J Stroke.
2023 Jan;25(1):151-159. 10.5853/jos.2022.02215.
Trends in Venous Thromboembolism Readmission Rates after Ischemic Stroke and Intracerebral Hemorrhage
- Affiliations
-
- 1Department of Neurology, Brown University, Providence, RI, USA
- 2Department of Neurology, Yale University, New Haven, CT, USA
- 3Department of Neurology, Weill Cornell Medical Center, New York, NY, USA
- 4Department of Neurology, University of Massachusetts, Worcester, MA, USA
- 5Department of Psychiatry, University of Massachusetts, Worcester, MA, USA
- 6Department of Neurology, Westchester Medical Center, Valhalla, NY, USA
- 7Department of Neurosurgery, Westchester Medical Center, Valhalla, NY, USA
- 8Department of Neurology, New York University, New York, NY, USA
- KMID: 2539068
- DOI: http://doi.org/10.5853/jos.2022.02215
Abstract
- Background and Purpose
Venous thromboembolism (VTE) is a life-threatening complication of stroke. We evaluated nationwide rates and risk factors for hospital readmissions with VTE after an intracerebral hemorrhage (ICH) or acute ischemic stroke (AIS) hospitalization.
Methods
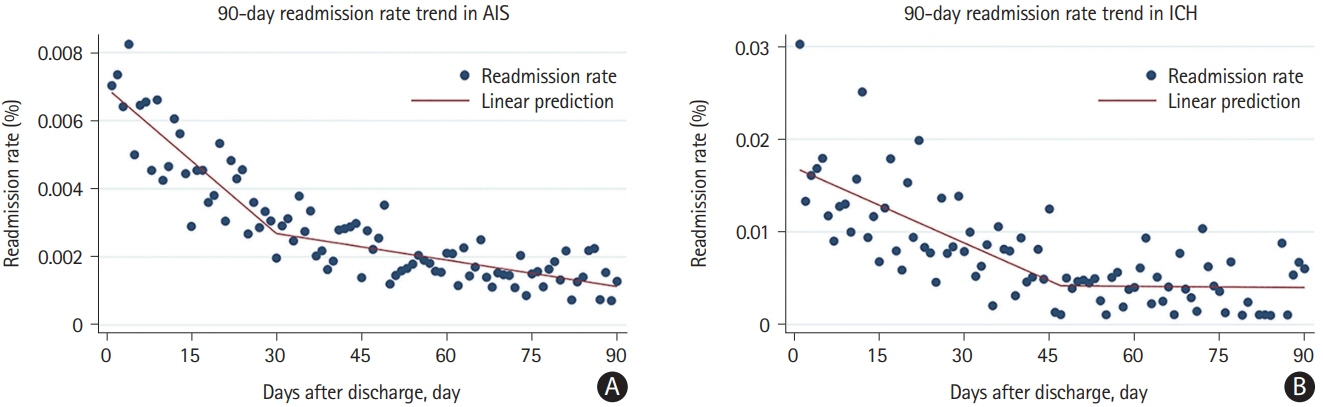
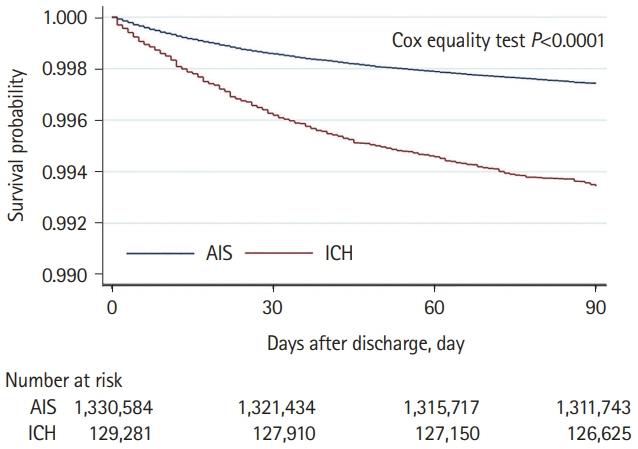
Using the Healthcare Cost and Utilization Project (HCUP) Nationwide Readmission Database, we included patients with a principal discharge diagnosis of ICH or AIS from 2016 to 2019. Patients who had VTE diagnosis or history of VTE during the index admission were excluded. We performed Cox regression models to determine factors associated with VTE readmission, compared rates between AIS and ICH and developed post-stroke VTE risk score. We estimated VTE readmission rates per day over a 90-day time window post-discharge using linear splines.
Results
Of the total 1,459,865 patients with stroke, readmission with VTE as the principal diagnosis within 90 days occurred in 0.26% (3,407/1,330,584) AIS and 0.65% (843/129,281) ICH patients. The rate of VTE readmission decreased within first 4–6 weeks (P<0.001). In AIS, cancer, obesity, higher National Institutes of Health Stroke Scale (NIHSS) score, longer hospital stay, home or rehabilitation disposition, and absence of atrial fibrillation were associated with VTE readmission. In ICH, longer hospital stay and rehabilitation disposition were associated with VTE readmission. The VTE rate was higher in ICH compared to AIS (adjusted hazard ratio 2.86, 95% confidence interval 1.93–4.25, P<0.001).
Conclusions
After stroke, VTE readmission risk is highest within the first 4–6 weeks and nearly three-fold higher after ICH vs. AIS. VTE risk is linked to decreased mobility and hypercoagulability. Studies are needed to test short-term VTE prophylaxis beyond hospitalization in high-risk patients.
Figure
Reference
-
References
1. Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, et al. Heart disease and stroke statistics-2021 update: a report from the American Heart Association. Circulation. 2021; 143:e254–e743.2. Seminog OO, Scarborough P, Wright FL, Rayner M, Goldacre MJ. Determinants of the decline in mortality from acute stroke in England: linked national database study of 795869 adults. BMJ. 2019; 365:l1778.3. Dennis M, Mordi N, Graham C, Sandercock P; CLOTS trials collaboration. The timing, extent, progression and regression of deep vein thrombosis in immobile stroke patients: observational data from the CLOTS multicenter randomized trials. J Thromb Haemost. 2011; 9:2193–2200.4. Viitanen M, Winblad B, Asplund K. Autopsy-verified causes of death after stroke. Acta Med Scand. 1987; 222:401–408.5. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2019; 50:e344–e418.6. Anderson DR, Morgano GP, Bennett C, Dentali F, Francis CW, Garcia DA, et al. American Society of Hematology 2019 guidelines for management of venous thromboembolism: prevention of venous thromboembolism in surgical hospitalized patients. Blood Adv. 2019; 3:3898–3944.7. Hemphill JC 3rd, Greenberg SM, Anderson CS, Becker K, Bendok BR, Cushman M, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a guideline for healthcare professionals from the American Heart Association/ American Stroke Association. Stroke. 2015; 46:2032–2060.8. Hsieh MT, Hsieh CY, Tsai TT, Wang YC, Sung SF. Performance of ICD-10-CM diagnosis codes for identifying acute ischemic stroke in a national health insurance claims database. Clin Epidemiol. 2020; 12:1007–1013.9. Molander V, Bower H, Askling J. Validation and characterization of venous thromboembolism diagnoses in the Swedish National Patient Register among patients with rheumatoid arthritis. Scand J Rheumatol. 2022; Jan. 13. [Epub]. https://doi.org/10.1080/03009742.2021.2001907.10. Dugoff EH, Schuler M, Stuart EA. Generalizing observational study results: applying propensity score methods to complex surveys. Health Serv Res. 2014; 49:284–303.11. Garrido MM, Kelley AS, Paris J, Roza K, Meier DE, Morrison RS, et al. Methods for constructing and assessing propensity scores. Health Serv Res. 2014; 49:1701–1720.12. Kelly J, Rudd A, Lewis R, Hunt BJ. Venous thromboembolism after acute stroke. Stroke. 2001; 32:262–267.13. Noel P, Gregoire F, Capon A, Lehert P. Atrial fibrillation as a risk factor for deep venous thrombosis and pulmonary emboli in stroke patients. Stroke. 1991; 22:760–762.14. Timp JF, Braekkan SK, Versteeg HH, Cannegieter SC. Epidemiology of cancer-associated venous thrombosis. Blood. 2013; 122:1712–1723.15. Caine GJ, Stonelake PS, Lip GY, Kehoe ST. The hypercoagulable state of malignancy: pathogenesis and current debate. Neoplasia. 2002; 4:465–473.16. Stein PD, Beemath A, Meyers FA, Skaf E, Sanchez J, Olson RE. Incidence of venous thromboembolism in patients hospitalized with cancer. Am J Med. 2006; 119:60–68.17. Stein PD, Beemath A, Olson RE. Obesity as a risk factor in venous thromboembolism. Am J Med. 2005; 118:978–980.18. Eichinger S, Hron G, Bialonczyk C, Hirschl M, Minar E, Wagner O, et al. Overweight, obesity, and the risk of recurrent venous thromboembolism. Arch Intern Med. 2008; 168:1678–1683.19. Henke PK, Kahn SR, Pannucci CJ, Secemksy EA, Evans NS, Khorana AA, et al. Call to action to prevent venous thromboembolism in hospitalized patients: a policy statement from the American Heart Association. Circulation. 2020; 141:e914–e931.20. Amin A, Neuman WR, Lingohr-Smith M, Menges B, Lin J. Influence of the duration of hospital length of stay on frequency of prophylaxis and risk for venous thromboembolism among patients hospitalized for acute medical illnesses in the USA. Drugs Context. 2019; 8:212568.21. Silver B, Hamid T, Khan M, Di Napoli M, Behrouz R, Saposnik G, et al. 12 versus 24 h bed rest after acute ischemic stroke thrombolysis: a preliminary experience. J Neurol Sci. 2020; 409:116618.22. Nutescu EA, Spinler SA, Wittkowsky A, Dager WE. Low-molecular-weight heparins in renal impairment and obesity: available evidence and clinical practice recommendations across medical and surgical settings. Ann Pharmacother. 2009; 43:1064–1083.23. Gregory PC, Kuhlemeier KV. Prevalence of venous thromboembolism in acute hemorrhagic and thromboembolic stroke. Am J Phys Med Rehabil. 2003; 82:364–369.24. Prabhakaran S, Herbers P, Khoury J, Adeoye O, Khatri P, Ferioli S, et al. Is prophylactic anticoagulation for deep venous thrombosis common practice after intracerebral hemorrhage? Stroke. 2015; 46:369–375.25. Rinde LB, Småbrekke B, Mathiesen EB, Løchen ML, Njølstad I, Hald EM, et al. Ischemic stroke and risk of venous thromboembolism in the general population: the Tromsø study. J Am Heart Assoc. 2016; 5:e004311.26. Dennis M, Mordi N, Graham C, Sandercock P; CLOTS trials collaboration. The timing, extent, progression and regression of deep vein thrombosis in immobile stroke patients: observational data from the CLOTS multicenter randomized trials. J Thromb Haemost. 2011; 9:2193–2200.27. Subbarao J, Smith J. Pulmonary embolism during stroke rehabilitation. IMJ Ill Med J. 1984; 165:328–332.28. Kahn SR, Lim W, Dunn AS, Cushman M, Dentali F, Akl EA, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012; 141(2 Suppl):e195S–e226S.29. Kamphuisen PW, Agnelli G. What is the optimal pharmacological prophylaxis for the prevention of deep-vein thrombosis and pulmonary embolism in patients with acute ischemic stroke? Thromb Res. 2007; 119:265–274.30. Skaf E, Stein PD, Beemath A, Sanchez J, Bustamante MA, Olson RE. Venous thromboembolism in patients with ischemic and hemorrhagic stroke. Am J Cardiol. 2005; 96:1731–1733.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cerebrovascular Disease : Overview and Classification
- CADASIL with Intracerebral Hemorrhage after Acute Ischemic Stroke
- Warfarin-Induced Intracerebral Hemorrhage Associated with Microbleeds
- A Clinical Analysis of Cerebrovascular Disease in YUH
- The Comparative Analysis of the Carotid Intima-Media Thickness and Homocysteine Level between Ischemic Stroke and Hypertensive Intracerebral Hemorrhage