Ann Surg Treat Res.
2023 Jan;104(1):18-26. 10.4174/astr.2023.104.1.18.
Comparison between laparoscopic pylorus-preserving gastrectomy and laparoscopic distal gastrectomy for overweight patients with early gastric cancer
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Surgery, College of Medicine, Taif University, Taif, Saudi Arabia
- 3Department of Surgery, Asan Medical Center, Seoul, Korea
- 4Department of Surgery, Gachon University Gil Medical Center, Incheon, Korea
- 5Department of Surgery, Seoul National University Bundang Hospital, Seoul, Korea
- 6Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 7Cancer Research Institute, Seoul National University, Seoul, Korea
- 8VITCAL, Co., Ltd., Seoul, Korea
- KMID: 2537623
- DOI: http://doi.org/10.4174/astr.2023.104.1.18
Abstract
- Purpose
Laparoscopic pylorus-preserving gastrectomy (LPPG) has a nutritional advantage over laparoscopic distal gastrectomy (LDG), however, may be less beneficial in overweight patients in terms of weight loss. The purpose of this study was to compare LPPG and LDG in overweight patients with early gastric cancer.
Methods
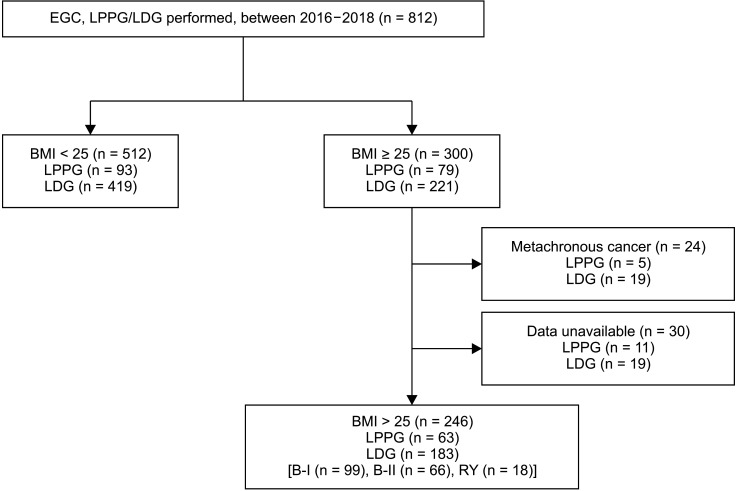
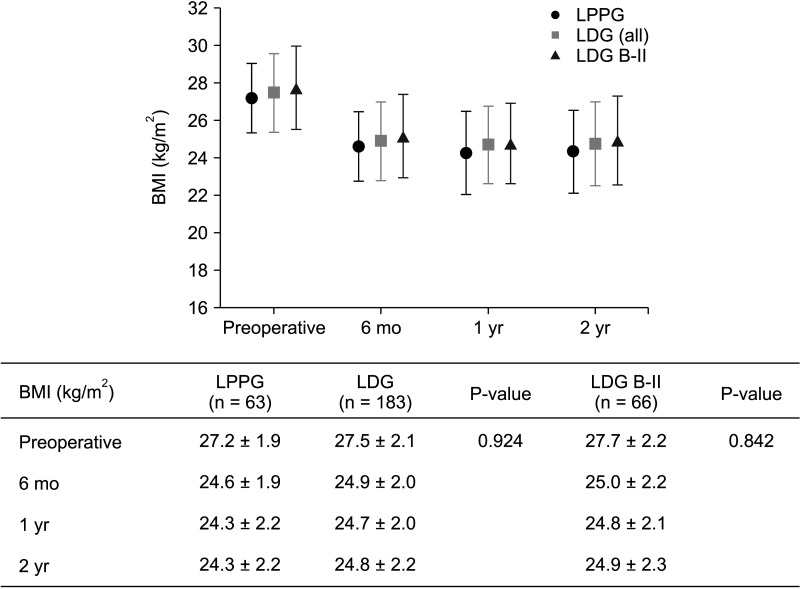
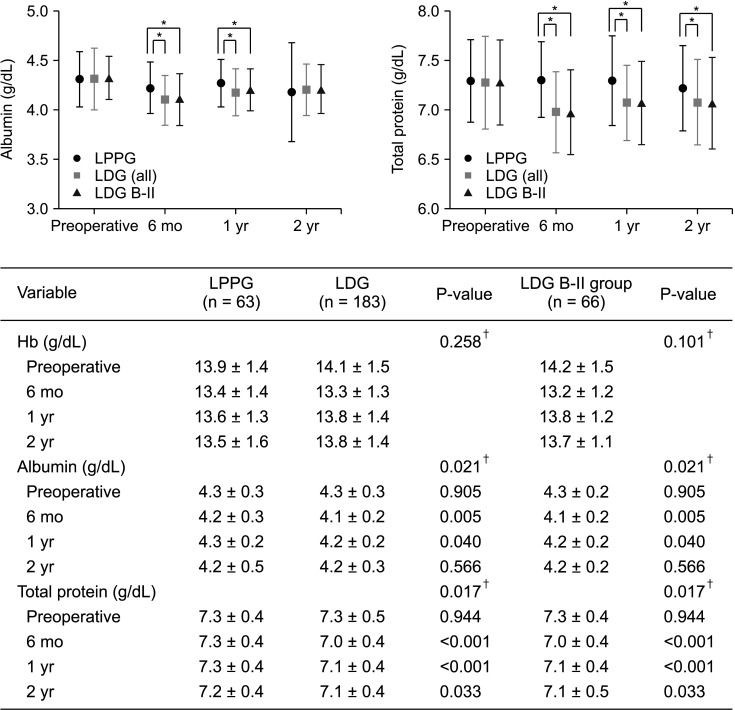
Clinicopathologic data of overweight patients (body mass index [BMI], ≥25 kg/m2 ) who underwent LPPG (n = 63) or LDG (n = 183) in 2016–2018 were retrospectively reviewed. In the LDG group, patients with Billroth-II anastomosis were separately grouped (LDG B-II, n = 66). Changes in BMI, hemoglobin, albumin, and total protein were compared among groups.
Results
Changes in BMI were not significant different among groups. The LPPG group had significantly higher albumin than the LDG group at postoperative 6 months and 1 year. The LPPG group had higher total protein than the LDG group at postoperative 2 years. The LPPG group had a higher complication rate of Clavien-Dindo classification III or higher (20.6%) than the LDG group (8.2%, P = 0.007). However, after excluding pyloric stenosis, there was no significant difference among groups (LPPG vs. LDG, P = 0.290; LPPG vs. LDG B-II, P = 0.921).
Conclusion
LPPG and LDG groups showed similar weight loss. However, the LPPG group had higher albumin and protein levels than the LDG group of overweight patients. Thus, it is not necessary to select LDG only for weight loss. LPPG may be selected as one option due to its potential nutritional benefit when pyloric stenosis is properly managed.
Keyword
Figure
Reference
-
1. Sasaki I, Fukushima K, Naito H, Matsuno S, Shiratori T, Maki T. Long-term results of pylorus-preserving gastrectomy for gastric ulcer. Tohoku J Exp Med. 1992; 168:539–548. PMID: 1306602.2. Information Committee of the Korean Gastric Cancer Association. Korean Gastric Cancer Association-led nationwide survey on surgically treated gastric cancers in 2019. J Gastric Cancer. 2021; 21:221–235. PMID: 34691807.3. Hotta T, Taniguchi K, Kobayashi Y, Johata K, Sahara M, Naka T, et al. Postoperative evaluation of pylorus-preserving procedures compared with conventional distal gastrectomy for early gastric cancer. Surg Today. 2001; 31:774–779. PMID: 11686554.4. Yamaguchi T, Ichikawa D, Kurioka H, Ikoma H, Koike H, Otsuji E, et al. Postoperative clinical evaluation following pylorus-preserving gastrectomy. Hepatogastroenterology. 2004; 51:883–886. PMID: 15143939.5. Park DJ, Lee HJ, Jung HC, Kim WH, Lee KU, Yang HK. Clinical outcome of pylorus-preserving gastrectomy in gastric cancer in comparison with conventional distal gastrectomy with Billroth I anastomosis. World J Surg. 2008; 32:1029–1036. PMID: 18256877.6. Park YS, Park DJ, Lee Y, Park KB, Min SH, Ahn SH, et al. Prognostic roles of perioperative body mass index and weight loss in the long-term survival of gastric cancer patients. Cancer Epidemiol Biomarkers Prev. 2018; 27:955–962. PMID: 29784729.7. Guideline Committee of the Korean Gastric Cancer Association (KGCA). Development Working Group & Review Panel. Korean Practice Guideline for Gastric Cancer 2018: an evidence-based, multi-disciplinary approach. J Gastric Cancer. 2019; 19:1–48. PMID: 30944757.8. Alzahrani K, Park JH, Lee HJ, Park SH, Choi JH, Wang C, et al. Short-term outcomes of pylorus-preserving gastrectomy for early gastric cancer: comparison between extracorporeal and intracorporeal gastrogastrostomy. J Gastric Cancer. 2022; 22:135–144. PMID: 35534450.9. Park DJ, Kim YW, Yang HK, Ryu KW, Han SU, Kim HH, et al. Short-term outcomes of a multicentre randomized clinical trial comparing laparoscopic pylorus-preserving gastrectomy with laparoscopic distal gastrectomy for gastric cancer (the KLASS-04 trial). Br J Surg. 2021; 108:1043–1049. PMID: 34487147.10. Oh SY, Lee HJ, Yang HK. Pylorus-preserving gastrectomy for gastric cancer. J Gastric Cancer. 2016; 16:63–71. PMID: 27433390.11. Hiramatsu Y, Kikuchi H, Takeuchi H. Function-preserving gastrectomy for early gastric cancer. Cancers (Basel). 2021; 13:6223. PMID: 34944841.12. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004; 240:205–213. PMID: 15273542.13. World Health Organization (WHO). Obesity and overweight [Internet]. Geneva: WHO;2021. cited 2021 Jun 9. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight .14. Suh YS, Han DS, Kong SH, Kwon S, Shin CI, Kim WH, et al. Laparoscopy-assisted pylorus-preserving gastrectomy is better than laparoscopy-assisted distal gastrectomy for middle-third early gastric cancer. Ann Surg. 2014; 259:485–493. PMID: 23652333.15. Tsujiura M, Hiki N, Ohashi M, Nunobe S, Kumagai K, Ida S, et al. Should pylorus-preserving gastrectomy be performed for overweight/obese patients with gastric cancer? Gastric Cancer. 2019; 22:1247–1255. PMID: 30888536.16. Jiang X, Hiki N, Nunobe S, Fukunaga T, Kumagai K, Nohara K, et al. Postoperative outcomes and complications after laparoscopy-assisted pylorus-preserving gastrectomy for early gastric cancer. Ann Surg. 2011; 253:928–933. PMID: 21358534.17. Fujita J, Takahashi M, Urushihara T, Tanabe K, Kodera Y, Yumiba T, et al. Assessment of postoperative quality of life following pylorus-preserving gastrectomy and Billroth-I distal gastrectomy in gastric cancer patients: results of the nationwide postgastrectomy syndrome assessment study. Gastric Cancer. 2016; 19:302–311. PMID: 25637175.18. Xia X, Xu J, Zhu C, Cao H, Yu F, Zhao G. Objective evaluation of clinical outcomes of laparoscopy-assisted pylorus-preserving gastrectomy for middle-third early gastric cancer. BMC Cancer. 2019; 19:481. PMID: 31117975.19. Tsujiura M, Hiki N, Ohashi M, Nunobe S, Kumagai K, Ida S, et al. Excellent long-term prognosis and favorable postoperative nutritional status after laparoscopic pylorus-preserving gastrectomy. Ann Surg Oncol. 2017; 24:2233–2240. PMID: 28280944.20. Wang CJ, Suh YS, Lee HJ, Park JH, Park SH, Choi JH, et al. Postoperative quality of life after gastrectomy in gastric cancer patients: a prospective longitudinal observation study. Ann Surg Treat Res. 2022; 103:19–31. PMID: 35919110.21. Schölmerich J. Postgastrectomy syndromes: diagnosis and treatment. Best Pract Res Clin Gastroenterol. 2004; 18:917–933. PMID: 15494286.22. Lim CH, Kim SW, Kim WC, Kim JS, Cho YK, Park JM, et al. Anemia after gastrectomy for early gastric cancer: long-term follow-up observational study. World J Gastroenterol. 2012; 18:6114–6119. PMID: 23155340.23. Rogers C. Postgastrectomy nutrition. Nutr Clin Pract. 2011; 26:126–136. PMID: 21447764.24. Pinheiro JS, Schiavon CA, Pereira PB, Correa JL, Noujaim P, Cohen R. Long-long limb Roux-en-Y gastric bypass is more efficacious in treatment of type 2 diabetes and lipid disorders in super-obese patients. Surg Obes Relat Dis. 2008; 4:521–527. PMID: 18539540.25. Kwon Y, Kim HJ, Lo Menzo E, Park S, Szomstein S, Rosenthal RJ. A systematic review and meta-analysis of the effect of Billroth reconstruction on type 2 diabetes: a new perspective on old surgical methods. Surg Obes Relat Dis. 2015; 11:1386–1395. PMID: 25892345.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracorporeal Anastomosis in Laparoscopic Gastric Cancer Surgery
- Laparoscopic Distal Gastrectomy for Gastric Cancer
- Function-Preserving Surgery in Gastric Cancer
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case
- A Comparison of Totally Laparoscopic Pylorus Preserving Gastrectomy and Laparoscopy-Assisted Pylorus Preserving Gastrectomy for Early Gastric Cancer