J Korean Assoc Oral Maxillofac Surg.
2023 Feb;49(1):43-48. 10.5125/jkaoms.2023.49.1.43.
Energy-dispersive X-ray spectroscopic investigation of a fractured non-submerged dental implant associated with abutment fracture
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea
- 2Oral and Maxillofacial Microvascular Reconstruction LAB, Brong Ahafo Regional Hospital, Sunyani, Ghana
- KMID: 2539703
- DOI: http://doi.org/10.5125/jkaoms.2023.49.1.43
Abstract
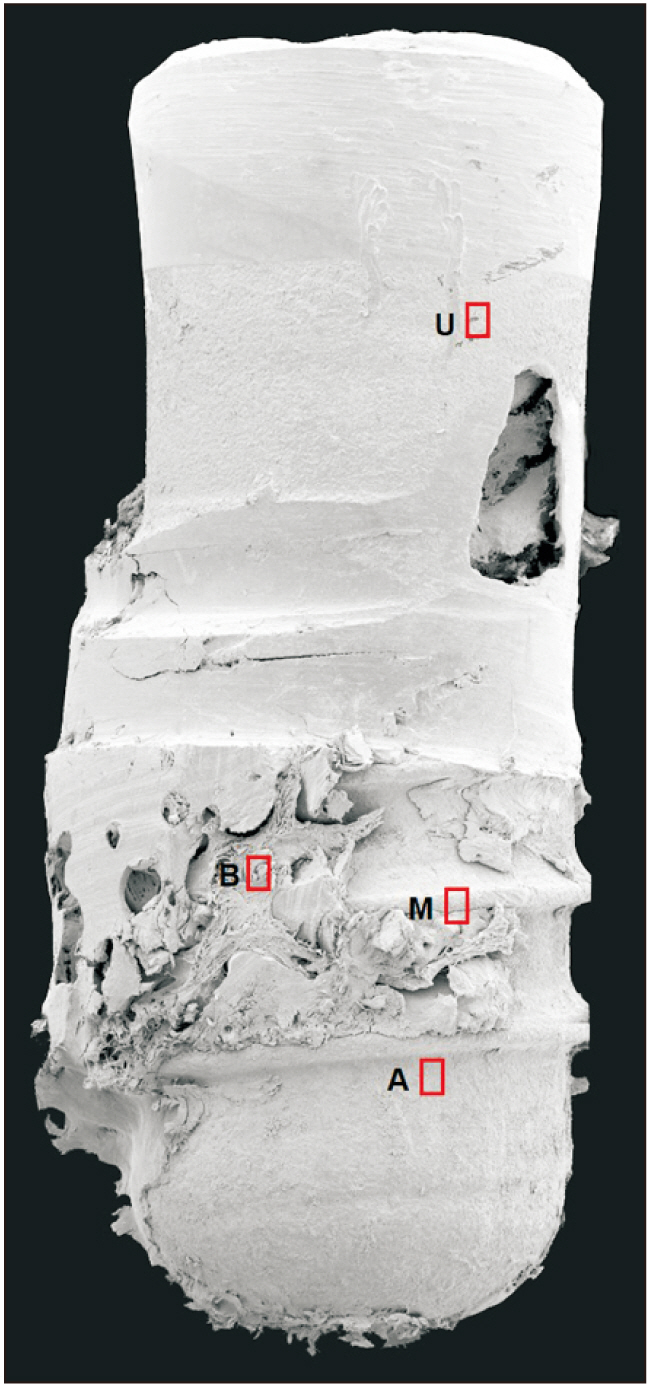
- The biocompatibility and durability of implant fixtures are major concerns for dentists and patients. Mechanical complications of the implant include abutment screw loosening, screw fracture, loss of implant prostheses, and implant fracture. This case report aims to describe management of a case of fixture damage that occurred after screw fracture in a tissue level, internal connection implant and microscopic evaluation of the fractured fixture. A trephine bur was used to remove the fixture, and the socket was grafted using allogeneic bone material. The failed implant was examined by scanning electron microscopy (SEM) and energy dispersive X-ray spectroscopy (EDS), which revealed a fractured fixture with both normal and irregular bone patterns. The SEM and EDS results give an enlightenment of the failed fixture surface micromorphology with microfracture and contaminated chemical compositions. Noticeably, the significantly high level of gold (Au) on the implant surface and the trace amounts of Au and titanium (Ti) in the bone tissue were recorded, which might have resulted from instability and micro-movement of the implant-abutment connection over an extended period of time. Further study with larger number of patient and different types of implants is needed for further conclusion.
Keyword
Figure
Reference
-
References
1. Albrektsson T, Zarb G, Worthington P, Eriksson AR. 1986; The long-term efficacy of currently used dental implants: a review and proposed criteria of success. Int J Oral Maxillofac Implants. 1:11–25. PMID: 3527955.2. Berglundh T, Persson L, Klinge B. 2002; A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol. 29 Suppl 3:197–212. discussion 232–3. https://doi.org/10.1034/j.1600-051x.29.s3.12.x. DOI: 10.1034/j.1600-051X.29.s3.12.x. PMID: 12787220.3. Rangert B, Krogh PH, Langer B, Van Roekel N. 1995; Bending overload and implant fracture: a retrospective clinical analysis. Int J Oral Maxillofac Implants. 10:326–34. PMID: 7615329.4. Balshi TJ. 1996; An analysis and management of fractured implants: a clinical report. Int J Oral Maxillofac Implants. 11:660–6. PMID: 8908866.5. Singh A, Singh A, Vivek R, Chaturvedi TP, Chauhan P, Gupta S. 2013; SEM analysis and management of fracture dental implant. Case Rep Dent. 2013:270385. https://doi.org/10.1155/2013/270385. DOI: 10.1155/2013/270385. PMID: 23710372. PMCID: PMC3655462.6. Sánchez-Pérez A, Moya-Villaescusa MJ, Jornet-Garcia A, Gomez S. 2010; Etiology, risk factors and management of implant fractures. Med Oral Patol Oral Cir Bucal. 15:e504–8. https://doi.org/10.4317/medoral.15.e504. DOI: 10.4317/medoral.15.e504. PMID: 20038899.7. Wee K, Lee BA. 2019; Implant fracture after screw fracture in a tissue-level implant: a case report. Implantology. 23:229–34. https://doi.org/10.32542/implantology.2019020. DOI: 10.32542/implantology.2019020.8. Delgado-Ruiz R, Romanos G. 2018; Potential causes of titanium particle and ion release in implant dentistry: a systematic review. Int J Mol Sci. 19:3585. https://doi.org/10.3390/ijms19113585. DOI: 10.3390/ijms19113585. PMID: 30428596. PMCID: PMC6274707.9. Hellsing M. 1997; Comparative surface analysis of four dental implant systems. J Dent Assoc S Afr. 52:399–402. PMID: 9461954.10. Sawase T, Hai K, Yoshida K, Baba K, Hatada R, Atsuta M. 1998; Spectroscopic studies of three osseointegrated implants. J Dent. 26:119–24. https://doi.org/10.1016/s0300-5712(96)00080-2. DOI: 10.1016/S0300-5712(96)00080-2. PMID: 9540308.11. Shibli JA, Marcantonio E, dʼAvila S, Guastaldi AC, Marcantonio E Jr. 2005; Analysis of failed commercially pure titanium dental implants: a scanning electron microscopy and energy-dispersive spectrometer x-ray study. J Periodontol. 76:1092–9. https://doi.org/10.1902/jop.2005.76.7.1092. DOI: 10.1902/jop.2005.76.7.1092. PMID: 16018751.12. Romeed SA, Malik R, Dunne SM. 2013; Marginal bone loss influence on the biomechanics of single implant crowns. J Craniofac Surg. 24:1459–65. https://doi.org/10.1097/SCS.0b013e3182902db0. DOI: 10.1097/SCS.0b013e3182902db0. PMID: 23851832.13. Jimbo R, Halldin A, Janda M, Wennerberg A, Vandeweghe S. 2013; Vertical fracture and marginal bone loss of internal-connection implants: a finite element analysis. Int J Oral Maxillofac Implants. 28:e171–6. https://doi.org/10.11607/jomi.3052. DOI: 10.11607/jomi.3052. PMID: 23869374.14. Shemtov-Yona K, Rittel D. 2014; Identification of failure mechanisms in retrieved fractured dental implants. Eng Fail Anal. 38:58–65. https://doi.org/10.1016/j.engfailanal.2014.01.002. DOI: 10.1016/j.engfailanal.2014.01.002.15. Apaza-Bedoya K, Tarce M, Benfatti CAM, Henriques B, Mathew MT, Teughels W, et al. 2017; Synergistic interactions between corrosion and wear at titanium-based dental implant connections: a scoping review. J Periodontal Res. 52:946–54. https://doi.org/10.1111/jre.12469. DOI: 10.1111/jre.12469. PMID: 28612506.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Removal of fractured implant screws: case report
- Repairment of abutment and abutment screw fracture in implant prosthesis: A case report
- Implant Fracture After Screw Fracture in a TissueLevel Implant: A Case Report
- Alternative Method to Salvage an Internally Damaged Implant using Cast Post
- Comparison of implant component fractures in external and internal type: A 12-year retrospective study