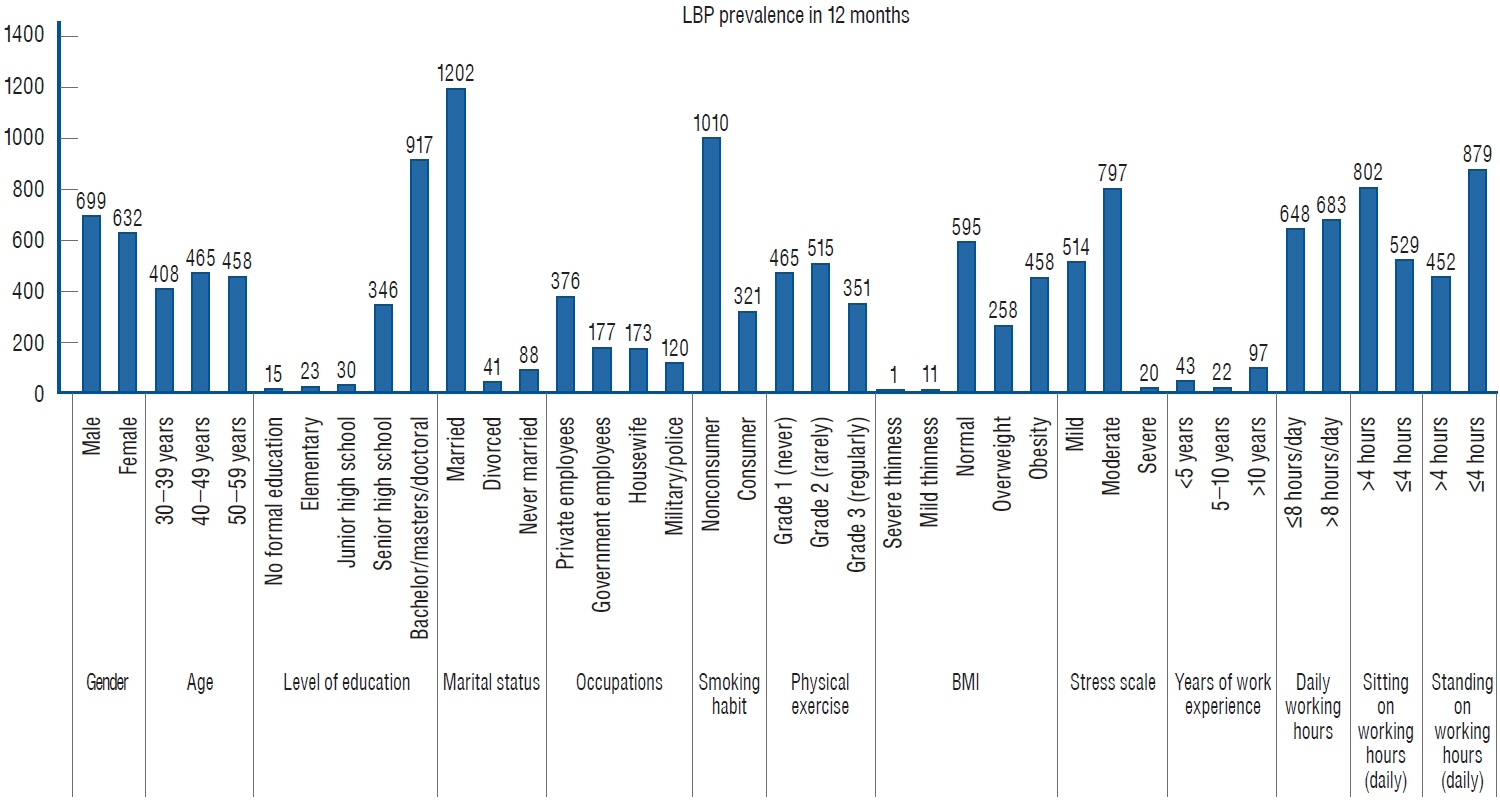
Results
: From the result of this study, it was found that the 12-month prevalence of LBP in middle-aged adults was 44,29%. Female (odds ratio [OR], 1.3; 95% confidence interval [Cl], 1.098–1.545; p=0.002), lack of physical exercises (OR, 0.87; 95% Cl, 0.794–0.959; p=0.005), high body mass index (OR, 1.09; 95% Cl, 1.009–1.187; p=0.002), stress level (OR, 1.26; 95% Cl, 1.088–1.458; p=0.002), and years of work experience (OR, 1.1; 95% Cl, 1.001–1.225; p=0.047) were determined as risk factors that significantly associated with LBP.
Conclusion
: LBP is quite common among middle-aged adults in Indonesia. Female gender, higher body mass index, lack of physical activity, stress level, and years of work experience were all potential risk factors for LBP in middle-aged adults. Middle-aged adults in Indonesia should be aware of LBP and avoid disabilities by identifying risk factors that may worsen LBP in the future.
Keyword
Figure
Reference
-
References
1. 2021 World Population Review : Indonesia Population 2021. Available at : https://worldpopulationreview.com/countries/indonesiapopulation.2. Abebe AD, Gebrehiwot EM, Lema S, Abebe TW. Prevalence of low back pain and associated risk factors among Adama Hospital Medical College Staff, Ethiopia. EJPM. 3:188–192. 2015.3. Al-Arfaj AS, Al-Saleh SS, Alballa SR, Al-Dalaan AN, Bahabri SA, Al-Sekeit MA, et al. How common is back pain in Al-Qaseem region. Saudi Med J. 24:170–173. 2003.4. ALMaghrabi AO, ALSharif FH, ALMutary HH. Prevalence of low back pain and associated risk factors among nurses - review. IJNRHN. 8:150–158. 2021.5. Alnaami I, Awadalla NJ, Alkhairy M, Alburidy S, Alqarni A, Algarni A, et al. Prevalence and factors associated with low back pain among health care workers in southwestern Saudi Arabia. BMC Musculoskelet Disord. 20:56. 2019.6. Barros Dos Santos AO, Pinto de Castro JB, Lima VP, da Silva EB, de Souza Vale RG. Effects of physical exercise on low back pain and cortisol levels: a systematic review with meta-analysis of randomized controlled trials. Pain Manag. 11:49–57. 2021.7. Bento TPF, Genebra CVDS, Maciel NM, Cornelio GP, Simeão SFAP, Vitta A. Low back pain and some associated factors: is there any difference between genders? Braz J Phys Ther. 24:79–87. 2020.8. Borg-Stein J, Dugan SA. Musculoskeletal disorders of pregnancy, delivery and postpartum. Phys Med Rehabil Clin N Am. 18:459–476. 2007.9. Choi S, Nah S, Jang HD, Moon JE, Han S. Association between chronic low back pain and degree of stress: a nationwide cross-sectional study. Sci Rep. 11:14549. 2021.10. Diallo SYK, Mweu MM, Mbuya SO, Mwanthi MA. Prevalence and risk factors for low back pain among university teaching staff in Nairobi, Kenya: a cross-sectional study. F1000Res. 8:808. 2019.11. Djalalinia S, Saeedi Moghaddam S, Moradi-Lakeh M, Shahraz S, Naghavi M, Murray CJL, et al. Prevalence and years lived with disability of 310 diseases and injuries in Iran and its neighboring countries, 1990-2015: findings from Global Burden of Disease Study 2015. Arch Iran Med. 20:392–402. 2017.12. Fernández-de-las-Peñas C, Hernández-Barrera V, Alonso-Blanco C, Palacios-Ceña D, Carrasco-Garrido P, Jiménez-Sánchez S, et al. Prevalence of neck and low back pain in community-dwelling adults in Spain: a population-based national study. Spine (Phila Pa 1976). 36:E213–E219. 2011.13. Fujii T, Matsudaira K. Prevalence of low back pain and factors associated with chronic disabling back pain in Japan. Eur Spine J. 22:432–438. 2013.14. Ganesan S, Acharya AS, Chauhan R, Acharya S. Prevalence and risk factors for low back pain in 1,355 young adults: a cross-sectional study. Asian Spine J. 11:610–617. 2017.15. Han IH. Pregnancy and spinal problems. Curr Opin Obstet Gynecol. 22:477–481. 2010.16. Hannibal KE, Bishop MD. Chronic stress, cortisol dysfunction, and pain: a psychoneuroendocrine rationale for stress management in pain rehabilitation. Phys Ther. 94:1816–1825. 2014.17. Heuch I, Hagen K, Heuch I, Nygaard Ø, Zwart JA. The impact of body mass index on the prevalence of low back pain: the HUNT study. Spine (Phila Pa 1976). 35:764–768. 2010.18. Hoy D, Bain C, Williams G, March L, Brooks P, Blyth F, et al. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 64:2028–2037. 2012.19. Hoy D, March L, Brooks P, Blyth F, Woolf A, Bain C, et al. The global burden of low back pain: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 73:968–974. 2014.20. Karahan A, Kav S, Abbasoglu A, Dogan N. Low back pain: prevalence and associated risk factors among hospital staff. J Adv Nurs. 65:516–524. 2009.21. Kurniasari A. The midlife crisis and the solutions. Sosio Informa. 3:165–179. 2017.22. Lachman ME, Teshale S, Agrigoroaei S. Midlife as a Pivotal period in the life course: balancing growth and decline at the crossroads of youth and old age. Int J Behav Dev. 39:20–31. 2015.23. Lezin N, Watkins-Castillo S. The impact of musculoskeletal disorders on Americans—opportunities for action : The Burden of Musculoskeletal Diseases in the United States: Prevalence, Societal, and Economic Cost. ed 3rd. Rosemont: United States Bone and Joint Initiative;2016. p. 71–73.24. Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 17 Suppl 2:3–10. 2014.25. Marras WS, Cutlip RG, Burt SE, Waters TR. National occupational research agenda (NORA) future directions in occupational musculoskeletal disorder health research. Appl Ergon. 40:15–22. 2009.26. Mijena GF, Geda B, Dheresa M, Fage SG. Low back pain among nurses working at public hospitals in Eastern Ethiopia. J Pain Res. 13:1349–1357. 2020.27. Novitasari DD, Sadeli HA, Soenggono A, Sofiatin Y, Sukandar H, Roesli RM. Prevalence and characteristics of low back pain among productive age population in Jatinangor. Althea Med J. 3:469–476. 2016.28. Nurul I, Haslinda A, Saidi M, Shamsul B, Zailina H. Prevalence of low back pain and its risk factors among school teachers. Am J Appl Sci. 7:634–639. 2010.29. Padayachy K, Vawda GHM, Shaik J, McCarthy PW. The immediate effect of low back manipulation on serum cortisol levels in adult males with mechanical low back pain. Clin Chiropr. 13:246–252. 2010.30. Parreira P, Maher CG, Steffens D, Hancock MJ, Ferreira ML. Risk factors for low back pain and sciatica: an umbrella review. Spine J. 18:1715–1721. 2018.31. Pin TL, Effendy E. Hubungan Kebiasaan Berolahraga Dengan Tingkat Stres Pada Mahasiswa Fakultas kedokteran universitas sumatera utara tahun masuk 2008. Sumatera Utara: Universitas Sumatera Utara;2011.32. Prieto-González P, Šutvajová M, Lesňáková A, Bartík P, Buľáková K, Friediger T. Back pain prevalence, intensity, and associated risk factors among female teachers in slovakia during the COVID-19 pandemic: a cross-sectional study. Healthcare (Basel). 9:860. 2021.33. Safarina L, Dewi SN. Pengaruh senam yoga terhadap skala nyeri low back pain (LBP) pada dewasa menengah di wilayah kerja puskesmas cimahi tengah. Sekolah Tinggi Ilmu Kesehatan Jendral Achmad Yani Cimahi. 1:150–157. 2018.34. Shiri R, Solovieva S, Husgafvel-Pursiainen K, Taimela S, Saarikoski LA, Huupponen R, et al. The association between obesity and the prevalence of low back pain in young adults: the cardiovascular risk in young finns study. Am J Epidemiol. 167:1110–1119. 2008.35. Şimşek Ş, Yağcı N, Şenol H. Prevalence of and risk factors for low back pain among healthcare workers in Denizli. Agri. 29:71–78. 2017.36. Skela-Savič B, Pesjak K, Hvalič-Touzery S. Low back pain among nurses in Slovenian hospitals: cross-sectional study. Int Nurs Rev. 64:544–551. 2017.37. Smith DR, Mihashi M, Adachi Y, Shouyama Y, Mouri F, Ishibashi N, et al. Menstrual disorders and their influence on low back pain among Japanese nurses. Ind Health. 47:301–312. 2009.38. Sugano A, Nomura T. Influence of water exercise and land stretching on salivary cortisol concentrations and anxiety in chronic low back pain patients. J Physiol Anthropol Appl Human Sci. 19:175–180. 2000.39. Svensson HO, Andersson GB, Hagstad A, Jansson PO. The relationship of low-back pain to pregnancy and gynecologic factors. Spine (Phila Pa 1976). 15:371–375. 1990.40. Tissot F, Messing K. Perimenstrual symptoms and working conditions among hospital workers in Quebec. Am J Ind Med. 27:511–522. 1995.41. Wicaksono PD. Validity and reliability of nordic musculoskeletal questionnaire (NMQ) on giriloyo tourism village batik workers group in bantul special region of yogyakarta 2019. Yogyakarta: Universitas Pembangunan Nasional Veteran Jakarta;2019.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associations Between Body Composition and Chronic Low Back Pain in Adults: Data from the 2009 Korea National Health and Nutrition Examination Survey
- The Risk Factors of Industrial Low Back Pain among Shipyard Workers
- Evaluation of Metabolic Syndrome in Patients with Chronic Low Back Pain: Using the Fourth Korea National Health and Nutrition Examination Survey Data
- An Epidemiologic Study of Low Back Pain of Women Working at a General Hospital
- Differences in Risk Factors for Suicidal Ideation among Younger, Middle-Aged, and Older Adults