Ann Surg Treat Res.
2023 Jan;104(1):43-50. 10.4174/astr.2023.104.1.43.
Clinical significance of acute care surgery system as a part of hospital medical emergency team for hospitalized patients
- Affiliations
-
- 1Division of Critical Care, Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 2Sungkyunkwan University Graduate School of Medicine, Suwon, Korea
- 3Division of Acute Care Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Critical Care Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2537629
- DOI: http://doi.org/10.4174/astr.2023.104.1.43
Abstract
- Purpose
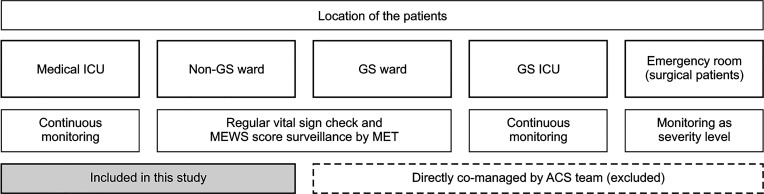
Acute care surgery (ACS) has been practiced in several tertiary hospitals in South Korea since the late 2000s. The medical emergency team (MET) has improved the management of patients with clinical deterioration during hospitalization. This study aimed to identify the clinical effectiveness of collaboration between ACS and MET in hospitalized patients.
Methods
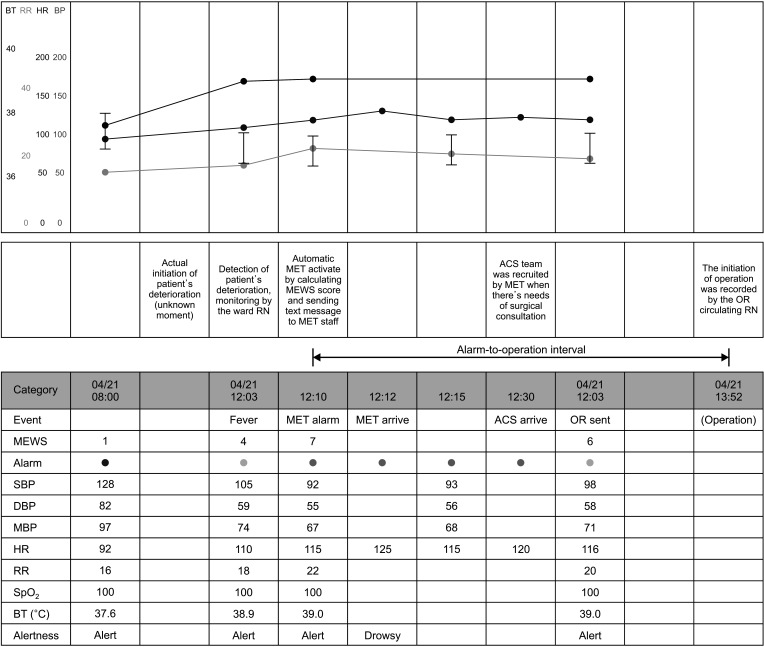
This was an observational before-and-after study. Emergency surgical cases of hospitalized patients were included in this study. Patients hospitalized in the Department of Emergency Medicine or Department of Surgery, directly comanaged by ACS were excluded. The primary outcome was in-hospital mortality rate. The secondary outcome was the alarm-to-operation interval, as recorded by a Modified Early Warning Score (MEWS) of >4.
Results
In total, 240 patients were included in the analysis (131 in the pre-ACS group and 109 in the post-ACS group). The in-hospital mortality rates in the pre- and post-ACS groups were 17.6% and 22.9%, respectively (P = 0.300). MEWS of >4 within 72 hours was recorded in 62 cases (31 in each group), and the median alarm-to-operation intervals of each group were 11 hours 16 minutes and 6 hours 41 minutes, respectively (P = 0.040).
Conclusion
Implementation of the ACS system resulted in faster surgical intervention in hospitalized patients, the need for which was detected early by the MET. The in-hospital mortality rates before and after ACS implementation were not significantly different.
Keyword
Figure
Reference
-
1. Jones DA, DeVita MA, Bellomo R. Rapid-response teams. N Engl J Med. 2011; 365:139–146. PMID: 21751906.2. Devita MA, Bellomo R, Hillman K, Kellum J, Rotondi A, Teres D, et al. Findings of the first consensus conference on medical emergency teams. Crit Care Med. 2006; 34:2463–2478. PMID: 16878033.3. Chana P, Burns EM, Arora S, Darzi AW, Faiz OD. A systematic review of the impact of dedicated emergency surgical services on patient outcomes. Ann Surg. 2016; 263:20–27. PMID: 26840649.4. Tran A, Fernando SM, McIsaac DI, Rochwerg B, Mok G, Seely AJ, et al. Predictors of mortality and cost among surgical patients requiring rapid response team activation. Can J Surg. 2020; 63:E598–E605. PMID: 33295715.5. Choi MS, Lee DS, Park CM. Evaluation of medical emergency team activation in surgical wards. J Acute Care Surg. 2019; 9:54–59.6. Committee to Develop the Reorganized Specialty of Trauma, Surgical Critical Care, and Emergency Surgery. Acute care surgery: trauma, critical care, and emergency surgery. J Trauma. 2005; 58:614–616. PMID: 15761359.7. Kim TH, Park JY, Jung YT, Lee SH, Jung MJ, Lee JG. 10 Years of acute care surgery: experiences in a single tertiary university hospital in Korea. J Acute Care Surg. 2020; 10:96–100.8. Park CI, Kim JH, Park SJ, Kim SH, Kim HH, Hong SK, et al. Acute care surgery: implementation in Korea. J Acute Care Surg. 2018; 8:51–58.9. Barnes SL, Cooper CJ, Coughenour JP, MacIntyre AD, Kessel JW. Impact of acute care surgery to departmental productivity. J Trauma. 2011; 71:1027–1034. PMID: 21986743.10. Kutcher ME, Sperry JL, Rosengart MR, Mohan D, Hoffman MK, Neal MD, et al. Surgical rescue: the next pillar of acute care surgery. J Trauma Acute Care Surg. 2017; 82:280–286. PMID: 27893639.11. Briggs A, Peitzman AB. Surgical rescue in medical patients: the role of acute care surgeons as the surgical rapid response team. Crit Care Clin. 2018; 34:209–219. PMID: 29482901.12. Gardner-Thorpe J, Love N, Wrightson J, Walsh S, Keeling N. The value of Modified Early Warning Score (MEWS) in surgical in-patients: a prospective observational study. Ann R Coll Surg Engl. 2006; 88:571–575. PMID: 17059720.13. Lim SY, Park SY, Park HK, Kim M, Park HY, Lee B, et al. Early impact of medical emergency team implementation in a country with limited medical resources: a before-and-after study. J Crit Care. 2011; 26:373–378. PMID: 21036527.14. Na SJ, Ko RE, Ko MG, Koh A, Chung CR, Suh GY, et al. Risk factors for early medical emergency team reactivation in hospitalized patients. Crit Care Med. 2020; 48:e1029–e1037. PMID: 32941188.15. Moreno RP, Metnitz PG, Almeida E, Jordan B, Bauer P, Campos RA, et al. SAPS 3: from evaluation of the patient to evaluation of the intensive care unit. Part 2: development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005; 31:1345–1355. PMID: 16132892.16. Ferreira FL, Bota DP, Bross A, Mélot C, Vincent JL. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001; 286:1754–1758. PMID: 11594901.17. Maharaj R, Raffaele I, Wendon J. Rapid response systems: a systematic review and meta-analysis. Crit Care. 2015; 19:254. PMID: 26070457.18. Lee DS, Suh GY, Ryu JA, Chung CR, Yang JH, Park CM, et al. Effect of early intervention on long-term outcomes of critically ill cancer patients admitted to ICUs. Crit Care Med. 2015; 43:1439–1448. PMID: 25803653.19. Yang E, Lee H, Lee SM, Kim S, Ryu HG, Lee HJ, et al. Effectiveness of a daytime rapid response system in hospitalized surgical ward patients. Acute Crit Care. 2020; 35:77–86. PMID: 32506872.20. Lee YJ, Lee DS, Min H, Choi YY, Lee EY, Song I, et al. Differences in the clinical characteristics of rapid response system activation in patients admitted to medical or surgical services. J Korean Med Sci. 2017; 32:688–694. PMID: 28244298.21. Ross SW, Reinke CE, Ingraham AM, Holena DN, Havens JM, Hemmila MR, et al. Emergency general surgery quality improvement: a review of recommended structure and key issues. J Am Coll Surg. 2022; 234:214–225. PMID: 35213443.22. Aggarwal G, Peden CJ, Mohammed MA, Pullyblank A, Williams B, Stephens T, et al. Evaluation of the collaborative use of an evidence-based care bundle in emergency laparotomy. JAMA Surg. 2019; 154:e190145. PMID: 30892581.23. Ciarleglio FA, Rigoni M, Mereu L, Tommaso C, Carrara A, Malossini G, et al. The negative effects of COVID-19 and national lockdown on emergency surgery morbidity due to delayed access. World J Emerg Surg. 2021; 16:37. PMID: 34256781.24. Gajic O, Urrutia LE, Sewani H, Schroeder DR, Cullinane DC, Peters SG. Acute abdomen in the medical intensive care unit. Crit Care Med. 2002; 30:1187–1190. PMID: 12072666.25. Patel SV, Groome PA, J Merchant S, Lajkosz K, Nanji S, Brogly SB. Timing of surgery and the risk of complications in patients with acute appendicitis: a population-level case-crossover study. J Trauma Acute Care Surg. 2018; 85:341–347. PMID: 29787550.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Organization and Roles of the Trauma Team
- Rapid response systems in Korea
- Disaster Medical Assistance Team
- New Concept of a Surgical Hospitalist: Early Experience of Managing the Admission, Critical Care, Trauma Surgery Team
- Comparison of Hospital Nurses' Recognition of the Team System and Effects on the Nursing Organizational Team System