J Korean Assoc Oral Maxillofac Surg.
2023 Feb;49(1):30-42. 10.5125/jkaoms.2023.49.1.30.
Guidance and rationale for the immediate implant placement in the maxillary molar
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea
- 2Oral and Maxillofacial Microvascular Reconstruction LAB, Brong Ahafo Regional Hospital, Sunyani, Ghana
- KMID: 2539702
- DOI: http://doi.org/10.5125/jkaoms.2023.49.1.30
Abstract
Objectives
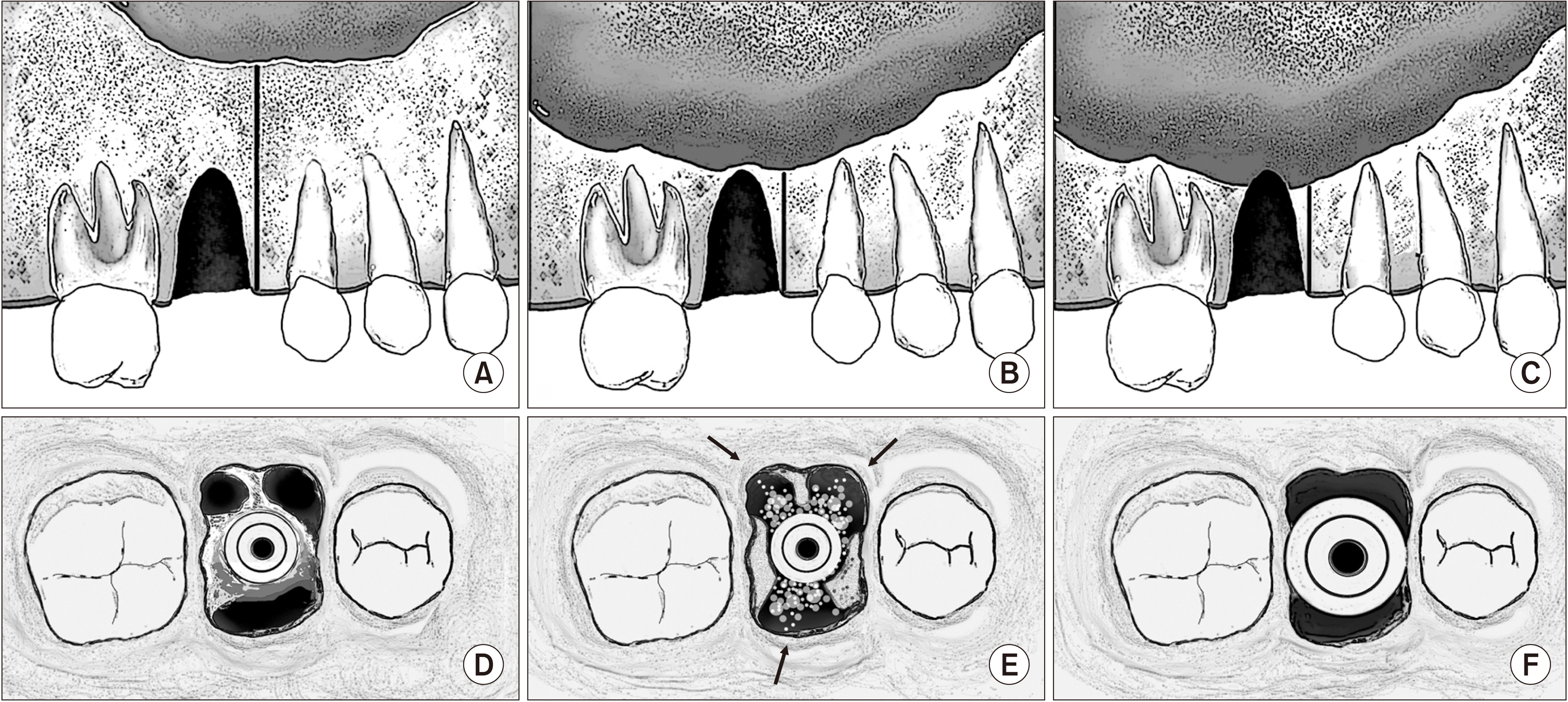
While the reliability of immediate implant placement in the maxillary molar has been discussed, its significance is questionable. There have been no guidelines for case selection and surgical technique for successful treatment outcomes of immediate maxillary molar implants. Therefore, in this study, we classified alveolar bone height and socket morphology of the maxillary molar to establish guidelines for immediate implant placement.
Materials and Methods
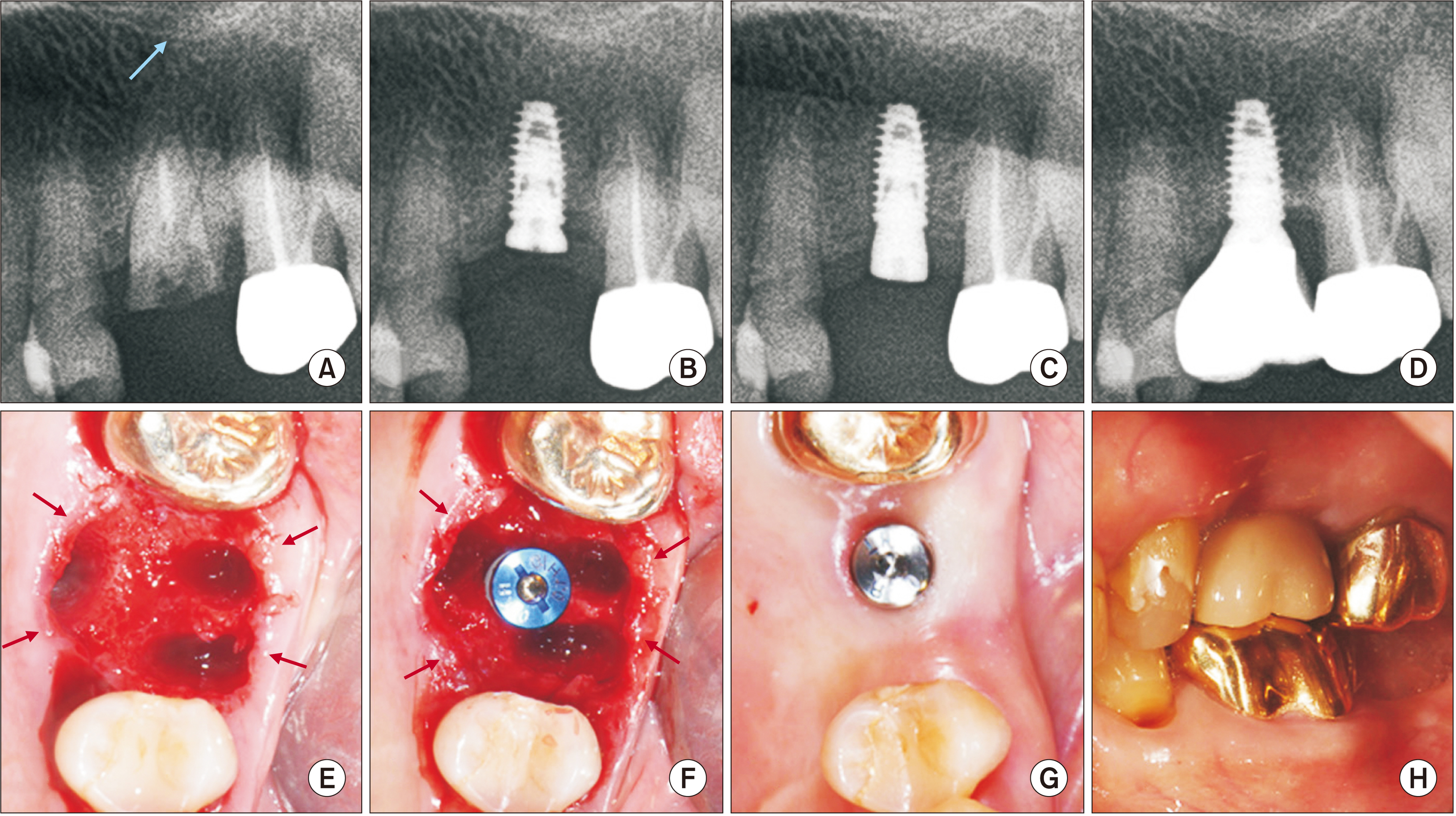
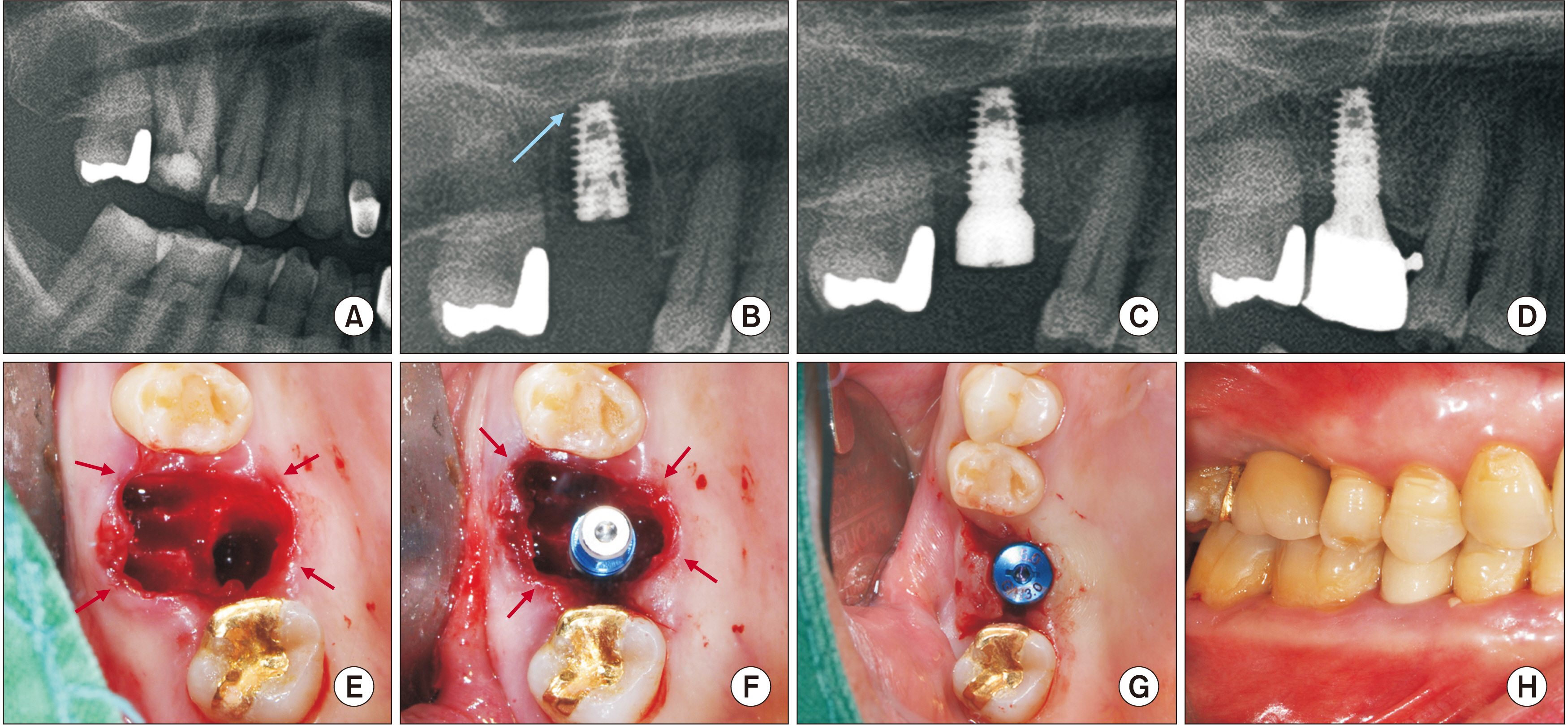
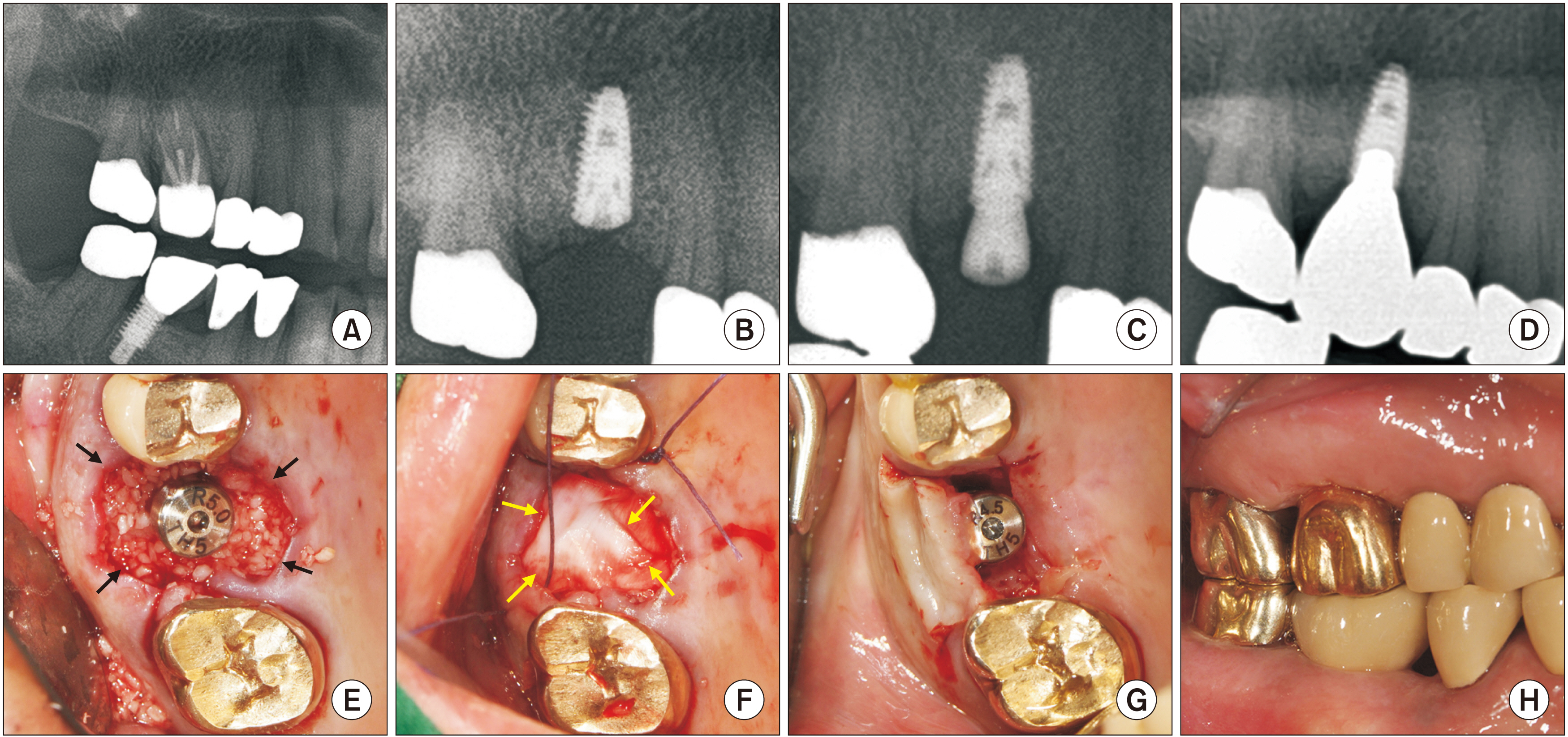
From 2011 to 2019, we retrospectively analyzed 106 patients with 148 immediate implants at the Department of Oral and Maxillofacial Surgery, Seoul National University Dental Hospital. Inclusion and exclusion criteria were applied, and patient characteristics and treatment results were evaluated clinically and radiologically.
Results
A total of 29 tapered, sand-blasted, large-grit, and acid-etched (SLA) surfaces of implants were placed in 26 patients. The mean patient age was 64.88 years. Two implants failed and were reinstalled, resulting in a 93.10% survival rate. Fluctuating marginal bone level changes indicating bone regeneration and bone loss were observed in the first year following installation and remained stable after one year of prosthesis loading, with an average bone loss of 0.01±0.01 mm on the distal side and 0.03±0.03 mm on the mesial side.
Conclusion
This clinical study demonstrated the significance of immediate implant placement in maxillary molars as a reliable treatment with a high survival rate using tapered SLA implants. With an accurate approach to immediate implantation, surgical intervention and treatment time can be reduced, resulting in patient satisfaction and comfort.
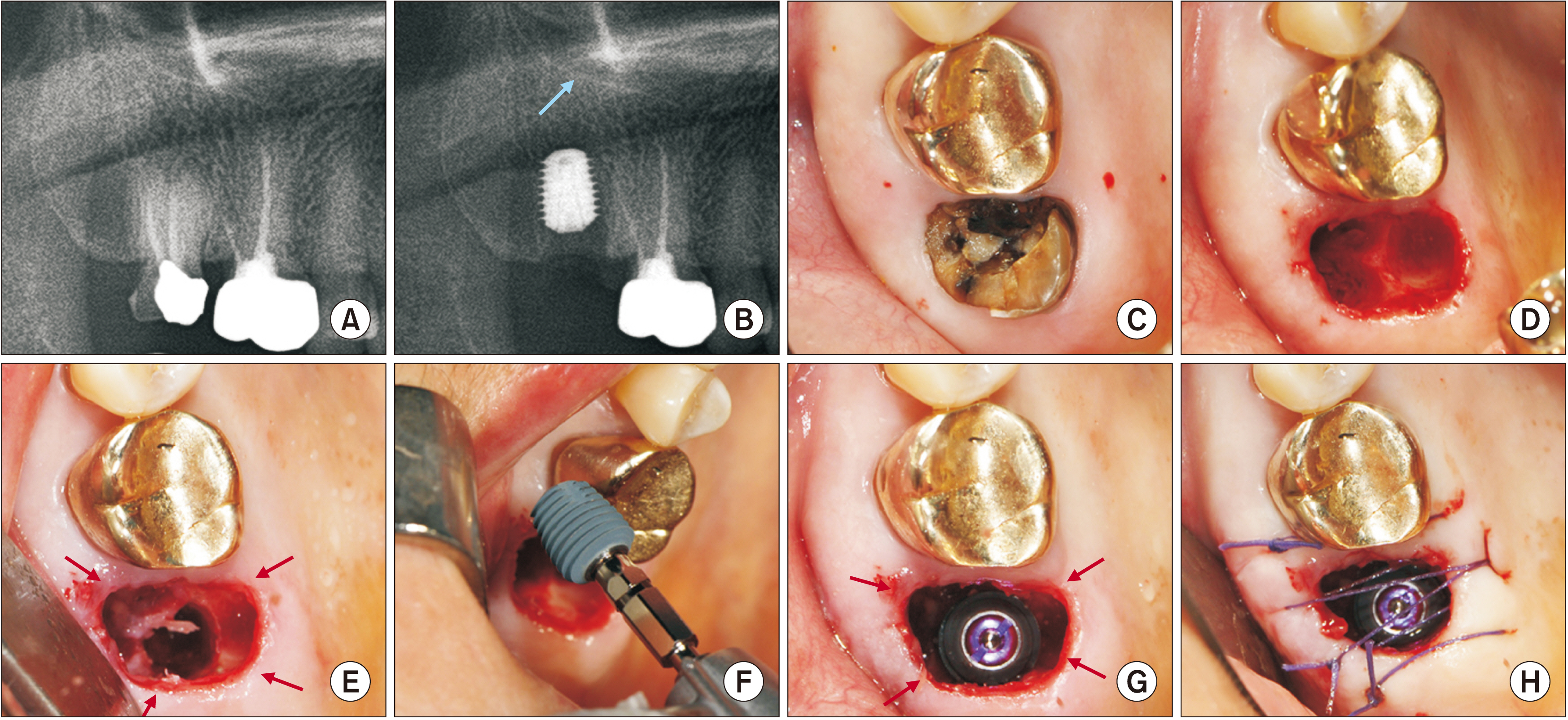
Figure
Reference
-
References
1. Demircan S, Çankaya AB. 2016; Is immediate implant placement possible in the maxillary molar area? An anatomical study. Quintessence Int. 47:853–9. https://doi.org/10.3290/j.qi.a36886. DOI: 10.3290/j.qi.a36886. PMID: 27669721.2. Ketabi M, Deporter D, Atenafu EG. 2016; A systematic review of outcomes following immediate molar implant placement based on recently published studies. Clin Implant Dent Relat Res. 18:1084–94. https://doi.org/10.1111/cid.12390. DOI: 10.1111/cid.12390. PMID: 26856388.3. Atieh MA, Payne AG, Duncan WJ, de Silva RK, Cullinan MP. 2010; Immediate placement or immediate restoration/loading of single implants for molar tooth replacement: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 25:401–15. PMID: 20369102.4. Smith RB, Tarnow DP. 2013; Classification of molar extraction sites for immediate dental implant placement: technical note. Int J Oral Maxillofac Implants. 28:911–6. https://doi.org/10.11607/jomi.2627. DOI: 10.11607/jomi.2627. PMID: 23748327.5. Ananda GK, Nambiar P, Mutalik S, Shanmuhasuntharam P. 2015; Anatomical considerations for implant placements in first maxillary molar extracted sites in East Asian patients. Surg Radiol Anat. 37:1099–108. https://doi.org/10.1007/s00276-015-1473-0. DOI: 10.1007/s00276-015-1473-0. PMID: 25850735.6. Fugazzotto PA. 2008; Implant placement at the time of maxillary molar extraction: treatment protocols and report of results. J Periodontol. 79:216–23. https://doi.org/10.1902/jop.2008.070338. DOI: 10.1902/jop.2008.070338. PMID: 18251636.7. Ragucci GM, Elnayef B, Criado-Cámara E, Del Amo FS, Hernández-Alfaro F. 2020; Immediate implant placement in molar extraction sockets: a systematic review and meta-analysis. Int J Implant Dent. 6:40. https://doi.org/10.1186/s40729-020-00235-5. DOI: 10.1186/s40729-020-00235-5. PMID: 32770283. PMCID: PMC7413966.8. Atieh MA, Alsabeeha NH, Duncan WJ, de Silva RK, Cullinan MP, Schwass D, et al. 2013; Immediate single implant restorations in mandibular molar extraction sockets: a controlled clinical trial. Clin Oral Implants Res. 24:484–96. https://doi.org/10.1111/j.1600-0501.2011.02415.x. DOI: 10.1111/j.1600-0501.2011.02415.x. PMID: 22276690.9. Checchi V, Felice P, Zucchelli G, Barausse C, Piattelli M, Pistilli R, et al. 2017; Wide diameter immediate post-extractive implants vs delayed placement of normal-diameter implants in preserved sockets in the molar region: 1-year post-loading outcome of a randomised controlled trial. Eur J Oral Implantol. 10:263–78. PMID: 28944355.10. Meijer HJA, Raghoebar GM. 2020; Immediate implant placement in molar extraction sites: a 1-year prospective case series pilot study. Int J Implant Dent. 6:3. https://doi.org/10.1186/s40729-019-0201-7. DOI: 10.1186/s40729-019-0201-7. PMID: 32048081. PMCID: PMC7013013.11. Nguyen TTH, Eo MY, Kuk TS, Myoung H, Kim SM. 2019; Rehabilitation of atrophic jaw using iliac onlay bone graft combined with dental implants. Int J Implant Dent. 5:11. https://doi.org/10.1186/s40729-019-0163-9. DOI: 10.1186/s40729-019-0163-9. PMID: 30887237. PMCID: PMC6423193.12. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC. Vandenbroucke JP; STROBE Initiative. 2007; The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 147:573–7. https://doi.org/10.7326/0003-4819-147-8-200710160-00010. DOI: 10.7326/0003-4819-147-8-200710160-00010. PMID: 17938396.13. Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, et al. 2008; Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa consensus conference. Implant Dent. 17:5–15. https://doi.org/10.1097/id.0b013e3181676059. DOI: 10.1097/ID.0b013e3181676059. PMID: 18332753.14. Yuan X, Pei X, Zhao Y, Li Z, Chen CH, Tulu US, et al. 2018; Biomechanics of immediate postextraction implant osseointegration. J Dent Res. 97:987–94. https://doi.org/10.1177/0022034518765757. DOI: 10.1177/0022034518765757. PMID: 29608868. PMCID: PMC6055256.15. Makishi S, Saito K, Ohshima H. 2017; Osteopontin-deficiency disturbs direct osteogenesis in the process of achieving osseointegration following immediate placement of endosseous implants. Clin Implant Dent Relat Res. 19:496–504. https://doi.org/10.1111/cid.12467. DOI: 10.1111/cid.12467. PMID: 27943627.16. Botticelli D, Persson LG, Lindhe J, Berglundh T. 2006; Bone tissue formation adjacent to implants placed in fresh extraction sockets: an experimental study in dogs. Clin Oral Implants Res. 17:351–8. https://doi.org/10.1111/j.1600-0501.2006.01270.x. DOI: 10.1111/j.1600-0501.2006.01270.x. PMID: 16907764.17. Botticelli D, Renzi A, Lindhe J, Berglundh T. 2008; Implants in fresh extraction sockets: a prospective 5-year follow-up clinical study. Clin Oral Implants Res. 19:1226–32. https://doi.org/10.1111/j.1600-0501.2008.01620.x. DOI: 10.1111/j.1600-0501.2008.01620.x. PMID: 19040437.18. Matarasso S, Salvi GE, Iorio Siciliano V, Cafiero C, Blasi A, Lang NP. 2009; Dimensional ridge alterations following immediate implant placement in molar extraction sites: a six-month prospective cohort study with surgical re-entry. Clin Oral Implants Res. 20:1092–8. https://doi.org/10.1111/j.1600-0501.2009.01803.x. DOI: 10.1111/j.1600-0501.2009.01803.x. PMID: 19719737.19. Adell R, Lekholm U, Brånemark PI, Lindhe J, Rockler B, Eriksson B, et al. 1985; Marginal tissue reactions at osseointegrated titanium fixtures. Swed Dent J Suppl. 28:175–81. DOI: 10.1016/s0300-9785(86)80010-2. PMID: 3904060.20. Javaid MA, Khurshid Z, Zafar MS, Najeeb S. 2016; Immediate implants: clinical guidelines for esthetic outcomes. Dent J (Basel). 4:21. https://doi.org/10.3390/dj4020021. DOI: 10.3390/dj4020021. PMID: 29563463. PMCID: PMC5851264.21. Amato F, Polara G. 2018; Immediate implant placement in single-tooth molar extraction sockets: a 1- to 6-year retrospective clinical study. Int J Periodontics Restorative Dent. 38:495–501. https://doi.org/10.11607/prd.3179. DOI: 10.11607/prd.3179. PMID: 29590222.22. Zita Gomes R, de Vasconcelos MR, Lopes Guerra IM, de Almeida RAB, de Campos Felino AC. 2017; Implant stability in the posterior maxilla: a controlled clinical trial. Biomed Res Int. 2017:6825213. https://doi.org/10.1155/2017/6825213. DOI: 10.1155/2017/6825213. PMID: 28626763. PMCID: PMC5463151.23. Acocella A, Bertolai R, Sacco R. 2010; Modified insertion technique for immediate implant placement into fresh extraction socket in the first maxillary molar sites: a 3-year prospective study. Implant Dent. 19:220–8. https://doi.org/10.1097/id.0b013e3181dbe2fe. DOI: 10.1097/ID.0b013e3181dbe2fe. PMID: 20523178.24. Nguyen TTH, Eo MY, Seo MH, Kim SM. 2022; Analysis of acute sinusitis-related early failed implant surface: a combined histological, electron microscopy, and X-ray spectroscopy approach. Maxillofac Plast Reconstr Surg. 44:18. https://doi.org/10.1186/s40902-022-00346-6. DOI: 10.1186/s40902-022-00346-6. PMID: 35469096. PMCID: PMC9038979.25. Andre A, Ogle OE. 2021; Vertical and horizontal augmentation of deficient maxilla and mandible for implant placement. Dent Clin North Am. 65:103–23. https://doi.org/10.1016/j.cden.2020.09.009. DOI: 10.1016/j.cden.2020.09.009. PMID: 33213705.26. Jun SH, Park CJ, Hwang SH, Lee YK, Zhou C, Jang HS, et al. 2018; The influence of bone graft procedures on primary stability and bone change of implants placed in fresh extraction sockets. Maxillofac Plast Reconstr Surg. 40:8. https://doi.org/10.1186/s40902-018-0148-2. DOI: 10.1186/s40902-018-0148-2. PMID: 29725586. PMCID: PMC5915983.27. Troeltzsch M, Troeltzsch M, Kauffmann P, Gruber R, Brockmeyer P, Moser N, et al. 2016; Clinical efficacy of grafting materials in alveolar ridge augmentation: a systematic review. J Craniomaxillofac Surg. 44:1618–29. https://doi.org/10.1016/j.jcms.2016.07.028. DOI: 10.1016/j.jcms.2016.07.028. PMID: 27622971.28. Kolerman R, Qahaz N, Barnea E, Mijiritsky E, Chaushu L, Tal H, et al. 2020; Allograft and collagen membrane augmentation procedures preserve the bone level around implants after immediate placement and restoration. Int J Environ Res Public Health. 17:1133. https://doi.org/10.3390/ijerph17041133. DOI: 10.3390/ijerph17041133. PMID: 32053928. PMCID: PMC7068471.29. Farina R, Trombelli L. 2011; Wound healing of extraction sockets. Endod Topics. 25:16–43. https://doi.org/10.1111/etp.12016. DOI: 10.1111/etp.12016.30. Cochran DL, Schenk RK, Lussi A, Higginbottom FL, Buser D. 1998; Bone response to unloaded and loaded titanium implants with a sandblasted and acid-etched surface: a histometric study in the canine mandible. J Biomed Mater Res. 40:1–11. https://doi.org/10.1002/(sici)1097-4636(199804)40:1%3C1::aid-jbm1%3E3.0.co;2-q. DOI: 10.1002/(SICI)1097-4636(199804)40:1<1::AID-JBM1>3.0.CO;2-Q. PMID: 9511093.31. Sayin Ozel G, Inan O, Secilmis Acar A, Alniacik Iyidogan G, Dolanmaz D, Yildirim G. 2021; Stability of dental implants with sandblasted and acid-etched (SLA) and modified (SLActive) surfaces during the osseointegration period. J Dent Res Dent Clin Dent Prospects. 15:226–31. https://doi.org/10.34172/joddd.2021.037. DOI: 10.34172/joddd.2021.037. PMID: 35070174. PMCID: PMC8760375.32. Kim YK, Kim JH, Yi YJ, Kwon MJ, Yun PY. 2015; Prospective comparative study of tapered implants with SLA surfaces in the maxillary posterior area according to 3- and 6-month loading time. Int J Periodontics Restorative Dent. 35:271–6. https://doi.org/10.11607/prd.1789. DOI: 10.11607/prd.1789. PMID: 25738348.33. El Chaar E, Puisys A, Sabbag I, Bellón B, Georgantza A, Kye W, et al. 2021; A novel fully tapered, self-cutting tissue-level implant: non-inferiority study in minipigs. Clin Oral Investig. 25:6127–37. https://doi.org/10.1007/s00784-021-03912-w. DOI: 10.1007/s00784-021-03912-w. PMID: 33861379. PMCID: PMC8531107.34. Mustakim KR, Han JJ, Eo MY, Kim SM. 2022; Tapered, sand-blasted, large-grit, and acid-etched surfaced internal dental implant in the diverse pathologic jaw. J Craniofac Surg. 33:2161–8. https://doi.org/10.1097/scs.0000000000008743. DOI: 10.1097/SCS.0000000000008743. PMID: 36089695.35. Mustakim KR, Eo MY, Lee JY, Cho YJ, Seo MH, Kim SM. 2023; Appropriate implant rehabilitation in patients with iatrogenic oroantral fistula and odontogenic maxillary sinusitis. J Craniofac Surg. 34:e92–6. https://doi.org/10.1097/scs.0000000000009099. DOI: 10.1097/SCS.0000000000009099. PMID: 36608090.36. Taheri M, Akbari S, Shamshiri AR, Shayesteh YS. 2020; Marginal bone loss around bone-level and tissue-level implants: a systematic review and meta-analysis. Ann Anat. 231:151525. https://doi.org/10.1016/j.aanat.2020.151525. DOI: 10.1016/j.aanat.2020.151525. PMID: 32380195.37. Vianna TT, Taiete T, Casarin RCV, Giorgi MCC, Aguiar FHB, Silvério KG, et al. 2018; Evaluation of peri-implant marginal tissues around tissue-level and bone-level implants in patients with a history of chronic periodontitis. J Clin Periodontol. 45:1255–65. https://doi.org/10.1111/jcpe.12999. DOI: 10.1111/jcpe.12999. PMID: 30107048.38. Will MJ, Drago C. 2022; Survival rate of ultrawide diameter implants placed into molar postextraction sockets and in function for up to 144 months. J Prosthodont. https://doi.org/10.1111/jopr.13534 [Epub ahead of print]. DOI: 10.1111/jopr.13534. PMID: 35567405.39. Hattingh A, De Bruyn H, Vandeweghe S. 2019; A retrospective study on ultra-wide diameter dental implants for immediate molar replacement. Clin Implant Dent Relat Res. 21:879–87. https://doi.org/10.1111/cid.12759. DOI: 10.1111/cid.12759. PMID: 30938033.40. Hattingh A, Hommez G, De Bruyn H, Huyghe M, Vandeweghe S. 2018; A prospective study on ultra-wide diameter dental implants for immediate molar replacement. Clin Implant Dent Relat Res. 20:1009–15. https://doi.org/10.1111/cid.12666. DOI: 10.1111/cid.12666. PMID: 30255544.41. Chen Y, Yuan S, Zhou N, Man Y. 2017; Transcrestal sinus floor augmentation with immediate implant placement applied in three types of fresh extraction sockets: a clinical prospective study with 1-year follow-up. Clin Implant Dent Relat Res. 19:1034–43. https://doi.org/10.1111/cid.12529. DOI: 10.1111/cid.12529. PMID: 28853203.42. Jensen OT, Brownd C, Baer D. 2006; Maxillary molar sinus floor intrusion at the time of dental extraction. J Oral Maxillofac Surg. 64:1415–9. https://doi.org/10.1016/j.joms.2006.05.027. DOI: 10.1016/j.joms.2006.05.027. PMID: 16916678.43. Ekhlasmandkermani M, Amid R, Kadkhodazadeh M, Hajizadeh F, Abed PF, Kheiri L, et al. 2021; Sinus floor elevation and simultaneous implant placement in fresh extraction sockets: a systematic review of clinical data. J Korean Assoc Oral Maxillofac Surg. 47:411–26. https://doi.org/10.5125/jkaoms.2021.47.6.411. DOI: 10.5125/jkaoms.2021.47.6.411. PMID: 34969014. PMCID: PMC8721410.44. Jensen OT, Shulman LB, Block MS, Iacono VJ. 1998; Report of the sinus consensus conference of 1996. Int J Oral Maxillofac Implants. 13 Suppl:11–45. PMID: 9715571.45. Khehra A, Levin L. 2020; Maxillary sinus augmentation procedures: a narrative clinical review. Quintessence Int. 51:578–84. https://doi.org/10.3290/j.qi.a44632. DOI: 10.3290/j.qi.a44632. PMID: 32500865.46. Nguyen TTH, Eo MY, Cho YJ, Myoung H, Kim SM. 2019; 7-mm-long dental implants: retrospective clinical outcomes in medically compromised patients. J Korean Assoc Oral Maxillofac Surg. 45:260–6. https://doi.org/10.5125/jkaoms.2019.45.5.260. DOI: 10.5125/jkaoms.2019.45.5.260. PMID: 31728333. PMCID: PMC6838352.47. Lemos CA, Ferro-Alves ML, Okamoto R, Mendonça MR, Pellizzer EP. 2016; Short dental implants versus standard dental implants placed in the posterior jaws: a systematic review and meta-analysis. J Dent. 47:8–17. https://doi.org/10.1016/j.jdent.2016.01.005. DOI: 10.1016/j.jdent.2016.01.005. PMID: 26804969.48. Duan XB, Wu TX, Guo YC, Zhou XD, Lei YL, Xu X, et al. 2017; Marginal bone loss around non-submerged implants is associated with salivary microbiome during bone healing. Int J Oral Sci. 9:95–103. https://doi.org/10.1038/ijos.2017.18. DOI: 10.1038/ijos.2017.18. PMID: 28621324. PMCID: PMC5518974.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Implant placement simultaneously sinus augmentation using crestal approach in severely atrophic maxilla; minimally invasive approach
- An analysis of ITI implants placed in korean patients
- Survival rate of Astra Tech implants with maxillary sinus lift
- Delayed Occurrence of Maxillary Sinusitis after Simultaneous Maxillary Sinus Augmentation and Implant: A Case Report and Literature Review
- A lateral approach to the maxillary sinus for simultaneous extraction of an ankylosed maxillary molar and sinus graft: a case report