J Korean Med Sci.
2022 Dec;37(47):e333. 10.3346/jkms.2022.37.e333.
Epidemiology and Management Trend of Renal Trauma: Results of a Nationwide Population-Based Study
- Affiliations
-
- 1Department of Urology, Korea University Ansan Hospital, Korea University College of Medicine, Ansan, Korea
- 2Uh Urology Clinic, Seoul, Korea
- 3Department of Urology, Sanggye Paik Hospital, Inje University, Seoul, Korea
- 4Department of Urology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 5Department of Urology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- KMID: 2536515
- DOI: http://doi.org/10.3346/jkms.2022.37.e333
Abstract
- Background
To analyze the incidence of renal trauma using the National Health Insurance Service Database (NHISD).
Methods
Using the NHISD, representative of all upper urinary tract injuries in Korea, data regarding renal trauma were analyzed. The International Classification of Diseases, Tenth Revision Clinical Modification codes were used to identify the diagnoses. The incidence estimates of renal traumas were analyzed using Poisson regression analysis. Risk factors for high-grade renal trauma were estimated using multivariable logistic regression analyses.
Results
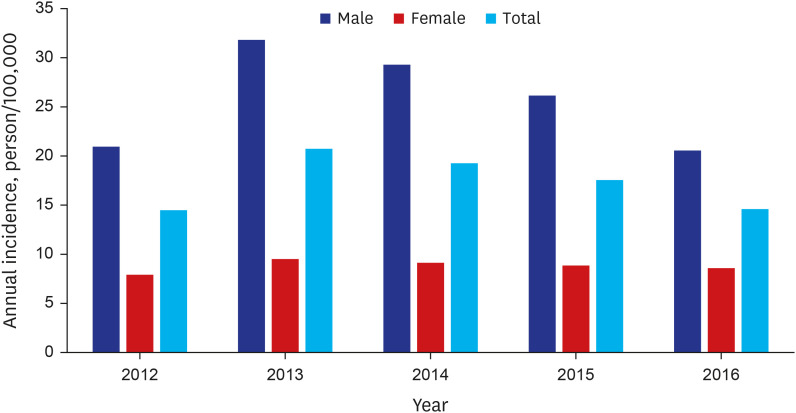
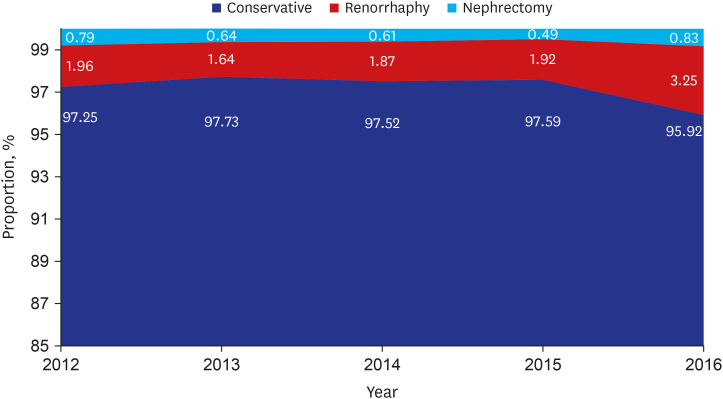
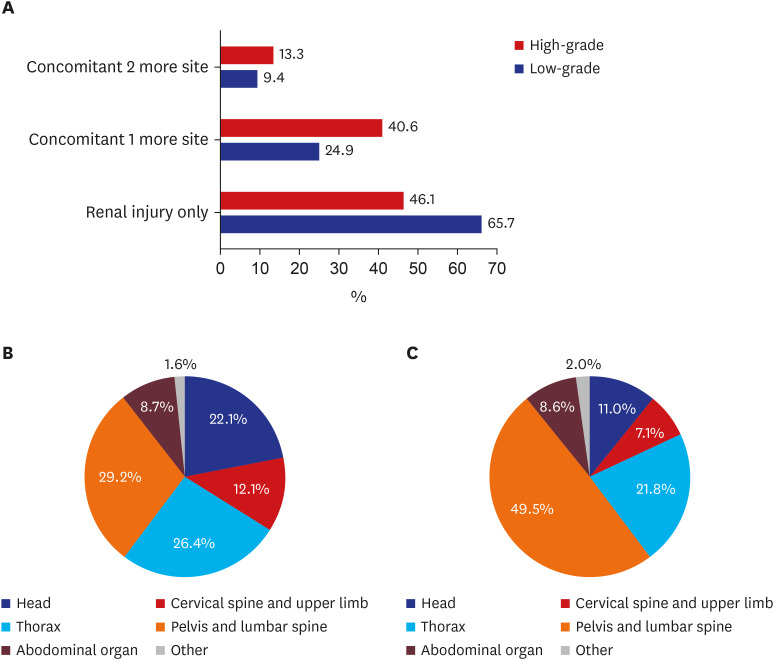
Patients with renal trauma were identified from a nationwide database collected by the National Health Insurance Service of Korea between 2012 and 2016. Among 37,683 individuals with renal trauma, 1,293 (3.4%) were diagnosed with high-grade renal trauma. Surgical therapy was performed in 995 (2.6%) patients with renal trauma and 184 (14.2%) patients with high-grade renal trauma. Renal trauma occurred in all age groups, and the ratio between men and women was approximately 3:1. Men and women experienced 8,000 (31.82/100,000) and 2,365 (9.52/100,000) renal trauma in 2013 (total 10,365, 20.73/100,000) and 5,243 (20.56/100.000) and 2,168 (8.58/100,000) in 2016 (total 7,411, 14.60/100,000), respectively. In multivariable analysis, female sex, age (age; 41–60 and 61–80 years), and comorbidity of peripheral vascular disease, renal disease, and malignancy were revealed as risk factors for high-grade renal trauma.
Conclusion
Annual incidence of renal trauma is 17.33 per 100,000 population from 2012 to 2016. The incidence of kidney damage decreased gradually from 2013 to 2016, and the majority of renal trauma cases were low-grade. Conservative management was the preferred treatment modality in most patients with renal trauma, including those with high-grade renal trauma.
Keyword
Figure
Reference
-
1. Moore EE, Shackford SR, Pachter HL, McAninch JW, Browner BD, Champion HR, et al. Organ injury scaling: spleen, liver, and kidney. J Trauma. 1989; 29(12):1664–1666. PMID: 2593197.2. Meng MV, Brandes SB, McAninch JW. Renal trauma: indications and techniques for surgical exploration. World J Urol. 1999; 17(2):71–77. PMID: 10367364.3. Santucci RA, Wessells H, Bartsch G, Descotes J, Heyns CF, McAninch JW, et al. Evaluation and management of renal injuries: consensus statement of the renal trauma subcommittee. BJU Int. 2004; 93(7):937–954. PMID: 15142141.4. Carroll PR, Klosterman PW, McAninch JW. Surgical management of renal trauma: analysis of risk factors, technique, and outcome. J Trauma. 1988; 28(7):1071–1077. PMID: 3398086.5. Broghammer JA, Fisher MB, Santucci RA. Conservative management of renal trauma: a review. Urology. 2007; 70(4):623–629. PMID: 17991526.6. Elashry OM, Dessouky BA. Conservative management of major blunt renal trauma with extravasation: a viable option? Eur J Trauma Emerg Surg. 2009; 35(2):115–123. PMID: 26814763.7. Shoobridge JJ, Bultitude MF, Koukounaras J, Martin KE, Royce PL, Corcoran NM. A 9-year experience of renal injury at an Australian level 1 trauma centre. BJU Int. 2013; 112(Suppl 2):53–60. PMID: 23418742.8. Hampson LA, Radadia KD, Odisho AY, McAninch JW, Breyer BN. Conservative management of high-grade renal trauma does not lead to prolonged hospital stay. Urology. 2018; 115:92–95. PMID: 29203185.9. Tae BS, Yoon YE, Na W, Oh KJ, Park SY, Park JY, et al. Epidemiologic study of bladder and urethral injury in Korea: a nationwide population-based study. Investig Clin Urol. 2022; 63(1):92–98.10. Song SO, Jung CH, Song YD, Park CY, Kwon HS, Cha BS, et al. Background and data configuration process of a nationwide population-based study using the Korean National Health Insurance System. Diabetes Metab J. 2014; 38(5):395–403. PMID: 25349827.11. Kozar RA, Crandall M, Shanmuganathan K, Zarzaur BL, Coburn M, Cribari C, et al. Organ injury scaling 2018 update: spleen, liver, and kidney. J Trauma Acute Care Surg. 2018; 85(6):1119–1122. PMID: 30462622.12. Wessells H, Suh D, Porter JR, Rivara F, MacKenzie EJ, Jurkovich GJ, et al. Renal injury and operative management in the United States: results of a population-based study. J Trauma. 2003; 54(3):423–430. PMID: 12634519.13. McClung CD, Hotaling JM, Wang J, Wessells H, Voelzke BB. Contemporary trends in the immediate surgical management of renal trauma using a national database. J Trauma Acute Care Surg. 2013; 75(4):602–606. PMID: 24064872.14. Buckley JC, McAninch JW. Pediatric renal injuries: management guidelines from a 25-year experience. J Urol. 2004; 172(2):687–690. PMID: 15247762.15. Grimsby GM, Voelzke B, Hotaling J, Sorensen MD, Koyle M, Jacobs MA. Demographics of pediatric renal trauma. J Urol. 2014; 192(5):1498–1502. PMID: 24907442.16. Bryk DJ, Zhao LC. Guideline of guidelines: a review of urological trauma guidelines. BJU Int. 2016; 117(2):226–234. PMID: 25600513.17. Oh JW, Lim J, Lee SH, Jin YS, Oh B, Lee CG, et al. Results from South Korea’s 2018 report card on physical activity for children and youth. J Phys Act Health. 2018; 15(S2):S409–S410. PMID: 30475150.18. Morey AF, Brandes S, Dugi DD 3rd, Armstrong JH, Breyer BN, Broghammer JA, et al. Urotrauma: AUA guideline. J Urol. 2014; 192(2):327–335. PMID: 24857651.19. Aldiwani M, Georgiades F, Omar I, Angel-Scott H, Tharakan T, Vale J, et al. Traumatic renal injury in a UK major trauma centre - current management strategies and the role of early re-imaging. BJU Int. 2019; 124(4):672–678.20. Lanchon C, Fiard G, Arnoux V, Descotes JL, Rambeaud JJ, Terrier N, et al. High grade blunt renal trauma: predictors of surgery and long-term outcomes of conservative management. a prospective single center study. J Urol. 2016; 195(1):106–111. PMID: 26254724.21. Voelzke BB, Leddy L. The epidemiology of renal trauma. Transl Androl Urol. 2014; 3(2):143–149. PMID: 26816762.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Nationwide Study on the Epidemiology of Head Trauma and the Utilization of Computed Tomography in Korea
- Epidemiology of Stroke in Korea
- Intervention for Urologic Trauma
- Treatment of Renal Injury: Practical Approach
- Absence of a Seasonal Variation of Hemorrhagic Fever with Renal Syndrome in Yeoncheon Compared to Nationwide Korea