Clin Endosc.
2023 Jan;56(1):65-74. 10.5946/ce.2021.119.
Endoscopic ultrasound-guided coiling and glue is safe and superior to endoscopic glue injection in gastric varices with severe liver disease: a retrospective case control study
- Affiliations
-
- 1Department of Gastroenterology, Artemis Hospitals, Gurugram, India
- 2Institute of Liver and Biliary Sciences, New Delhi, India
- KMID: 2538753
- DOI: http://doi.org/10.5946/ce.2021.119
Abstract
- Background/Aims
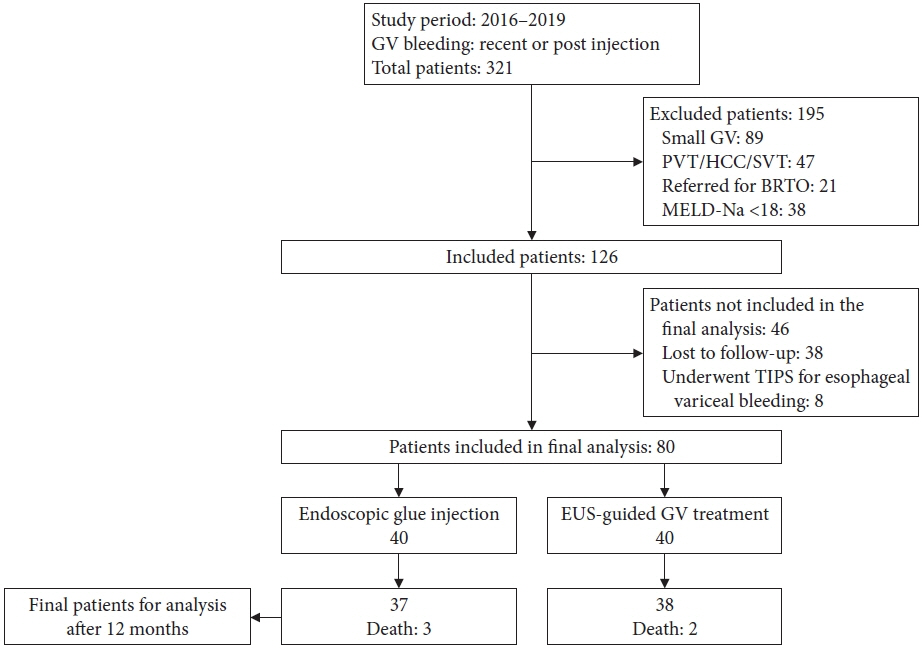
Gastric varices (GV) are present in 25% of cirrhotic patients with high rates of rebleeding and mortality. Data on endoscopic ultrasound (EUS)-guided treatment in severe liver disease (model for end stage liver disease sodium [MELD-Na] >18 and Child-Turcotte-Pugh [CTP] C with GV) are scarce. Thus, we performed a retrospective comparison of endoscopic glue injection with EUS-guided therapy in cirrhotic patients with large GV.
Methods
A retrospective study was performed in the tertiary hospitals of India. A total of 80 patients were recruited. The inclusion criteria were gastroesophageal varices type 2, isolated gastric varices type 1, bleeding within 6 weeks, size of GV >10 mm, and a MELD-Na >18. Treatment outcomes and complications of endoscopic glue injection and EUS-guided GV therapy were compared.
Results
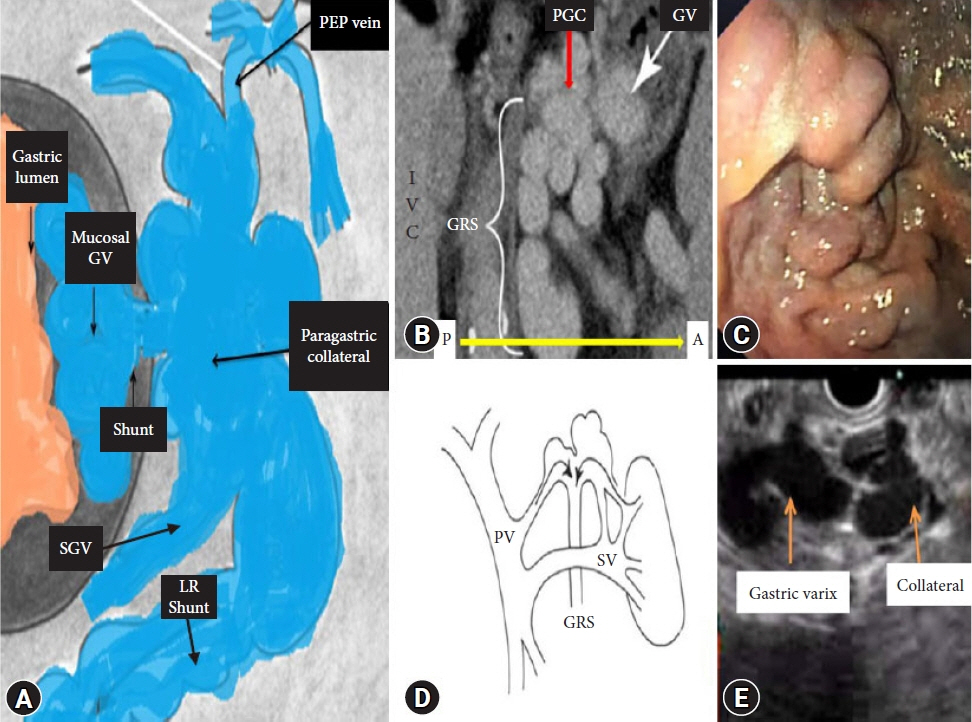
In this study, the patients’ age, sex, liver disease severity (CTP, MELD-Na) and clinical parameters were comparable. The median number of procedures, injected glue volume, complications, and GV obturation were better in the EUS group, respectively. On subgroup analysis of the EUS method (e.g., direct gastric fundus vs. paragastric collateral [PGC] coil placement), PGC coil placement showed decreased coil requirement, less injected glue volume, decreased luminal coil extrusion, and increased successful GV obturation.
Conclusions
EUS-guided treatment is more efficient and safer, and requires a smaller number of treatment sessions, as compared to endoscopic treatment in severe liver disease patients with large GV. Furthermore, PGC coil placement increases the complete obliteration of GV.
Figure
Reference
-
1. Sarin SK, Lahoti D, Saxena SP, et al. Prevalence, classification and natural history of gastric varices: a long-term follow-up study in 568 portal hypertension patients. Hepatology. 1992; 16:1343–1349.2. Kim T, Shijo H, Kokawa H, et al. Risk factors for hemorrhage from gastric fundal varices. Hepatology. 1997; 25:307–312.3. Pereira P, Peixoto A. Left-sided portal hypertension: a clinical challenge. GE Port J Gastroenterol. 2015; 22:231–233.4. Jamwal K, Padhan RK, Sharma A. Refractory variceal bleeding: approach to management (mini review). World J Gastroenterol Hepatol Endosc. 2020; 3:1–3.5. Lahoti S, Catalano MF, Alcocer E, et al. Obliteration of esophageal varices using EUS-guided sclerotherapy with color Doppler. Gastrointest Endosc. 2000; 51:331–333.6. Trudeau W, Prindiville T. Endoscopic injection sclerosis in bleeding gastric varices. Gastrointest Endosc. 1986; 32:264–268.7. Sarin SK, Kumar A. Endoscopic treatment of gastric varices. Clin Liver Dis. 2014; 18:809–827.8. Henry Z, Uppal D, Saad W, et al. Gastric and ectopic varices. Clin Liver Dis. 2014; 18:371–388.9. Weilert F, Binmoeller KF. EUS-guided vascular access and therapy. Gastrointest Endosc Clin N Am. 2012; 22:303–314.10. Saraswat VA, Verma A. Gluing gastric varices in 2012: lessons learnt over 25 years. J Clin Exp Hepatol. 2012; 2:55–69.11. Watanabe K, Kimura K, Matsutani S, et al. Portal hemodynamics in patients with gastric varices. A study in 230 patients with esophageal and/or gastric varices using portal vein catheterization. Gastroenterology. 1988; 95:434–440.12. Mishra SR, Sharma BC, Kumar A, et al. Primary prophylaxis of gastric variceal bleeding comparing cyanoacrylate injection and beta-blockers: a randomized controlled trial. J Hepatol. 2011; 54:1161–1167.13. Weilert F, Binmoeller KF. New endoscopic technologies and procedural advances for endoscopic hemostasis. Clin Gastroenterol Hepatol. 2016; 14:1234–1244.14. McCarty TR, Bazarbashi AN, Hathorn KE, et al. Combination therapy versus monotherapy for EUS-guided management of gastric varices: a systematic review and meta-analysis. Endosc Ultrasound. 2020; 9:6–15.15. Robles-Medranda C, Oleas R, Valero M, et al. Endoscopic ultrasonography-guided deployment of embolization coils and cyanoacrylate injection in gastric varices versus coiling alone: a randomized trial. Endoscopy. 2020; 52:268–275.16. Lôbo MR de A, Chaves DM, DE Moura DTH, et al. Safety and efficacy of EUS-guided coil plus cyanoacrylate versus conventional cyanoacrylate technique in the treatment of gastric varices: a randomized controlled trial. Arq Gastroenterol. 2019; 56:99–105.17. Mohan BP, Chandan S, Khan SR, et al. Efficacy and safety of endoscopic ultrasound-guided therapy versus direct endoscopic glue injection therapy for gastric varices: systematic review and meta-analysis. Endoscopy. 2020; 52:259–267.18. Romero-Castro R, Ellrichmann M, Ortiz-Moyano C, et al. EUS-guided coil versus cyanoacrylate therapy for the treatment of gastric varices: a multicenter study (with videos). Gastrointest Endosc. 2013; 78:711–721.19. Bhat YM, Weilert F, Fredrick RT, et al. EUS-guided treatment of gastric fundal varices with combined injection of coils and cyanoacrylate glue: a large U.S. experience over 6 years (with video). Gastrointest Endosc. 2016; 83:1164–1172.20. Iwase H, Suga S, Morise K, et al. Color Doppler endoscopic ultrasonography for the evaluation of gastric varices and endoscopic obliteration with cyanoacrylate glue. Gastrointest Endosc. 1995; 41:150–154.21. Romero-Castro R, Pellicer-Bautista FJ, Jimenez-Saenz M, et al. EUS-guided injection of cyanoacrylate in perforating feeding veins in gastric varices: results in 5 cases. Gastrointest Endosc. 2007; 66:402–407.22. Kakutani H, Hino S, Ikeda K, et al. Use of the curved linear-array echo endoscope to identify gastrorenal shunts in patients with gastric fundal varices. Endoscopy. 2004; 36:710–714.23. Bick BL, Al-Haddad M, Liangpunsakul S, et al. EUS-guided fine needle injection is superior to direct endoscopic injection of 2-octyl cyanoacrylate for the treatment of gastric variceal bleeding. Surg Endosc. 2019; 33:1837–1845.24. Jamwal K, Sharma M, Sarin S, et al. A comparitive analysis of endoscopic management of gastric varices: is EUS guided treatment safe, more efficacious and cost effective as compared to standard treatment in advanced liver disease? J Gastroenterol Hepatol. 2019; 34(Suppl 3):72.25. Jamwal K, Sharma A, Padhan R, et al. EUS in management of gastric varices: targeting paraesophageal collateral is safe and better in severe liver disease as compared to gastric varices itself. Gastroenterology. 2020; 158(Suppl 1):S–1478.26. Fujii-Lau LL, Law R, Wong Kee Song LM, et al. Endoscopic ultrasound (EUS)-guided coil injection therapy of esophagogastric and ectopic varices. Surg Endosc. 2016; 30:1396–1404.27. Jamwal K. Gastric varices treatment: is it possible to individualise therapy for bleeding patients. World J Gastroenterol Hepatol Endosc. 2021; 3:1–2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Ultrasound-Guided Vascular Therapy: The Present and the Future
- The Influence of EIS or EVL to Gastric Varices in Bleeding Esophageal Varices
- Practical Approach to Endoscopic Management for Bleeding Gastric Varices
- Usefulness of Endoscopic Ultrasound in Esophagogastric Varices
- Endoscopic ultrasound-guided vascular intervention for portal hypertension