Korean J healthc assoc Infect Control Prev.
2022 Dec;27(2):162-167. 10.14192/kjicp.2022.27.2.162.
Outbreaks of Carbapenem Resistant Enterobacterales (CRE) According to the Type of Hospitals
- Affiliations
-
- 1Team of Waterborne Disease, Gyeonggi Province Institute of Health and Environment, Suwon, Korea
- KMID: 2537077
- DOI: http://doi.org/10.14192/kjicp.2022.27.2.162
Abstract
- Background
Carbapenem-resistant Enterobacterales(CRE) are increasing rapidly worldwide, posing a major threat to global health. This study aimed to identify the epidemiological characteristics of CRE isolated in Gyeonggi-do according to hospital type.
Methods
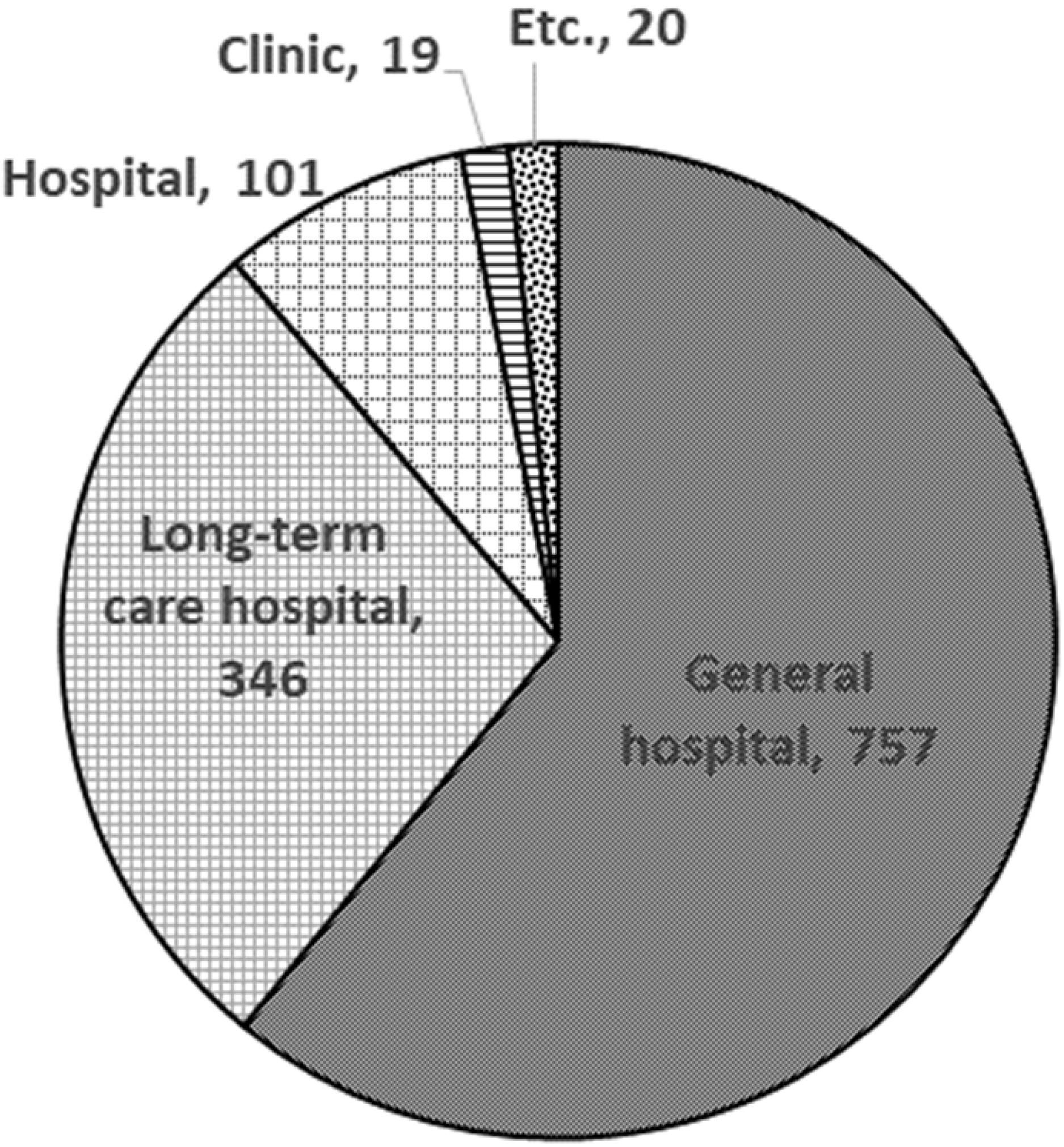
We conducted antibiotic susceptibility and genetic tests for carbapenemase-producing Enterobacterales (CPE) among 1,243 clinical isolates of CRE from Gyeonggi-do in 2019. CRE strains were identified using MALDI-TOF (Microflex, BRUKER, Germany), and antimicrobial susceptibility tests were performed using the broth microdilution method, according to the CLSI guidelines. Genetic testing of the CPE type was performed for KPC, NDM, OXA-48, IMP, VIM, and GES.
Results
Most CRE infections in Gyeonggi-do occurred in general hospitals (60.9%) and long-term care hospitals (27.8%). While the proportion of the CPE group in general hospitals was low (55.7%), 85.0% of CRE isolates in long-term care hospitals were identified in the CPE group. In the CPE group, the proportion of CRE isolates above the minimum inhibitory concentration of carbapenem namely meropenem, imipenem, and doripenem was 76.0%, 90.2%, and 66.5%, respectively. The non-CPE group showed a relatively low resistance percentage (44.6% [meropenem], 27.6% [imipenem], and 25.2% [doripenem]) compared to the CPE group. Furthermore, we found a correlation between CPE genes and carbapenem resistance rate on the Kruskal–Wallis test (P≤0.05).
Conclusion
Carbapenem resistance rate and the genetic characteristics of CRE isolates differed according to the type of hospital in which they occurred. The high proportion of the CPE group in long-term care hospitals indicates the need for more attention to strict infection control in these hospitals.
Keyword
Figure
Reference
-
1. O'Neill J. 2016. Tackling drug-resistant infections globally: final report and recommendations. Government of the United Kingdom;London: p. 10–17.2. Rex JH, Pfaller MA. 2002; Has antifungal susceptibility testing come of age? Clin Infect Dis. 35:982–9. DOI: 10.1086/342384. PMID: 12355386.
Article3. Solomon SL, Oliver KB. 2014; Antibiotic resistance threats in the United States: stepping back from the brink. Am Fam Physician. 89:938–41. PMID: 25162160.4. Ben-David D, Kordevani R, Keller N, Tal I, Marzel A, Gal-Mor O, et al. 2012; Outcome of carbapenem resistant Klebsiella pneumoniae bloodstream infections. Clin Microbiol Infect. 18:54–60. DOI: 10.1111/j.1469-0691.2011.03478.x. PMID: 21722257.
Article5. Centers for Disease Control. 2009; Guidance for control of infections with carbapenem-resistant or carbapenemase-producing Enterobacteriaceae in acute care facilities. MMWR Morb Mortal Wkly Rep. 58:256–60. PMID: 19300408.6. Lee E, Lee S, Yoon S, Lee Y. 2021; Number of cabapenem-resistant Enterobacteriaceae infections in Republic of Korea (2018-2020). Public Health Wkly Rep. 14:2765–72.7. Trecarichi EM, Tumbarello M. 2017; Therapeutic options for carbapenem-resistant Enterobacteriaceae infections. Virulence. 8:470–84. DOI: 10.1080/21505594.2017.1292196. PMID: 28276996. PMCID: PMC5477725.
Article8. Lee CS, Doi Y. 2014; Therapy of infections due to carbapenem-resistant gram-negative pathogens. Infect Chemother. 46:149–64. DOI: 10.3947/ic.2014.46.3.149. PMID: 25298904. PMCID: PMC4189141.
Article9. Papst L, Beović B, Pulcini C, Durante-Mangoni E, Rodríguez-Baño J, Kaye KS, et al. 2018; Antibiotic treatment of infections caused by carbapenem-resistant Gram-negative bacilli: an international ESCMID cross-sectional survey among infectious diseases specialists practicing in large hospitals. Clin Microbiol Infect. 24:1070–6. DOI: 10.1016/j.cmi.2018.01.015. PMID: 29410094.
Article10. Wi YM, Kang CI. 2018; Antimicrobial therapy for infections caused by carbapenem-resistant Gram-negative bacteria. Korean J Med. 93:439–46. DOI: 10.3904/kjm.2018.93.5.439.
Article11. Codjoe FS, Donkor ES. 2017; Carbapenem resistance: a review. Med Sci (Basel). 6:1. DOI: 10.3390/medsci6010001. PMID: 29267233. PMCID: PMC5872158.
Article12. Majewski P, Wieczorek P, Łapuć I, Ojdana D, Sieńko A, Sacha P, et al. 2017; Emergence of a multidrug-resistant Citrobacter freundii ST8 harboring an unusual VIM-4 gene cassette in Poland. Int J Infect Dis. 61:70–3. DOI: 10.1016/j.ijid.2017.05.016. PMID: 28602727.
Article13. Venditti C, Fortini D, Villa L, Vulcano A, D'Arezzo S, Capone A, et al. 2017; Circulation of blaKPC-3-carrying IncX3 plasmids among Citrobacter freundii isolates in an Italian hospital. Antimicrob Agents Chemother. 61:e00505–17. DOI: 10.1128/AAC.00505-17. PMID: 28559268. PMCID: PMC5527586.14. Lin MY, Lyles-Banks RD, Lolans K, Hines DW, Spear JB, Petrak R, et al. 2013; The importance of long-term acute care hospitals in the regional epidemiology of Klebsiella pneumoniae carbapenemase-producing Enterobacteriaceae. Clin Infect Dis. 57:1246–52. DOI: 10.1093/cid/cit500. PMID: 23946222. PMCID: PMC8383150.15. Snitkin ES, Zelazny AM, Thomas PJ, Stock F, Henderson DK, Palmore TN, et al. 2012; Tracking a hospital outbreak of carbapenem-resistant Klebsiella pneumoniae with whole-genome sequencing. Sci Transl Med. 4:148ra116. DOI: 10.1126/scitranslmed.3004129. PMID: 22914622. PMCID: PMC3521604.
Article16. Kim JS, Jin YH, Park SH, Han S, Kim HS, Park JH, et al. 2019; Emergence of a multidrug-resistant clinical isolate of Escherichia coli ST8499 strain producing NDM-13 carbapenemase in the Republic of Korea. Diagn Microbiol Infect Dis. 94:410–2. DOI: 10.1016/j.diagmicrobio.2019.02.013. PMID: 30879710.
Article17. Clinical. 2011. Performance standards for antimicrobial susceptibility testing; twenty-first informational supplement. Clinical and Laboratory Standards Institute;Wayne: p. 50. DOI: 10.1016/j.diagmicrobio.2019.02.013.18. Wang Q, Wang X, Wang J, Ouyang P, Jin C, Wang R, et al. 2018; Phenotypic and genotypic characterization of carbapenem-resistant Enterobacteriaceae: data from a longitudinal large-scale CRE study in China (2012-2016). Clin Infect Dis. 67(suppl_2):S196–205. DOI: 10.1093/cid/ciy660. PMID: 30423057.19. Arnold RS, Thom KA, Sharma S, Phillips M, Kristie Johnson J, Morgan DJ. 2011; Emergence of Klebsiella pneumoniae carbapenemase-producing bacteria. South Med J. 104:40–5. DOI: 10.1097/SMJ.0b013e3181fd7d5a. PMID: 21119555. PMCID: PMC3075864.
Article20. Yan L, Sun J, Xu X, Huang S. 2020; Epidemiology and risk factors of rectal colonization of carbapenemase-producing Enterobacteriaceae among high-risk patients from ICU and HSCT wards in a university hospital. Antimicrob Resist Infect Control. 9:155. DOI: 10.1186/s13756-020-00816-4. PMID: 32967718. PMCID: PMC7513325.
Article21. Tamma PD, Goodman KE, Harris AD, Tekle T, Roberts A, Taiwo A, et al. 2017; Comparing the outcomes of patients with carbapenemase-producing and non-carbapenemase-producing carbapenem-resistant Enterobacteriaceae bacteremia. Clin Infect Dis. 64:257–64. DOI: 10.1093/cid/ciw741. PMID: 28013264. PMCID: PMC5241781.22. Hussein K, Raz-Pasteur A, Finkelstein R, Neuberger A, Shachor-Meyouhas Y, Oren I, et al. 2013; Impact of carbapenem resistance on the outcome of patients' hospital-acquired bacteraemia caused by Klebsiella pneumoniae. J Hosp Infect. 83:307–13. DOI: 10.1016/j.jhin.2012.10.012. PMID: 23313086.
Article23. Toth DJA, Khader K, Slayton RB, Kallen AJ, Gundlapalli AV, O'Hagan JJ, et al. 2017; The potential for interventions in a long-term acute care hospital to reduce transmission of carbapenem-resistant Enterobacteriaceae in affiliated healthcare facilities. Clin Infect Dis. 65:581–7. DOI: 10.1093/cid/cix370. PMID: 28472233.
Article24. Ben-David D, Masarwa S, Fallach N, Temkin E, Solter E, Carmeli Y, et al. 2019; Success of a national intervention in controlling carbapenem-resistant Enterobacteriaceae in Israel's long-term care facilities. Clin Infect Dis. 68:964–71. DOI: 10.1093/cid/ciy572. PMID: 29986007.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Value and Clinical Application of Carbapenem-resistant Enterobacterales Surveillance Culture
- Carbapenem-resistant Enterobacteriaceae in Korea
- Identification and infection control of carbapenem-resistant Enterobacterales in intensive care units
- A Study on the Status and Genetic Characteristics of Carbapenem Resistance of Clinical-derived Bacteria in Northern Gyeonggi Province
- Epidemiological Characteristics of Carbapenemase Producing Carbapenem-Resistant Enterobacteriaceae Colonization