Ann Surg Treat Res.
2023 Feb;104(2):80-89. 10.4174/astr.2023.104.2.80.
Postoperative major bleeding risk in patients using oral antiplatelets and/or anticoagulants after laparoscopic gastric cancer surgery
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Surgery, Asan Medical Center, Seoul, Korea
- 3Department of Surgery, Kyung Hee University Hospital at Gangdong, Seoul, Korea
- 4Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 5Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2539222
- DOI: http://doi.org/10.4174/astr.2023.104.2.80
Abstract
- Purpose
The use of antiplatelet and/or anticoagulant therapies has become common. In rare cases, these therapies may increase the risk of dangerous postoperative bleeding. We investigated the association of antiplatelets and/or anticoagulants with postoperative major bleeding risk in laparoscopic gastric cancer surgery.
Methods
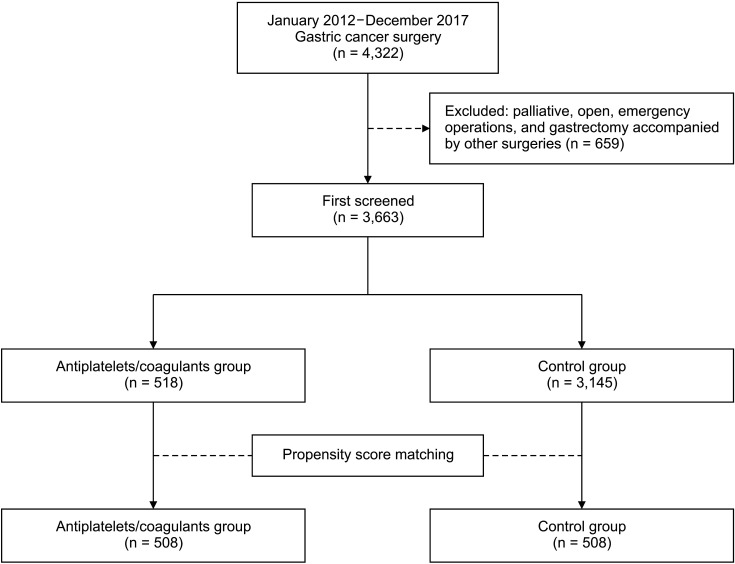
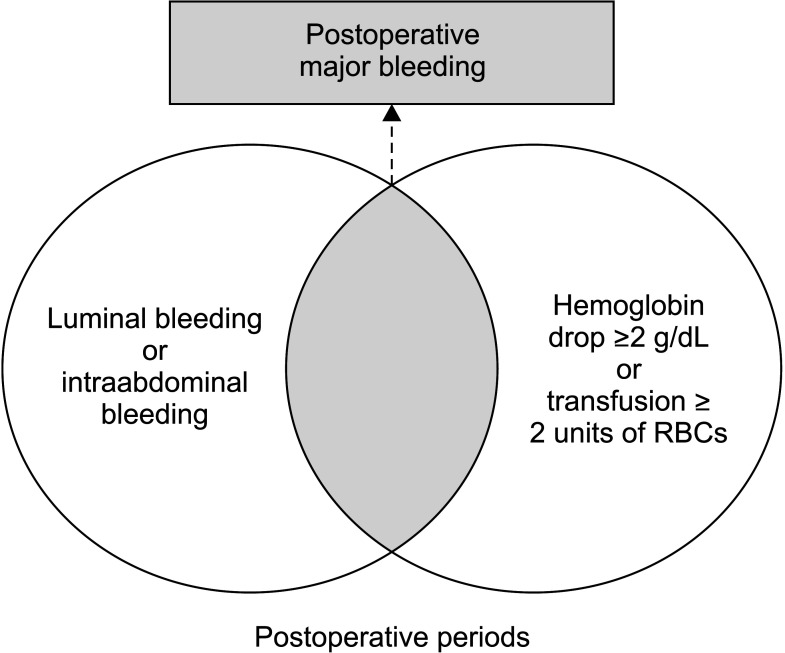
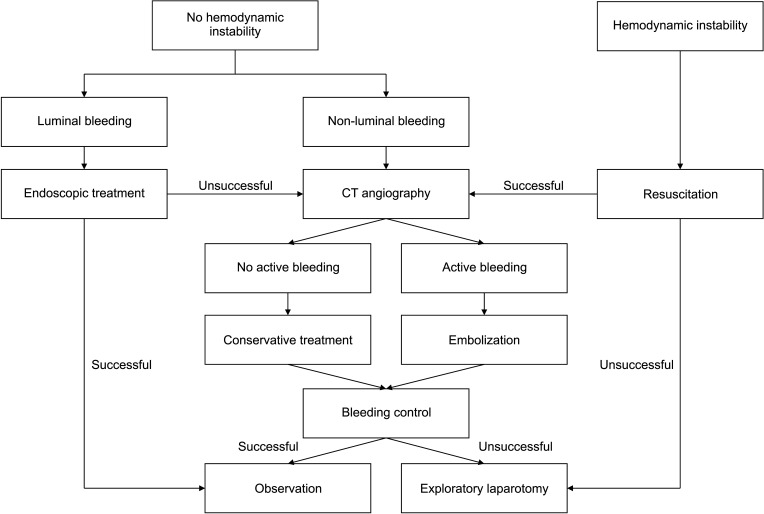
We retrospectively enrolled 3,663 gastric cancer patients (antiplatelet/anticoagulant group, 518; control group, 3,145) who had undergone laparoscopic surgery between January 2012 and December 2017. To minimize selection bias, 508 patients in each group were matched using propensity score matching (PSM) method. The primary outcome was postoperative major bleeding. Secondary outcomes were intraoperative, postoperative transfusion and early complications.
Results
After PSM, postoperative major bleeding occurred in 10 (2.0%) and 3 cases (0.6%) in the antiplatelets/ anticoagulants and control groups, respectively (P = 0.090). Intraoperative and postoperative transfusions were not significantly different between 2 groups (2.4% vs. 1.4%, P = 0.355 and 5.5% vs. 4.3%, P = 0.469). Early complications developed in 58 (11.4%) and 43 patients (8.5%) in the antiplatelets/anticoagulants and control groups, respectively (P = 0.142). The mean amounts of intraoperative and postoperative transfusions were not significantly different between the groups (366.67 ± 238.68 mL vs. 371.43 ± 138.01 mL, P = 0.962; 728.57 ± 642.25 mL vs. 508.09 ± 468.95 mL, P = 0.185). In multivariable analysis, male (P = 0.008) and advanced stage (III, IV) (P = 0.024) were independent significant risk factors for postoperative major bleeding.
Conclusion
Preoperative antiplatelets and/or anticoagulants administration did not significantly increase the risk of postoperative major bleeding after laparoscopic gastric cancer surgery.
Keyword
Figure
Reference
-
1. Oprea AD, Popescu WM. Perioperative management of antiplatelet therapy. Br J Anaesth. 2013; 111 Suppl 1:i3–i17. PMID: 24335397.2. Vandvik PO, Lincoff AM, Gore JM, Gutterman DD, Sonnenberg FA, Alonso-Coello P, et al. Primary and secondary prevention of cardiovascular disease: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012; 141(2 Suppl):e637S–e668S. PMID: 22315274.3. Keeling D, Tait RC, Watson H. British Committee of Standards for Haematology. Peri-operative management of anticoagulation and antiplatelet therapy. Br J Haematol. 2016; 175:602–613. PMID: 27714755.4. Yeung LY, Sarani B, Weinberg JA, McBeth PB, May AK. Surgeon’s guide to anticoagulant and antiplatelet medications part two: antiplatelet agents and perioperative management of long-term anticoagulation. Trauma Surg Acute Care Open. 2016; 1:e000022. PMID: 29767644.5. Schulman S, Angerås U, Bergqvist D, Eriksson B, Lassen MR, Fisher W, et al. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. J Thromb Haemost. 2010; 8:202–204. PMID: 19878532.6. Song W, Yuan Y, Peng J, Chen J, Han F, Cai S, et al. The delayed massive hemorrhage after gastrectomy in patients with gastric cancer: characteristics, management opinions and risk factors. Eur J Surg Oncol. 2014; 40:1299–1306. PMID: 24731269.7. Illuminati G, Ceccanei G, Pacilè MA, Pizzardi G, Palumbo P, Vietri F. Dual antiplatelet treatment in patients candidates for abdominal surgery. Ann Ital Chir. 2013; 84:291–294. PMID: 23103787.8. Fujikawa T, Tanaka A, Abe T, Yoshimoto Y, Tada S, Maekawa H, et al. Does antiplatelet therapy affect outcomes of patients receiving abdominal laparoscopic surgery? Lessons from more than 1,000 laparoscopic operations in a single tertiary referral hospital. J Am Coll Surg. 2013; 217:1044–1053. PMID: 24051069.9. Cui RBJ, Ng KS, Young CJ. Complications arising from perioperative anticoagulant/antiplatelet therapy in major colorectal and abdominal wall surgery. Dis Colon Rectum. 2018; 61:1306–1315. PMID: 30239396.10. Mita K, Ito H, Murabayashi R, Sueyoshi K, Asakawa H, Nabetani M, et al. Postoperative bleeding complications after gastric cancer surgery in patients receiving anticoagulation and/or antiplatelet agents. Ann Surg Oncol. 2012; 19:3745–3752. PMID: 22805868.11. Dindo D, Clavien PA. What is a surgical complication? World J Surg. 2008; 32:939–941. PMID: 18414942.12. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.13. Curnow J, Pasalic L, Favaloro EJ. Why Do Patients Bleed? Surg J (N Y). 2016; 2:e29–e43. PMID: 28824979.14. Woodman RC, Harker LA. Bleeding complications associated with cardiopulmonary bypass. Blood. 1990; 76:1680–1697. PMID: 2224118.15. Bevan DH. Cardiac bypass haemostasis: putting blood through the mill. Br J Haematol. 1999; 104:208–219. PMID: 10050700.16. Penttilä T, Lehto M, Niiranen J, Mehtälä J, Khanfir H, Lassila R, et al. Differences in the risk of stroke, bleeding events, and mortality between female and male patients with atrial fibrillation during warfarin therapy. Eur Heart J Cardiovasc Pharmacother. 2019; 5:29–36. PMID: 30052822.17. Park JY, Kim YW, Eom BW, Yoon HM, Lee JH, Ryu KW, et al. Unique patterns and proper management of postgastrectomy bleeding in patients with gastric cancer. Surgery. 2014; 155:1023–1029. PMID: 24856122.18. Pollei TR, Hinni ML, Moore EJ, Hayden RE, Olsen KD, Casler JD, et al. Analysis of postoperative bleeding and risk factors in transoral surgery of the oropharynx. JAMA Otolaryngol Head Neck Surg. 2013; 139:1212–1218. PMID: 24113922.19. Jeong O, Park YK, Ryu SY, Kim DY, Kim HK, Jeong MR. Predisposing factors and management of postoperative bleeding after radical gastrectomy for gastric carcinoma. Surg Today. 2011; 41:363–368. PMID: 21365417.20. Xie XS, Lin JX, Li P, Xie JW, Wang JB, Lu J, et al. A risk prediction system of postoperative hemorrhage following laparoscopy-assisted radical gastrectomy with D2 lymphadenectomy for primary gastric cancer. Oncotarget. 2017; 8:81511–81519. PMID: 29113410.21. Ng JL, Chan MT, Gelb AW. Perioperative stroke in noncardiac, nonneurosurgical surgery. Anesthesiology. 2011; 115:879–890. PMID: 21862923.22. Bateman BT, Schumacher HC, Wang S, Shaefi S, Berman MF. Perioperative acute ischemic stroke in noncardiac and nonvascular surgery: incidence, risk factors, and outcomes. Anesthesiology. 2009; 110:231–238. PMID: 19194149.23. Smilowitz NR, Gupta N, Ramakrishna H, Guo Y, Berger JS, Bangalore S. Perioperative major adverse cardiovascular and cerebrovascular events associated with noncardiac surgery. JAMA Cardiol. 2017; 2:181–187. PMID: 28030663.24. Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American college of chest physicians evidence-based clinical practice guidelines. Chest. 2012; 141(2 Suppl):e326S–e350S. PMID: 22315266.25. Diamantis T, Tsiminikakis N, Skordylaki A, Samiotaki F, Vernadakis S, Bongiorni C, et al. Alterations of hemostasis after laparoscopic and open surgery. Hematology. 2007; 12:561–570. PMID: 17852431.26. Yasui M, Ikeda M, Miyake M, Ide Y, Okuyama M, Shingai T, et al. Comparison of bleeding risks related to venous thromboembolism prophylaxis in laparoscopic vs open colorectal cancer surgery: a multicenter study in Japanese patients. Am J Surg. 2017; 213:43–49. PMID: 26772140.27. Chi lders CP, Maggard-Gibbons M, Ulloa JG, MacQueen IT, Miake-Lye IM, Shanman R, et al. Perioperative management of antiplatelet therapy in patients undergoing non-cardiac surgery following coronary stent placement: a systematic review. Syst Rev. 2018; 7:4. PMID: 29321066.28. Raval AN, Cigarroa JE, Chung MK, Diaz-Sandoval LJ, Diercks D, Piccini JP, et al. Management of patients on non-vitamin K Antagonist oral anticoagulants in the acute care and periprocedural setting: a scientific statement from the American Heart Association. Circulation. 2017; 135:e604–e633. PMID: 28167634.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prophylactic Antibiotics, Anticoagulants and Antiplatelets for GI Endoscopy
- A Review of the 2018 Asia-Pacific Working Group Consensus on Non-variceal Upper Gastrointestinal Bleeding
- Delayed bleeding after implant surgery in patients taking novel oral anticoagulants: a case report
- Entirely Laparoscopic Gastrectomy and Colectomy for Remnant Gastric Cancer with Gastric Outlet Obstruction and Transverse Colon Invasion
- Continuous Use of Thienopyridine May Be as Safe as Low-Dose Aspirin in Endoscopic Resection of Gastric Tumors