J Korean Med Sci.
2023 Jan;38(1):e4. 10.3346/jkms.2023.38.e4.
Rapid FEV 1 /FVC Decline Is Related With Incidence of Obstructive Lung Disease and Mortality in General Population
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Seoul National University College of Medicine, Seoul Metropolitan Government-Seoul National University Boramae Medical Center, Seoul, Korea
- KMID: 2537447
- DOI: http://doi.org/10.3346/jkms.2023.38.e4
Abstract
- Background
Forced expiratory volume in 1 second (FEV1 )/forced vital capacity (FVC) naturally decreases with age; however, an excessive decline may be related with increased morbidity and mortality. This study aimed to evaluate the FEV1 /FVC decline rate in the Korean general population and to identify whether rapid FEV1 /FVC decline is a risk factor for obstructive lung disease (OLD) and all-cause and respiratory mortality.
Methods
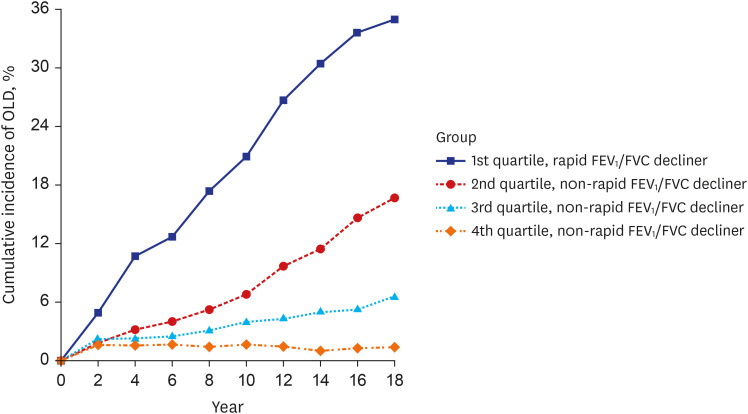
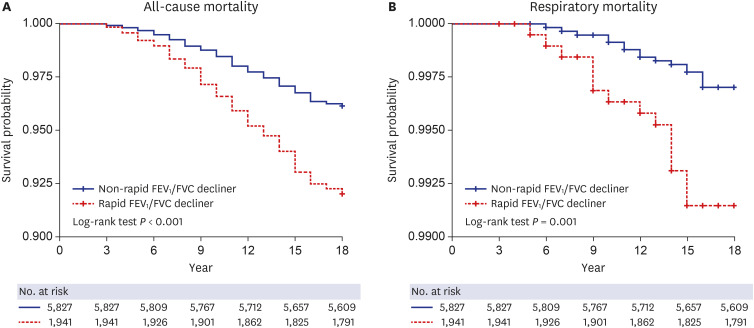
We evaluated individuals aged 40−69 years who underwent baseline and biannual follow-up spirometric assessments for up to 18 years, excluding those with airflow limitations at baseline. Based on the quartiles of the annual FEV1 /FVC decline rate, the most negative FEV1 /FVC change (1 st quartile of annual FEV1 /FVC decline rate) was classified as rapid FEV1 / FVC decline. We investigated the risk of progression to OLD and all-cause and respiratory mortality in individuals with rapid FEV1 /FVC decline.
Results
The annual FEV1 /FVC decline rate in the eligible 7,768 patients was 0.32 percentage point/year. The incidence rate of OLD was significantly higher in patients with rapid FEV1 / FVC decline than in those with non-rapid FEV1 /FVC decline (adjusted incidence rate, 2.119; 95% confidence interval [CI], 1.932–2.324). Rapid FEV1 /FVC decline was an independent risk factor for all-cause mortality (adjusted hazard [HR], 1.374; 95% CI, 1.105–1.709) and respiratory mortality (adjusted HR, 1.353; 95% CI, 1.089–1.680).
Conclusion
The annual FEV1 /FVC decline rate was 0.32%p in the general population in Korea. The incidence rate of OLD and the hazards of all-cause and respiratory mortality were increased in rapid FEV1 /FVC decliners.
Keyword
Figure
Reference
-
1. Ryu JH, Scanlon PD. Obstructive lung diseases: COPD, asthma, and many imitators. Mayo Clin Proc. 2001; 76(11):1144–1153. PMID: 11702903.2. Adeloye D, Chua S, Lee C, Basquill C, Papana A, Theodoratou E, et al. Global and regional estimates of COPD prevalence: systematic review and meta-analysis. J Glob Health. 2015; 5(2):020415. PMID: 26755942.3. Ogata H, Hirakawa Y, Matsumoto K, Hata J, Yoshida D, Fukuyama S, et al. Trends in the prevalence of airflow limitation in a general Japanese population: two serial cross-sectional surveys from the Hisayama Study. BMJ Open. 2019; 9(3):e023673.4. Amaral AF, Burney PG, Patel J, Minelli C, Mejza F, Mannino DM, et al. Chronic airflow obstruction and ambient particulate air pollution. Thorax. 2021; 76(12):1236–1241. PMID: 33975927.5. Tejero E, Prats E, Casitas R, Galera R, Pardo P, Gavilán A, et al. Classification of airflow limitation based on z-score underestimates mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2017; 196(3):298–305. PMID: 28306326.6. Huang S, Vasquez MM, Halonen M, Martinez FD, Guerra S. Asthma, airflow limitation and mortality risk in the general population. Eur Respir J. 2015; 45(2):338–346. PMID: 25323227.7. Hopkins RJ, Ko J, Gamble GD, Young RP. Airflow limitation and survival after surgery for non-small cell lung cancer: results from a systematic review and lung cancer screening trial (NLST-ACRIN sub-study). Lung Cancer. 2019; 135:80–87. PMID: 31447006.8. Lee MK, Kim SB, Lee JH, Lee SJ, Kim SH, Lee WY, et al. Association between airflow limitation and prognosis in patients with chronic pulmonary aspergillosis. J Thorac Dis. 2021; 13(2):681–688. PMID: 33717541.9. Heederik D, Kromhout H, Kromhout D, Burema J, Biersteker K. Relations between occupation, smoking, lung function, and incidence and mortality of chronic non-specific lung disease: the Zutphen Study. Br J Ind Med. 1992; 49(5):299–308. PMID: 1599867.10. Bugajski A, Frazier SK, Moser DK, Chung M, Lennie TA. Airflow limitation more than doubles the risk for hospitalization/mortality in patients with heart failure. Eur J Cardiovasc Nurs. 2019; 18(3):245–252. PMID: 30607982.11. Mangione CM, Barry MJ, Nicholson WK, Cabana M, Caughey AB, Chelmow D, et al. Screening for chronic obstructive pulmonary disease: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA. 2022; 327(18):1806–1811. PMID: 35536260.12. Guirguis-Blake JM, Senger CA, Webber EM, Mularski R, Whitlock EP. Preventive Services Task Force Evidence Syntheses, formerly Systematic Evidence Reviews. Screening for Chronic Obstructive Pulmonary Disease: A Systematic Evidence Review for the US Preventive Services Task Force. Rockville, MD, USA: Agency for Healthcare Research and Quality;2016.13. Perez-Padilla R, Vollmer WM, Vázquez-García JC, Enright PL, Menezes AM, Buist AS, et al. Can a normal peak expiratory flow exclude severe chronic obstructive pulmonary disease? Int J Tuberc Lung Dis. 2009; 13(3):387–393. PMID: 19275802.14. Frith P, Crockett A, Beilby J, Marshall D, Attewell R, Ratnanesan A, et al. Simplified COPD screening: validation of the PiKo-6® in primary care. Prim Care Respir J. 2011; 20(2):190–198. PMID: 21597667.15. Thorn J, Tilling B, Lisspers K, Jörgensen L, Stenling A, Stratelis G. Improved prediction of COPD in at-risk patients using lung function pre-screening in primary care: a real-life study and cost-effectiveness analysis. Prim Care Respir J. 2012; 21(2):159–166. PMID: 22270480.16. Thomas ET, Guppy M, Straus SE, Bell KJ, Glasziou P. Rate of normal lung function decline in ageing adults: a systematic review of prospective cohort studies. BMJ Open. 2019; 9(6):e028150.17. Liao SY, Lin X, Christiani DC. Occupational exposures and longitudinal lung function decline. Am J Ind Med. 2015; 58(1):14–20. PMID: 25384732.18. Gladysheva ES, Malhotra A, Owens RL. Influencing the decline of lung function in COPD: use of pharmacotherapy. Int J Chron Obstruct Pulmon Dis. 2010; 5:153–164. PMID: 20631815.19. Bang KM, Gergen PJ, Kramer R, Cohen B. The effect of pulmonary impairment on all-cause mortality in a national cohort. Chest. 1993; 103(2):536–540. PMID: 8432150.20. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007; 4(10):e296. PMID: 17941714.21. Kim Y, Han BG. KoGES group. Cohort profile: the Korean Genome and Epidemiology Study (KoGES) consortium. Int J Epidemiol. 2017; 46(2):e20. PMID: 27085081.22. Hnizdo E, Yan T, Hakobyan A, Enright P, Beeckman-Wagner LA, Hankinson J, et al. Spirometry longitudinal data analysis software (SPIROLA) for analysis of spirometry data in workplace prevention or COPD treatment. Open Med Inform J. 2010; 4(1):94–102. PMID: 20835361.23. Mannino DM, Reichert MM, Davis KJ. Lung function decline and outcomes in an adult population. Am J Respir Crit Care Med. 2006; 173(9):985–990. PMID: 16439715.24. Mannino DM, Davis KJ. Lung function decline and outcomes in an elderly population. Thorax. 2006; 61(6):472–477. PMID: 16517577.25. Kesten S, Celli B, Decramer M, Liu D, Tashkin D. Adverse health consequences in COPD patients with rapid decline in FEV1--evidence from the UPLIFT trial. Respir Res. 2011; 12(1):129. PMID: 21955733.26. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Updated 2022. Accessed January 27, 2022. http://www.goldcopd.org/ .27. Lange P, Celli B, Agustí A, Boje Jensen G, Divo M, Faner R, et al. Lung-function trajectories leading to chronic obstructive pulmonary disease. N Engl J Med. 2015; 373(2):111–122. PMID: 26154786.28. Han MK, Agusti A, Celli BR, Criner GJ, Halpin DM, Roche N, et al. From GOLD 0 to Pre-COPD. Am J Respir Crit Care Med. 2021; 203(4):414–423. PMID: 33211970.29. Talaminos Barroso A, Márquez Martín E, Roa Romero LM, Ortega Ruiz F. Factors affecting lung function: a review of the literature. Arch Bronconeumol (Engl Ed). 2018; 54(6):327–332. PMID: 29496283.30. Sun Y, Milne S, Jaw JE, Yang CX, Xu F, Li X, et al. BMI is associated with FEV1 decline in chronic obstructive pulmonary disease: a meta-analysis of clinical trials. Respir Res. 2019; 20(1):236. PMID: 31665000.31. Wijnant SR, De Roos E, Kavousi M, Stricker BH, Terzikhan N, Lahousse L, et al. Trajectory and mortality of preserved ratio impaired spirometry: the Rotterdam Study. Eur Respir J. 2020; 55(1):1901217. PMID: 31601717.32. Lee HW, Lee HJ, Lee JK, Park TY, Heo EY, Kim DK. Rapid FEV1 decline and lung cancer incidence in South Korea. Chest. 2022; 162(2):466–474. PMID: 35318007.33. Tantucci C, Modina D. Lung function decline in COPD. Int J Chron Obstruct Pulmon Dis. 2012; 7:95–99. PMID: 22371650.34. Mannino DM, Buist AS, Petty TL, Enright PL, Redd SC. Lung function and mortality in the United States: data from the First National Health and Nutrition Examination Survey follow up study. Thorax. 2003; 58(5):388–393. PMID: 12728157.35. Weinmayr G, Schulz H, Klenk J, Denkinger M, Duran-Tauleria E, Koenig W, et al. Association of lung function with overall mortality is independent of inflammatory, cardiac, and functional biomarkers in older adults: the ActiFE-study. Sci Rep. 2020; 10(1):11862. PMID: 32681112.36. Collaro AJ, Chang AB, Marchant JM, Chatfield MD, Dent A, Blake T, et al. Associations between lung function and future cardiovascular morbidity and overall mortality in a predominantly First Nations population: a cohort study. Lancet Reg Health West Pac. 2021; 13:100188. PMID: 34527981.37. Sabia S, Shipley M, Elbaz A, Marmot M, Kivimaki M, Kauffmann F, et al. Why does lung function predict mortality? Results from the Whitehall II Cohort Study. Am J Epidemiol. 2010; 172(12):1415–1423. PMID: 20961971.38. Baines KJ, Backer V, Gibson PG, Powel H, Porsbjerg CM. Impaired lung function is associated with systemic inflammation and macrophage activation. Eur Respir J. 2015; 45(2):557–559. PMID: 25504991.39. Shrine N, Guyatt AL, Erzurumluoglu AM, Jackson VE, Hobbs BD, Melbourne CA, et al. New genetic signals for lung function highlight pathways and chronic obstructive pulmonary disease associations across multiple ancestries. Nat Genet. 2019; 51(3):481–493. PMID: 30804560.40. Sikdar S, Wyss AB, Lee MK, Hoang TT, Richards M, Beane Freeman LE, et al. Interaction between Genetic Risk Scores for reduced pulmonary function and smoking, asthma and endotoxin. Thorax. 2021; 76(12):1219–1226. PMID: 33963087.41. Lundbäck B, Lindberg A, Lindström M, Rönmark E, Jonsson AC, Jönsson E, et al. Not 15 but 50% of smokers develop COPD?--report from the obstructive lung disease in Northern Sweden studies. Respir Med. 2003; 97(2):115–122. PMID: 12587960.42. Carter BD, Abnet CC, Feskanich D, Freedman ND, Hartge P, Lewis CE, et al. Smoking and mortality--beyond established causes. N Engl J Med. 2015; 372(7):631–640. PMID: 25671255.43. Godtfredsen NS, Lam TH, Hansel TT, Leon ME, Gray N, Dresler C, et al. COPD-related morbidity and mortality after smoking cessation: status of the evidence. Eur Respir J. 2008; 32(4):844–853. PMID: 18827152.44. Tommola M, Ilmarinen P, Tuomisto LE, Haanpää J, Kankaanranta T, Niemelä O, et al. The effect of smoking on lung function: a clinical study of adult-onset asthma. Eur Respir J. 2016; 48(5):1298–1306. PMID: 27660515.45. Braber S, Henricks PA, Nijkamp FP, Kraneveld AD, Folkerts G. Inflammatory changes in the airways of mice caused by cigarette smoke exposure are only partially reversed after smoking cessation. Respir Res. 2010; 11(1):99. PMID: 20649997.46. Sterk PJ. Let’s not forget: the GOLD criteria for COPD are based on post-bronchodilator FEV1. Eur Respir J. 2004; 23(4):497–498. PMID: 15083741.47. Celli BR, Halbert RJ, Isonaka S, Schau B. Population impact of different definitions of airway obstruction. Eur Respir J. 2003; 22(2):268–273. PMID: 12952259.48. Kitaguchi Y, Fujimoto K, Hayashi R, Hanaoka M, Honda T, Kubo K. Annual changes in pulmonary function in combined pulmonary fibrosis and emphysema: over a 5-year follow-up. Respir Med. 2013; 107(12):1986–1992. PMID: 23850272.49. Paulin LM, Diette GB, Blanc PD, Putcha N, Eisner MD, Kanner RE, et al. Occupational exposures are associated with worse morbidity in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2015; 191(5):557–565. PMID: 25562375.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Study on Lung Function in Patients with Bronchogenic Cancer
- Risk of Rapid Lung Function Decline in Young Adults With Chronic Obstructive Pulmonary Disease: A Community-Based Prospective Cohort Study
- Comparison of Predicted Postoperative Lung Function in Pneumonectomy Using Computed Tomography and Lung Perfusion Scans
- The Impact of Erosive Reflux Esophagitis on the Decline of Lung Function in the General Population
- A genome wide association study for lung function in the Korean population using an exome array