Korean J Gastroenterol.
2023 Feb;81(2):91-94. 10.4166/kjg.2022.116.
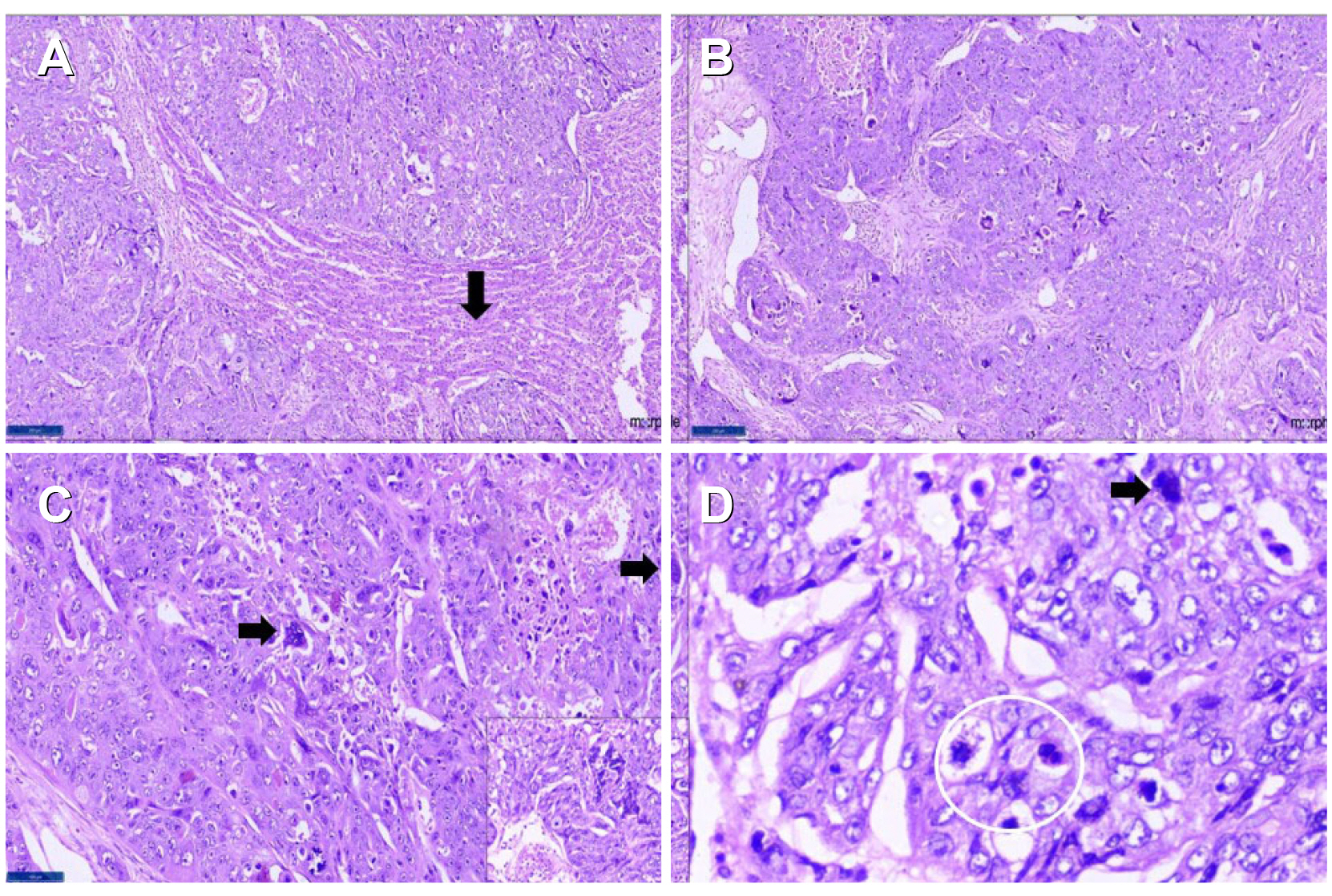
Primary Hepatic Choriocarcinoma with Pregnancy: A Diagnostic and Therapeutic Challenge
- Affiliations
-
- 1Department of Surgical Gastroenterology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India
- 2Department of Surgical Pathology, Nizam’s Institute of Medical Sciences, Hyderabad, Telangana, India
- KMID: 2539578
- DOI: http://doi.org/10.4166/kjg.2022.116
Abstract
- Choriocarcinoma occurs mainly in the gonads, but an extragonadal origin has been reported, albeit infrequently. Primary hepatic choriocarcinoma (PHC) is a rare malignancy, with only 11 cases reported. Most cases reported were in males, with none reported in pregnant females. A 23-year-old primigravida presented with a large liver lesion involving the right lobe of the liver at 28 weeks of pregnancy. Preoperative imaging was suggestive of hepatocellular carcinoma. She underwent a non-anatomical resection of the liver lesion. Surprisingly, her postoperative histopathology revealed a diagnosis of PHC. Her blood workup showed elevated beta human chorionic gonadotrophin. She underwent a termination of her pregnancy at 32 weeks. Before initiating adjuvant chemotherapy four weeks after surgery, a whole-body PET scan revealed multiple bi-lobar liver and pelvic deposits. After a multidisciplinary team discussion, she was started on adjuvant chemotherapy. She is currently under regular follow-up, seven months post-surgery. PHC, one of the vascular lesions of the liver, poses a diagnostic and therapeutic challenge, warranting a multidisciplinary approach.
Keyword
Figure
Reference
-
1. Kohler A, Welsch T, Sturm AK, et al. 2018; Primary choriocarcinoma of the liver: a rare, but important differential diagnosis of liver lesions. J Surg Case Rep. 2018:rjy068. DOI: 10.1093/jscr/rjy110.
Article2. Yousefi Z, Saied S, Davachi B, Rezaei A, Mirzamarjani F. Postmenopausal choriocarcinoma: case report and lliterature review. Int J Cancer Manag. 2017; Mar. 20. doi: 10.5812/ijcm.4400. DOI: 10.5812/ijcm.4400.3. Lee E, Cho H. 2019; A case of intraplacental choriocarcinoma with pulmonary metastasis. Case Rep Oncol. 12:802–806. DOI: 10.1159/000503816. PMID: 31762752. PMCID: PMC6873010.
Article4. Ahn Y, Kim JH, Park CS, Kim TE, Hwang S, Lee SG. 2018; Multidisciplinary approach for treatment of primary hepatic choriocarcinoma in adult male patient. Ann Hepatobiliary Pancreat Surg. 22:164–168. DOI: 10.14701/ahbps.2018.22.2.164. PMID: 29896579. PMCID: PMC5981148.
Article5. Sekine R, Hyodo M, Kojima M, et al. 2013; Primary hepatic choriocarcinoma in a 49-year-old man: report of a case. World J Gastroenterol. 19:9485–9489. DOI: 10.3748/wjg.v19.i48.9485. PMID: 24409080. PMCID: PMC3882426.
Article6. Shi H, Cao D, Wei L, Sun L, Guo A. 2010; Primary choriocarcinoma of the liver: a clinicopathological study of five cases in males. Virchows Arch. 456:65–70. DOI: 10.1007/s00428-009-0864-1. PMID: 20013345.
Article7. Jiang F, Xiang Y, Feng FZ, Ren T, Cui ZM, Wan XR. 2014; Clinical analysis of 13 males with primary choriocarcinoma and review of the literature. Onco Targets Ther. 7:1135–1141. DOI: 10.2147/OTT.S62561. PMID: 25018640. PMCID: PMC4074184.
Article8. Martins VF, Moreno F, Vizcaíno JR, Santos J. 2015; Primary gastric choriocarcinoma: A rare case. Int J Surg Case Rep. 14:44–47. DOI: 10.1016/j.ijscr.2015.07.009. PMID: 26218175. PMCID: PMC4573415.
Article9. Xiong Y, Yang MX. 2019; Primary gastric choriocarcinoma with multiple metastases - A case report and literature review of carcinogenesis. Hum Pathol Case Rep. 18:200330. DOI: 10.1016/j.ehpc.2019.200330.
Article10. Qiu J, Jia S, Li G. 2018; Incidence and prognosis factors of extragonadal choriocarcinoma in males: a population-based study. Cancer Manag Res. 10:4565–4573. DOI: 10.2147/CMAR.S175948. PMID: 30410393. PMCID: PMC6197831.
Article