Cardiovasc Prev Pharmacother.
2022 Jan;4(1):26-33. 10.36011/cpp.2022.4.e6.
Safety and efficacy of low-dose aspirin in patients with coronary artery spasm: long-term clinical follow-up
- Affiliations
-
- 1Department of Cardiology, Cardiovascular Center, Korea University Guro Hospital, Seoul, Korea
- 2Department of Cardiology, Cardiovascular Center, Incheon Sejong Hospital, Incheon, Korea
- KMID: 2536930
- DOI: http://doi.org/10.36011/cpp.2022.4.e6
Abstract
- Background
Aspirin is known to aggravate coronary artery spasm (CAS) regardless of the dose (100–325 mg/day). However, it is unclear whether low-dose aspirin (LDA; 100 mg) has deleterious impacts on the clinical course of CAS patients in the long-term. Thus, we investigated the impact of LDA on the long-term clinical outcomes of CAS patients.
Methods
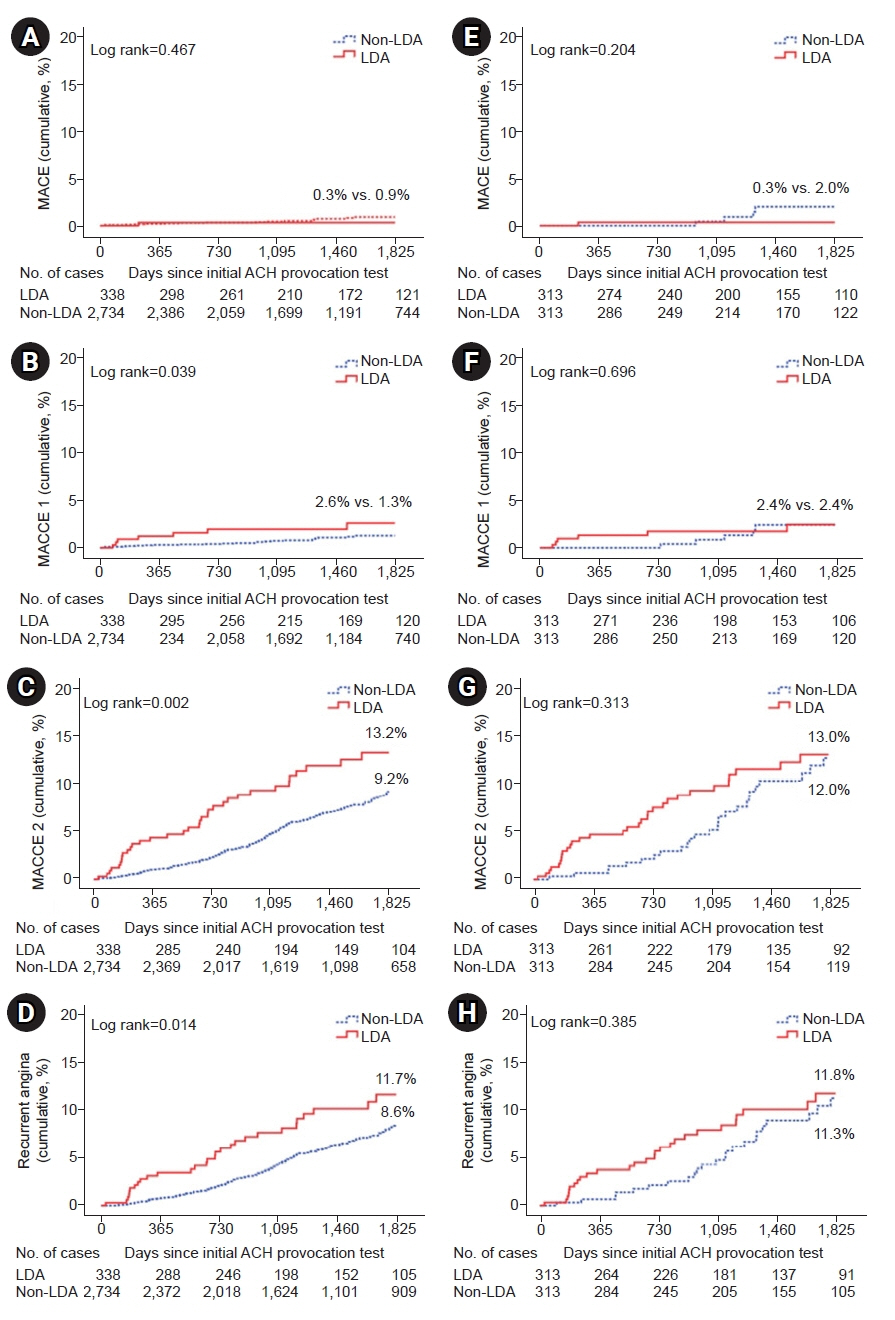
A total of 5,697 consecutive patients without significant coronary artery disease who underwent an acetylcholine provocation test from November 2004 to May 2015 were enrolled. Of these patients, 3,072 CAS patients were enrolled in the study and divided into two groups based on whether they took LDA: the LDA group (n=338) and the non-LDA group (n=2,734). All CAS patients were prescribed anti-anginal medication as appropriate. To adjust for any potential confounders that could cause bias, a propensity score matching analysis was performed using a logistic regression model.
Results
After propensity score matching, two propensity-matched groups (524 pairs, 1,048 patients, C-statistic=0.827) were generated, and the baseline characteristics of the two groups were balanced. The two groups were showed no significant differences in any follow-up events, such as major adverse cardiac events and recurrent angina.
Conclusions
The main finding of the present study is that the use of LDA did not affect cardiovascular events up to 5 years in CAS patients. Therefore, the prescription of LDA in these patients should be individualized considering their clinical status.
Keyword
Figure
Reference
-
1. Picard F, Sayah N, Spagnoli V, Adjedj J, Varenne O. Vasospastic angina: a literature review of current evidence. Arch Cardiovasc Dis. 2019; 112:44–55.
Article2. Stern S, Bayes de Luna A. Coronary artery spasm: a 2009 update. Circulation. 2009; 119:2531–4.3. Yasue H, Nakagawa H, Itoh T, Harada E, Mizuno Y. Coronary artery spasm: clinical features, diagnosis, pathogenesis, and treatment. J Cardiol. 2008; 51:2–17.
Article4. Park JY, Rha SW, Poddar KL, Ramasamy S, Chen KY, Li YJ, et al. Impact of low-dose aspirin on coronary artery spasm as assessed by intracoronary acetylcholine provocation test in Korean patients. J Cardiol. 2012; 60:187–91.
Article5. Choi BG, Park SH, Rha SW, Park JY, Choi SY, Park Y, et al. Five-year clinical outcomes in patients with significant coronary artery spasm: a propensity score-matched analysis. Int J Cardiol. 2015; 184:533–9.
Article6. Chen KY, Rha SW, Li YJ, Poddar KL, Jin Z, Minami Y, et al. Peripheral arterial disease is associated with coronary artery spasm as assessed by an intracoronary acetylcholine provocation test. Clin Exp Pharmacol Physiol. 2009; 36:e78–82.
Article7. Chen KY, Rha SW, Li YJ, Poddar KL, Jin Z, Minami Y, et al. Impact of hypertension on coronary artery spasm as assessed with intracoronary acetylcholine provocation test. J Hum Hypertens. 2010; 24:77–85.
Article8. Li YJ, Hyun MH, Rha SW, Chen KY, Jin Z, Dang Q, et al. Diabetes mellitus is not a risk factor for coronary artery spasm as assessed by an intracoronary acetylcholine provocation test: angiographic and clinical characteristics of 986 patients. J Invasive Cardiol. 2014; 26:234–9.9. Mishra PK. Variations in presentation and various options in management of variant angina. Eur J Cardiothorac Surg. 2006; 29:748–59.
Article10. Miwa K, Kambara H, Kawai C. Effect of aspirin in large doses on attacks of variant angina. Am Heart J. 1983; 105:351–5.
Article11. Cutlip DE, Windecker S, Mehran R, Boam A, Cohen DJ, van Es GA, et al. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007; 115:2344–51.12. Patrono C, Garcia Rodriguez LA, Landolfi R, Baigent C. Low-dose aspirin for the prevention of atherothrombosis. N Engl J Med. 2005; 353:2373–83.
Article13. Weisman SM, Graham DY. Evaluation of the benefits and risks of low-dose aspirin in the secondary prevention of cardiovascular and cerebrovascular events. Arch Intern Med. 2002; 162:2197–202.
Article14. Berger JS, Brown DL, Becker RC. Low-dose aspirin in patients with stable cardiovascular disease: a meta-analysis. Am J Med. 2008; 121:43–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Right Gastroepiploic Artery Spasm during Pst-CABG Coronary Angiography
- Follow-up Provocation Test in Patients with Coronary Artery Spasm
- Thrombolytic Therapy and Long Term Follow-up Study in a Child with Kawasaki Disease Complicated by Giant Coronary Aneurysm with Thrombosis
- The outcome of short-term low-dose aspirin treatment in Kawasaki disease based on inflammatory markers
- Feel Free to Use Aspirin before Coronary Artery Bypass Surgery