Pediatr Emerg Med J.
2022 Dec;9(2):95-102. 10.22470/pemj.2022.00507.
Epidemiologic features according to age groups of pediatric dental injury in emergency departments
- Affiliations
-
- 1Department of Emergency Medicine, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Republic of Korea
- 2Department of Traumatology, Gachon University Gil Medical Center, Gachon University College of Medicine, Incheon, Republic of Korea
- KMID: 2538070
- DOI: http://doi.org/10.22470/pemj.2022.00507
Abstract
- Purpose
The aim of this study was to investigate the epidemiologic features of pediatric dental injury according to age groups using Korean national data.
Methods
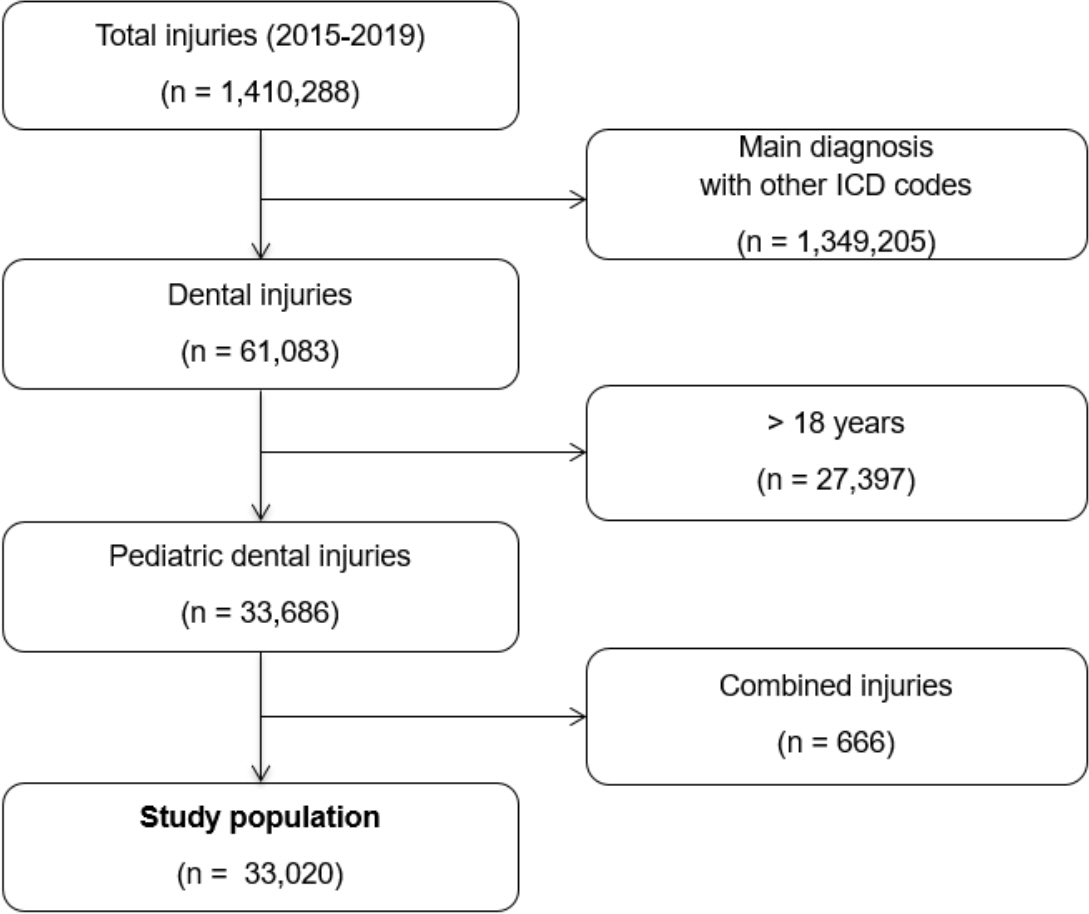
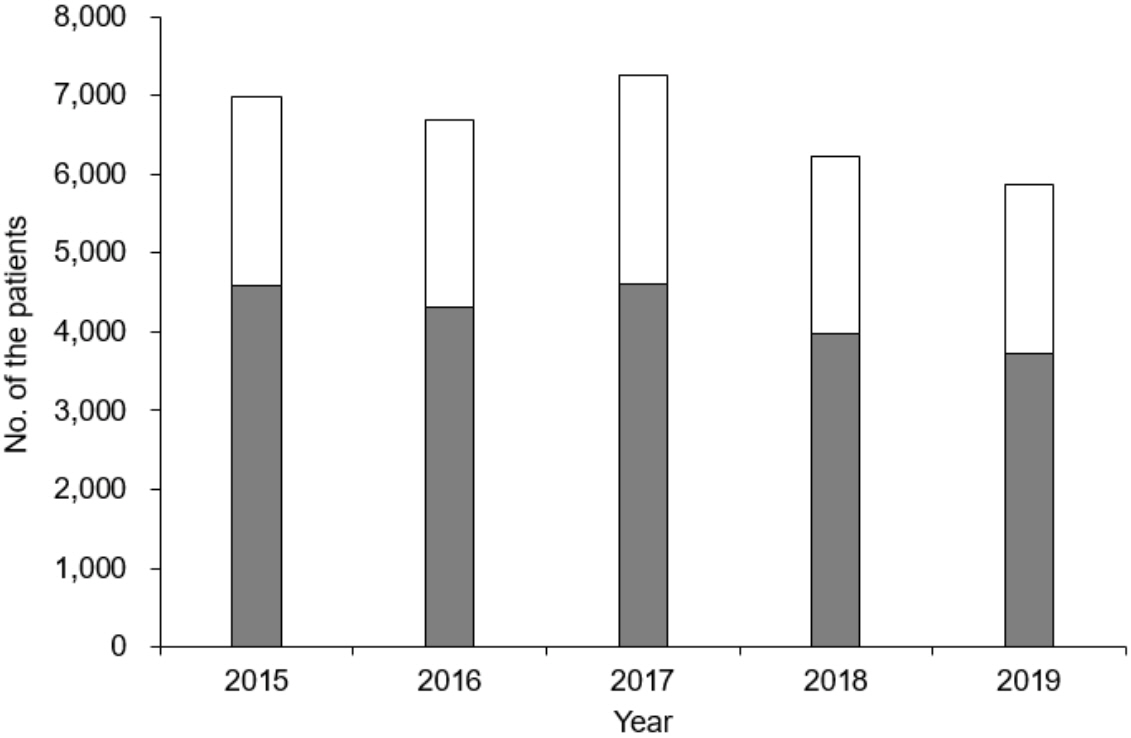
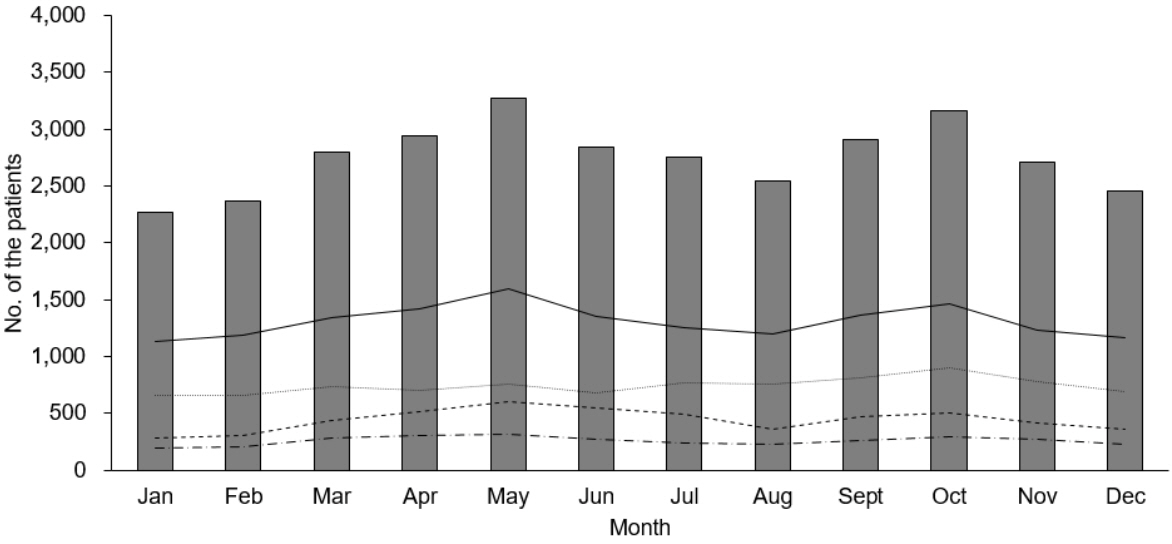
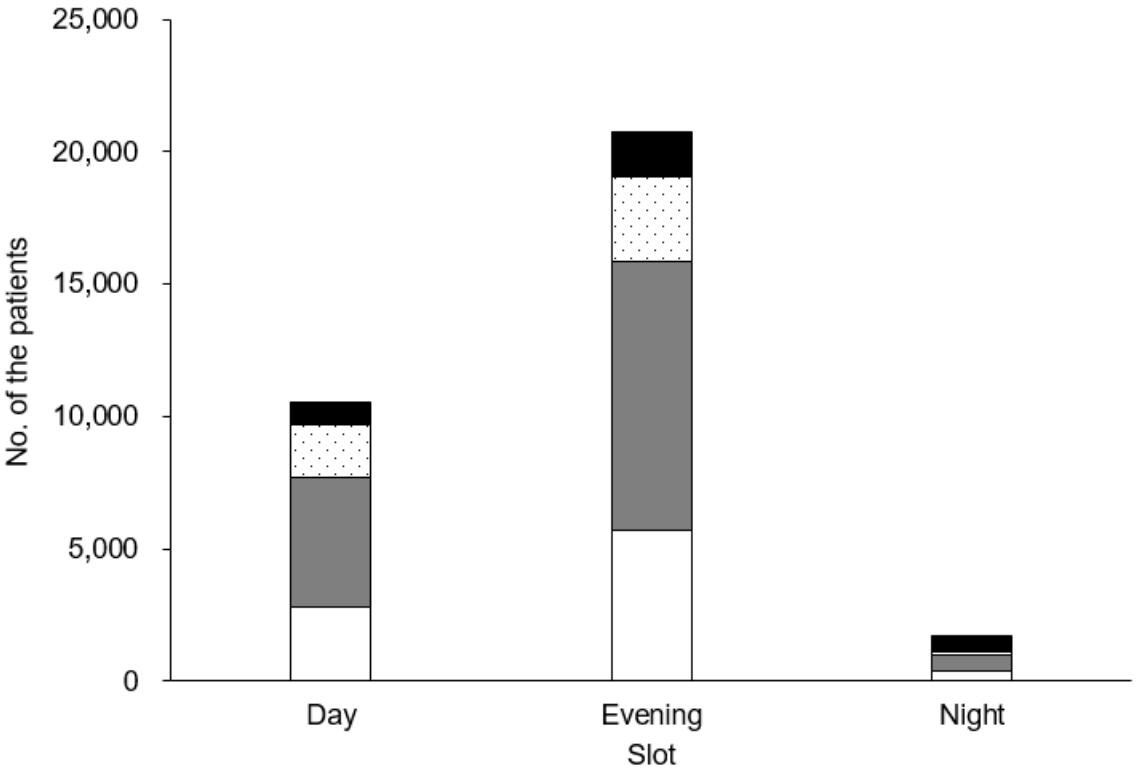
We reviewed the data from 2015 to 2019 Emergency Department-based Injury In-depth Surveillance registry, which involves 23 emergency departments in Korea. We included children aged 18 years or younger with the International Classification of Disease, 10th Revision codes related to dental injury. Other or combined codes were excluded. The children were classified by age groups: infants (< 1 year), preschoolers (2-6), schoolers (7-12), and adolescents (13-18). As per the age groups, we compared the clinical characteristics, injury event profiles, and outcomes.
Results
The study population (n = 33,020) consisted of 8,900 infants (27.0%), 15,705 preschoolers (47.6%), 5,295 schoolers (16.0%), and 3,120 adolescents (9.4%). Their median age was 3 years (interquartile range, 1-7), and boys accounted for 64.2%. The most common mechanism, type of activity, and place were slip down (14,274 [43.2%]), daily activity (23,777 [72.0%]), and home (19,980 [60.5%]), respectively. Among the injury types, soft tissue injury was most common (24,357 [73.8%]). As for the outcomes, 32,841 (99.5%) children were discharged, and 332 (1.0%) children had severe injury. As the age increased, the frequencies changed as follows. As for the place and type, household injury and soft tissue injury decreased while outdoor injury, such as road traffic injury, and tooth fracture increased (P < 0.001). As for the type of activity, injuries related to exercise/sports and education increased (P < 0.001). Of the sports activity, ball sports increased while kickboard/cycle decreased (P < 0.001).
Conclusion
Using the epidemiologic features of pediatric dental injury, it is advisable to establish injury prevention strategies according to the age groups.
Figure
Reference
-
References
1. Kiyak HA. Does orthodontic treatment affect patients’ quality of life? J Dent Educ. 2008; 72:886–94.2. Tin-Oo MM, Saddki N, Hassan N. Factors influencing patient satisfaction with dental appearance and treatments they desire to improve aesthetics. BMC Oral Health. 2011; 11:6.3. Andersson L. Epidemiology of traumatic dental injuries. J Endod. 2013; 39(3 Suppl):S2–5.4. Osunde OD, Amole IO, Ver-or N, Akhiwu BI, Adebola RA, Iyogun CA, et al. Pediatric maxillofacial injuries at a Nigerian teaching hospital: a three-year review. Niger J Clin Pract. 2013; 16:149–54.5. Flores MT, Andersson L, Andreasen JO, Bakland LK, Malmgren B, Barnett F, et al. Guidelines for the management of traumatic dental injuries. II. Avulsion of permanent teeth. Dent Traumatol. 2007; 23:130–6.6. Levin L, Day PF, Hicks L, O’Connell A, Fouad AF, Bourguignon C, et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: general introduction. Dent Traumatol. 2020; 36:309–13.7. James V, Vandersluis YR, Zhang EW, Scolnik D. Dental injuries in younger emergency department patients. CJEM. 2018; 20:425–31.8. Antunes LA, Lemos HM, Milani AJ, Guimarães LS, Kuchler EC, Antunes LS. Does traumatic dental injury impact oral health-related to quality of life of children and adolescents? Systematic review and meta-analysis. Int J Dent Hyg. 2020; 18:142–62.9. Park KH, Song JM, Hwang DS, Kim YD, Shin SH, Kim UK, et al. A clinical study of emergency room visits for oral and maxillofacial lacerations. J Korean Assoc Oral Maxillofac Surg. 2015; 41:246–50.10. Kim C, Choi E, Park KM, Kwak EJ, Huh J, Park W. Characteristics of patients who visit the dental emergency room in a dental college hospital. J Dent Anesth Pain Med. 2019; 19:21–7.11. Kang BS, Jang SB, Im TH, Bae SM. Tooth injuries in the emergency department. J Korean Soc Emerg Med. 2002; 13:250–5. Korean.12. Jang CS, Lee CY, Kim JW, Yim JH, Kim JY, Kim YH, et al. A clinical study on the dental emergency patients visiting an university hospital emergency room. J Korean Assoc Oral Maxillofac Surg. 2011; 37:439–47. Korean.13. Bae DH, Kim JH. Retrospective study of traumatic dental injuries among children aged 0-15 years in Wonju. J Korean Acad Pediatr Dent. 2017; 44:64–71. Korean.14. Korea Disease Control and Prevention Agency (KDCA). Emergency Department-based Injury In-depth Surveillance guidebook [Internet]. Cheongju (Korea): KDCA;2022. [cited 2021 May 27]. Available from: http://www.kdca.go.kr/injury/biz/injury/recsroom/examinGudbkMain.do. Korean.15. Kim J, Shin SD, Im TH, Lee KJ, Ko SB, Park JO, et al. Development and validation of the excess mortality ratio-adjusted Injury Severity Score using the International Classification of Diseases 10th Edition. Acad Emerg Med. 2009; 16:454–64.16. Yang RT, Li Z, Li ZB. Maxillofacial injuries in infants and preschools: a 2.5-year study. J Craniofac Surg. 2014; 25:964–7.17. Ahn KA, Kim ES, Lim KS. Age-related injury profile in childhood. J Korean Soc Trauma. 2009; 22:87–96. Korean.18. Keum KC, Paeng JY, Choi BY, Choi JG, Oh SR, Lee J, et al. An clinical analysis on the dental emergency patients visiting the emergency room of Dental Hospital of Won-kwang University. J Korean Assoc Maxillofac Plast Reconstr Surg. 2009; 31:35–40. Korean.19. Matsumura T, Ohshige K, Tsuchida K, Mizushima S, Tochikubo O. The increasing use of pediatric emergency facilities in the evening. Pediatr Emerg Care. 2007; 23:142–7.20. Lam R. Epidemiology and outcomes of traumatic dental injuries: a review of the literature. Aust Dent J. 2016; 61 Suppl 1:4–20.21. Kotecha S, Scannell J, Monaghan A, Williams RW. A four year retrospective study of 1,062 patients presenting with maxillofacial emergencies at a specialist paediatric hospital. Br J Oral Maxillofac Surg. 2008; 46:293–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiologic features of pediatric genital injury in emergency departments in Korea
- Epidemiologic characteristics of children who visited an emergency department: a single center study over three years
- National Patterns and Characteristics in Pediatric Dental Emergency Visits for Dental Conditions
- Management of abdominal pain in pediatric emergency departments
- Difference in the epidemiologic and clinical characteristics by age groups of the children who visited a hand center emergency department with a hand injury requiring surgery