J Stroke.
2023 Jan;25(1):141-150. 10.5853/jos.2022.02012.
Explanatory Power and Prognostic Implications of Factors Associated with Troponin Elevation in Acute Ischemic Stroke
- Affiliations
-
- 1Department of Neurology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Busan, Korea
- 2Clinical Research Center, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Division of Biostatistics, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Busan, Korea
- 4Department of Neurology, Asan Medical Center, University of Ulsan, College of Medicine, Seoul, Korea
- 5Division of Cardiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 6Division of Cardiology, Research Institute for Convergence of Biomedical Science and Technology, Pusan National University Yangsan Hospital, Pusan National University School of Medicine, Busan, Korea
- 7Department of Neurology, Gangneung Asan Hospital, University of Ulsan, Gangneung, Korea
- KMID: 2539067
- DOI: http://doi.org/10.5853/jos.2022.02012
Abstract
- Background and Purpose
We investigated the impact of comorbidity burden on troponin elevation, with separate consideration of neurological conditions, in patients with acute ischemic stroke (AIS).
Methods
This prospective, observational cohort study consecutively enrolled patients with AIS for 2 years. Serum cardiac troponin I was repeatedly measured, and disease-related biomarkers were collected for diagnosis of preassigned comorbidities, including atrial fibrillation (AF), ischemic heart disease (IHD), myocardial hypertrophy (MH), heart failure (HF), renal insufficiency (RI), and active cancer. The severity of neurological deficits and insular cortical ischemic lesions were assessed as neurological conditions. Adjusted associations between these factors and troponin elevation were determined using a multivariate ordinal logistic regression model and area under the receiver operating characteristic curve (AUC). Cox proportional hazards model was used to determine the prognostic significance of comorbidity beyond neurological conditions.
Results
Among 1,092 patients (66.5±12.4 years, 63.3% male), 145 (13.3%) and 335 (30.7%) had elevated (≥0.040 ng/mL) and minimally-elevated (0.040–0.010 ng/mL) troponin, respectively. In the adjusted analysis, AF, MH, HF, RI, active cancer, and neurological deficits were associated with troponin elevation. The multivariate model with six comorbidities and two neurological conditions exhibited an AUC of 0.729 (95% confidence interval [CI], 0.698–0.759). In Cox regression, AF, IHD, and HF were associated with adverse cardio-cerebrovascular events, whereas HF and active cancer were associated with mortality.
Conclusion
Troponin elevation in patients with AIS can be explained by the burden of comorbidities in combination with neurological status, which explains the prognostic significance of troponin assay.
Keyword
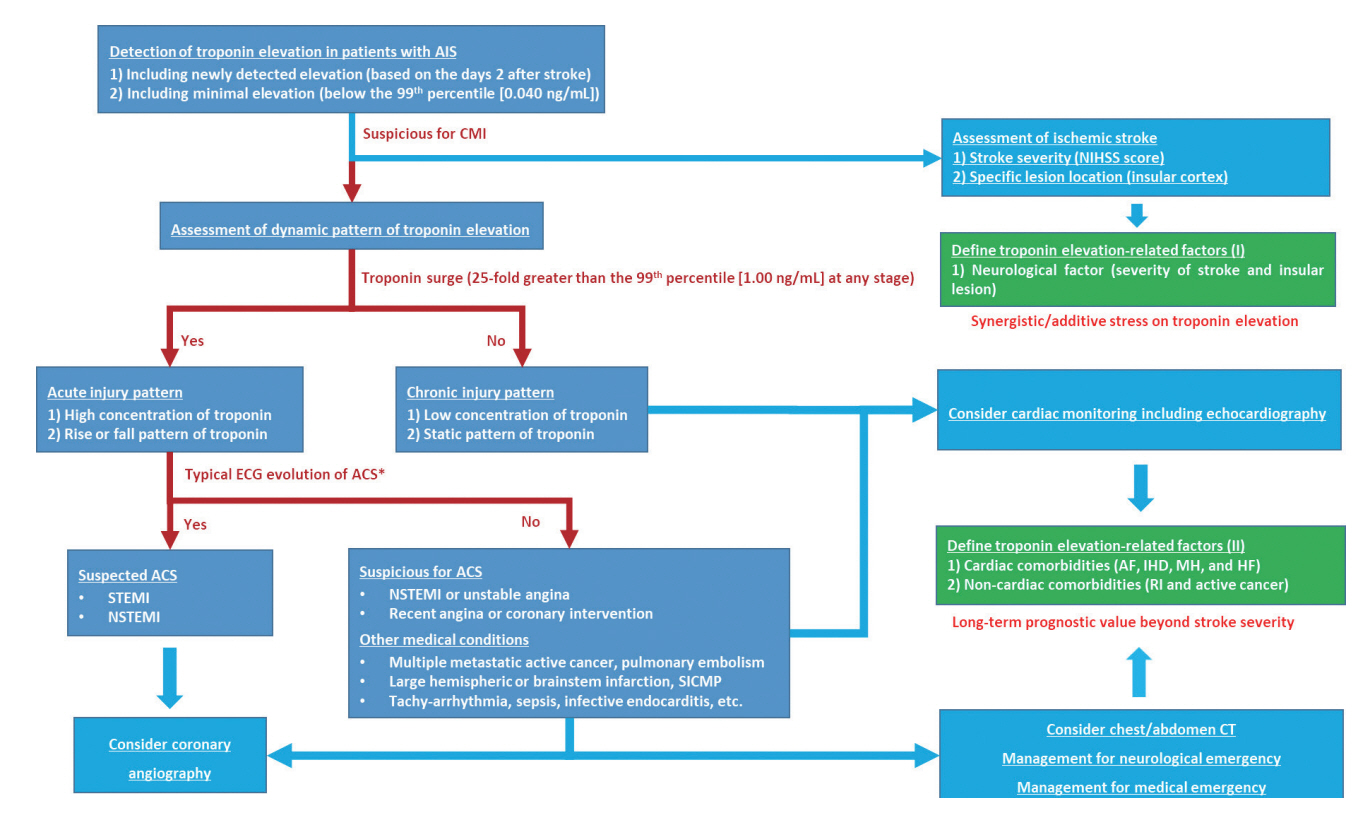
Figure
Reference
-
References
1. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018; 72:2231–2264.2. Eggers KM, Jernberg T, Lindahl B. Cardiac troponin elevation in patients without a specific diagnosis. J Am Coll Cardiol. 2019; 73:1–9.3. Twerenbold R, Jaffe A, Reichlin T, Reiter M, Mueller C. High-sensitive troponin T measurements: what do we gain and what are the challenges? Eur Heart J. 2012; 33:579–586.4. Balch MHH, Nimjee SM, Rink C, Hannawi Y. Beyond the brain: the systemic pathophysiological response to acute ischemic stroke. J Stroke. 2020; 22:159–172.5. Newby LK, Jesse RL, Babb JD, Christenson RH, De Fer TM, Diamond GA, et al. ACCF 2012 expert consensus document on practical clinical considerations in the interpretation of troponin elevations: a report of the American College of Cardiology Foundation task force on clinical expert consensus documents. J Am Coll Cardiol. 2012; 60:2427–2463.6. Kerr G, Ray G, Wu O, Stott DJ, Langhorne P. Elevated troponin after stroke: a systematic review. Cerebrovasc Dis. 2009; 28:220–226.7. Powers WJ, Rabinstein AA, Ackerson T, Adeoye OM, Bambakidis NC, Becker K, et al. 2018 guidelines for the early management of patients with acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2018; 49:e46–e110.8. Ahn SH, Kim YH, Lee JS, Han JH, Kim SY, Kang DW, et al. Troponin I levels and long-term outcomes in acute ischemic stroke patients. J Am Coll Cardiol. 2019; 73:525–526.9. Ahn SH, Lee JS, Kim YH, Kim BJ, Kim YJ, Kang DW, et al. Prognostic significance of troponin elevation for long-term mortality after ischemic stroke. J Stroke. 2017; 19:312–322.10. Ahn SH, Kim YH, Shin CH, Lee JS, Kim BJ, Kim YJ, et al. Cardiac vulnerability to cerebrogenic stress as a possible cause of troponin elevation in stroke. J Am Heart Assoc. 2016; 5:e004135.11. Thygesen K, Mair J, Mueller C, Huber K, Weber M, Plebani M, et al. Recommendations for the use of natriuretic peptides in acute cardiac care: a position statement from the study group on biomarkers in cardiology of the ESC working group on acute cardiac care. Eur Heart J. 2012; 33:2001–2006.12. Seok JM, Kim SG, Kim JW, Chung CS, Kim GM, Lee KH, et al. Coagulopathy and embolic signal in cancer patients with ischemic stroke. Ann Neurol. 2010; 68:213–219.13. Adams HP Jr, Davis PH, Leira EC, Chang KC, Bendixen BH, Clarke WR, et al. Baseline NIH stroke scale score strongly predicts outcome after stroke: a report of the Trial of Org 10172 in Acute Stroke Treatment (TOAST). Neurology. 1999; 53:126–131.14. Palma JA, Benarroch EE. Neural control of the heart: recent concepts and clinical correlations. Neurology. 2014; 83:261–271.15. Hijazi Z, Oldgren J, Andersson U, Connolly SJ, Ezekowitz MD, Hohnloser SH, et al. Cardiac biomarkers are associated with an increased risk of stroke and death in patients with atrial fibrillation: a randomized evaluation of long-term anticoagulation therapy (RE-LY) substudy. Circulation. 2012; 125:1605–1616.16. van den Bos EJ, Constantinescu AA, van Domburg RT, Akin S, Jordaens LJ, Kofflard MJ. Minor elevations in troponin I are associated with mortality and adverse cardiac events in patients with atrial fibrillation. Eur Heart J. 2011; 32:611–617.17. Cikes M, Solomon SD. Beyond ejection fraction: an integrative approach for assessment of cardiac structure and function in heart failure. Eur Heart J. 2016; 37:1642–1650.18. Ducrocq G, Amarenco P, Labreuche J, Alberts MJ, Mas JL, Ohman EM, et al. A history of stroke/transient ischemic attack indicates high risks of cardiovascular event and hemorrhagic stroke in patients with coronary artery disease. Circulation. 2013; 127:730–738.19. Chin CW, Shah AS, McAllister DA, Joanna Cowell S, Alam S, Langrish JP, et al. High-sensitivity troponin I concentrations are a marker of an advanced hypertrophic response and adverse outcomes in patients with aortic stenosis. Eur Heart J. 2014; 35:2312–2321.20. Turakhia MP, Blankestijn PJ, Carrero JJ, Clase CM, Deo R, Herzog CA, et al. Chronic kidney disease and arrhythmias: conclusions from a kidney disease: improving global outcomes (KDIGO) controversies conference. Eur Heart J. 2018; 39:2314–2325.21. Zimetbaum PJ, Josephson ME. Use of the electrocardiogram in acute myocardial infarction. N Engl J Med. 2003; 348:933–940.22. Adams RJ, Chimowitz MI, Alpert JS, Awad IA, Cerqueria MD, Fayad P, et al. Coronary risk evaluation in patients with transient ischemic attack and ischemic stroke: a scientific statement for healthcare professionals from the Stroke Council and the Council on Clinical Cardiology of the American Heart Association/American Stroke Association. Circulation. 2003; 108:1278–1290.23. Mochmann HC, Scheitz JF, Petzold GC, Haeusler KG, Audebert HJ, Laufs U, et al. Coronary angiographic findings in acute ischemic stroke patients with elevated cardiac troponin. The troponin elevation in acute ischemic stroke (TRELAS) study. Circulation. 2016; 133:1264–1271.24. Maisel A, Mueller C, Adams K Jr, Anker SD, Aspromonte N, Cleland JG, et al. State of the art: using natriuretic peptide levels in clinical practice. Eur J Heart Fail. 2008; 10:824–839.25. Bacharova L, Schocken D, Estes EH, Strauss D. The role of ECG in the diagnosis of left ventricular hypertrophy. Curr Cardiol Rev. 2014; 10:257–261.26. Galderisi M, Cosyns B, Edvardsen T, Cardim N, Delgado V, Di Salvo G, et al. Standardization of adult transthoracic echocardiography reporting in agreement with recent chamber quantification, diastolic function, and heart valve disease recommendations: an expert consensus document of the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2017; 18:1301–1310.27. DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988; 44:837–845.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prognostic Implications of Elevated Cardiac Troponin T in Patients with Acute Ischemic Stroke
- Prognostic Significance of Troponin Elevation for Long-Term Mortality after Ischemic Stroke
- Cardiac Troponin T Elevation After Stroke: Relationships Between Elevated Serum Troponin T, Stroke Location, and Prognosis
- The Usefulness of Cardiac Biomarker in Patients with Acute Ischemic Stroke
- Acute Coronary Syndrome