Korean J Gastroenterol.
2022 Nov;80(5):221-224. 10.4166/kjg.2022.060.
Gastric Perforation Encountered during Duodenal Stent Insertion
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University of Korea, Eunpyeong St. Mary's Hospital, Seoul, Korea
- 2Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- KMID: 2536350
- DOI: http://doi.org/10.4166/kjg.2022.060
Abstract
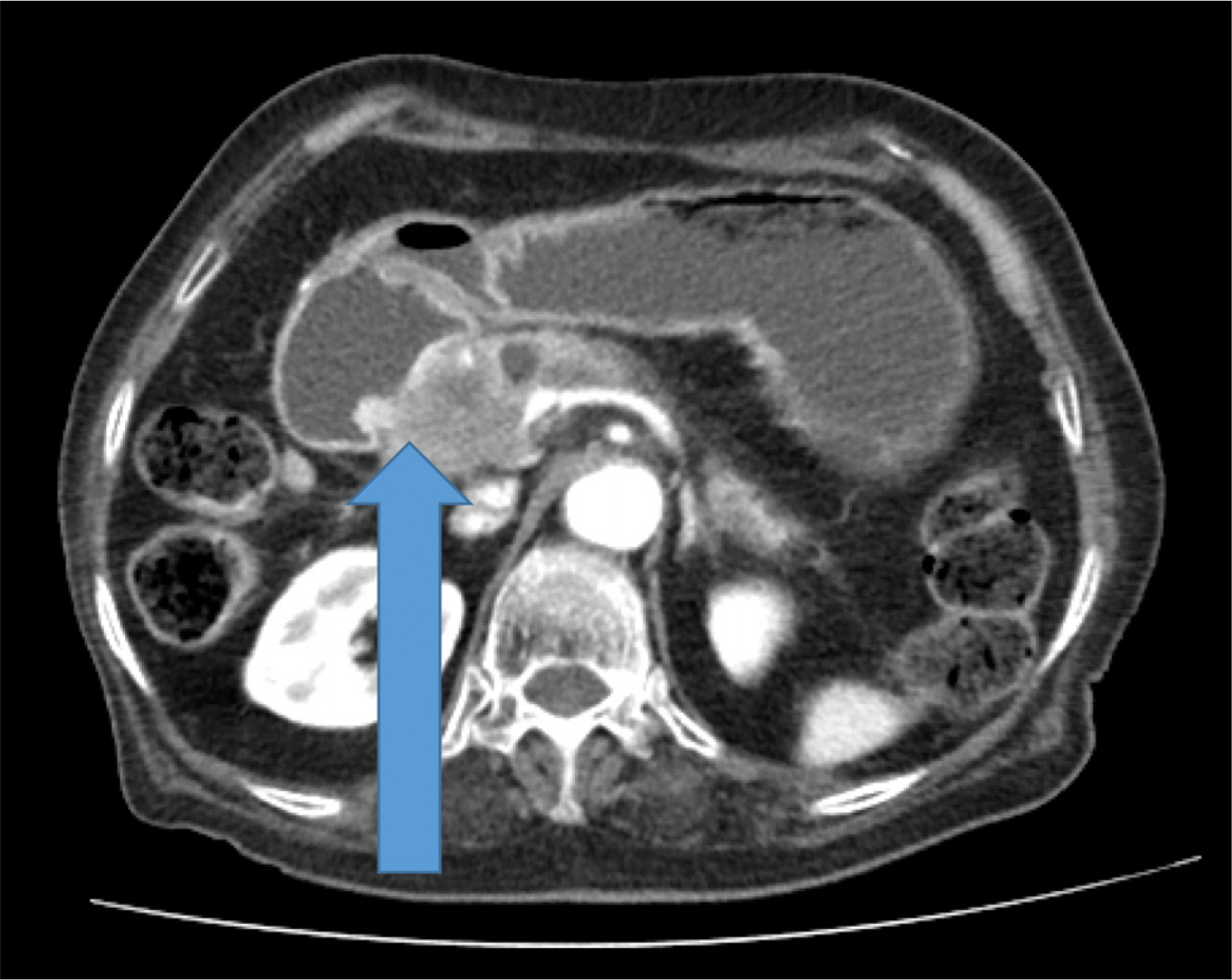
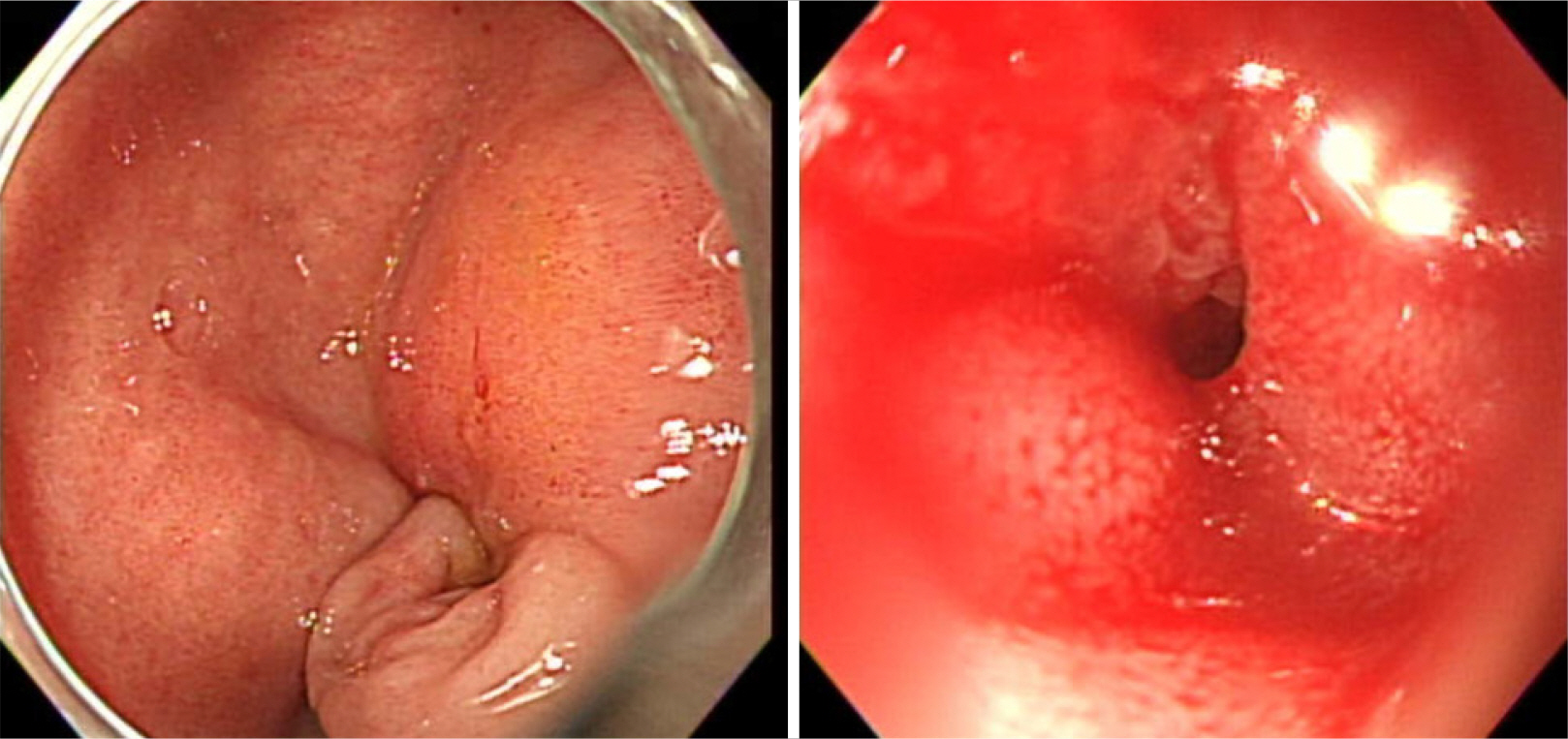
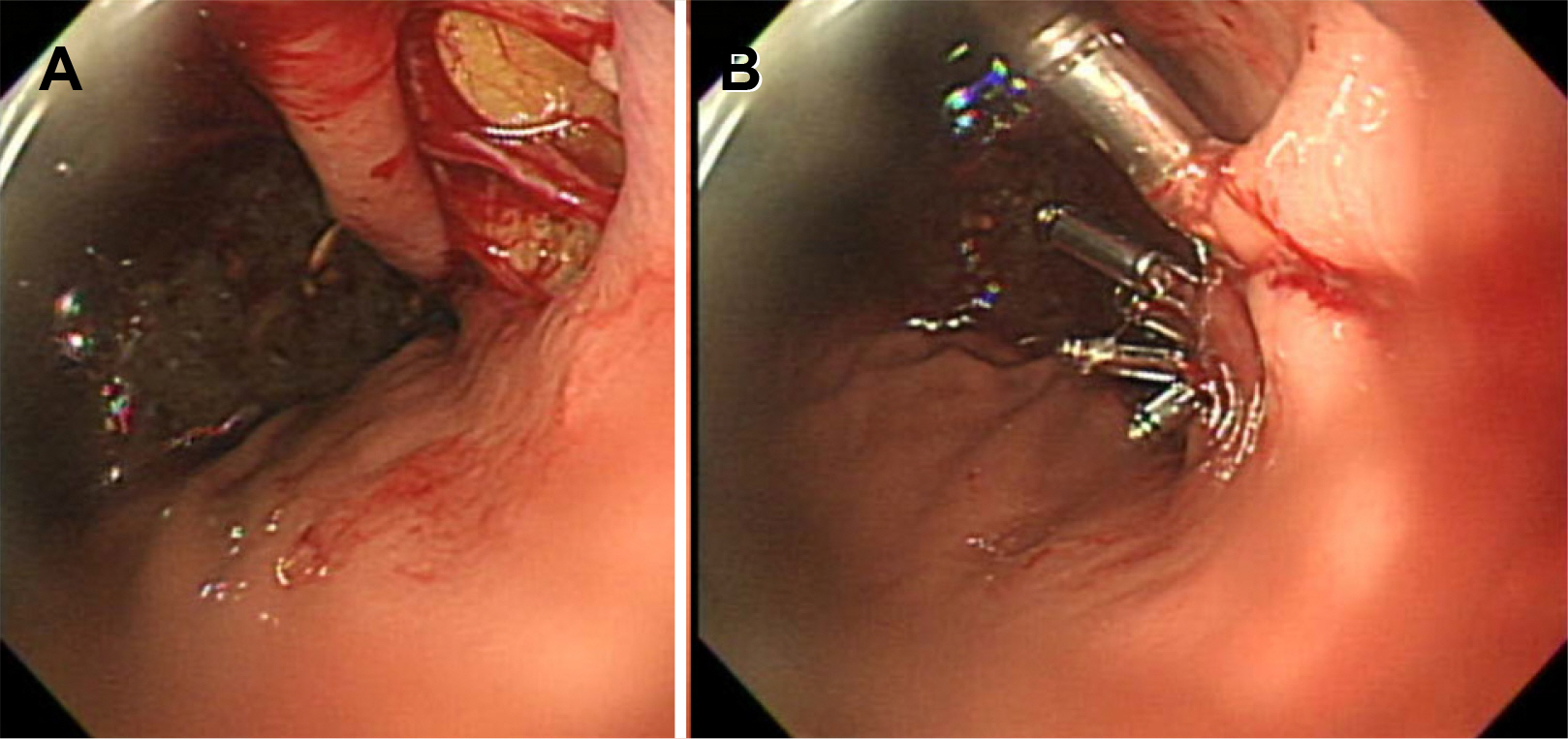
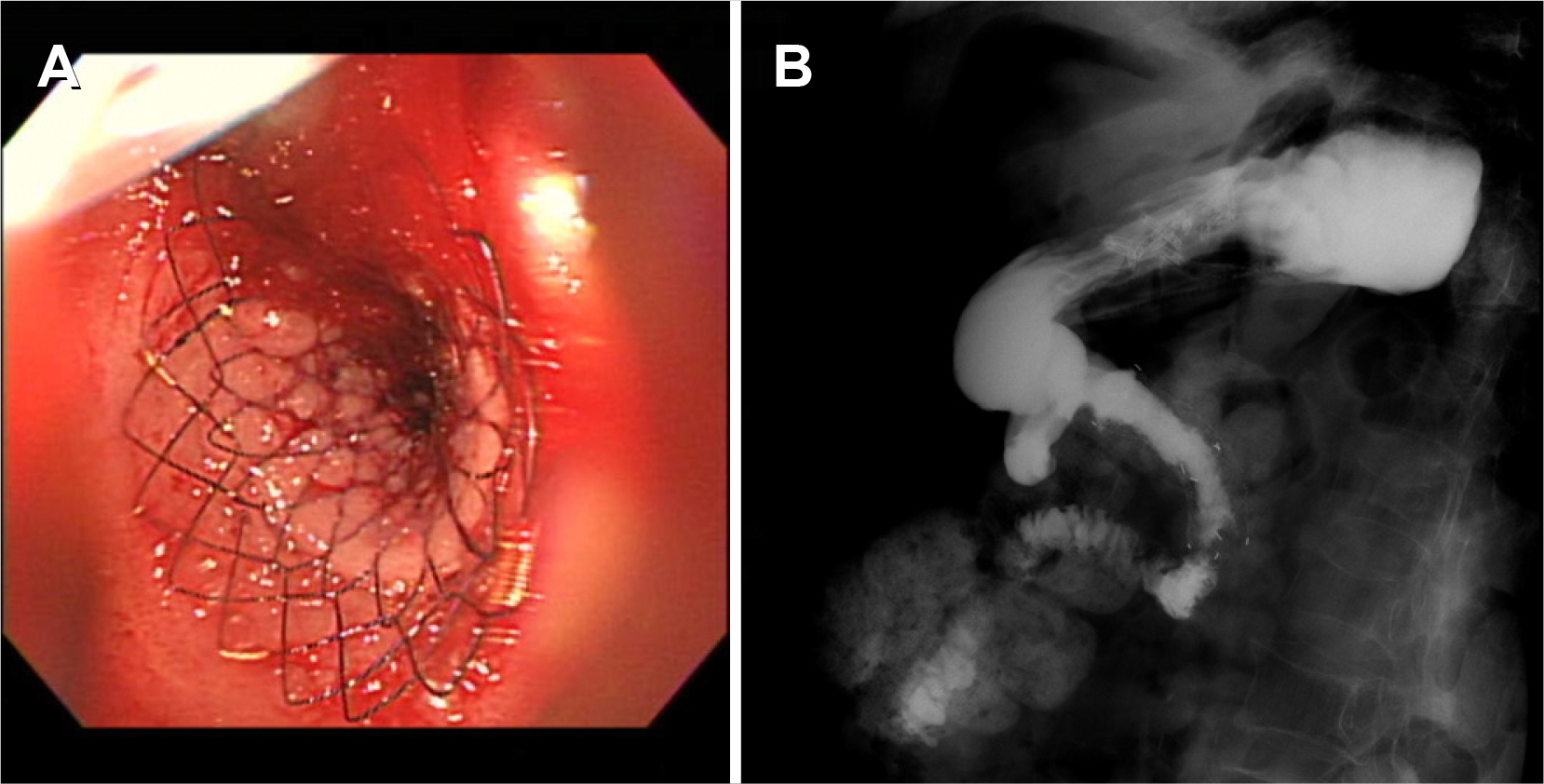
- Gastric outlet obstruction is a major symptom in patients with advanced pancreatic cancer. Endoscopic intervention is often challenging in severe strictures because the guidewire cannot pass beyond the stricture. Sometimes, the air itself cannot pass beyond the stricture, which can result in a severely distended stomach. Such a stomach is vulnerable to excessive air insertion or mechanical stress during endoscopic procedures, and endoscopists may encounter a higher rate of complications. Gastric perforation is rare but could be fatal. However, endoscopic management can show a favorable result if the perforation is noticed early. The authors report a case of the perforation of a gastric tear during duodenal stent insertion in a patient with a gastric outlet obstruction.
Keyword
Figure
Reference
-
1. Paspatis GA, Arvanitakis M, Dumonceau JM, et al. 2020; Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) position statement- update 2020. Endoscopy. 52:792–810. DOI: 10.1055/a-1222-3191. PMID: 32781470.
Article2. Kang DH, Ryu DG, Choi CW, et al. 2019; Clinical outcomes of iatrogenic upper gastrointestinal endoscopic perforation: a 10-year study. BMC Gastroenterol. 19:218. DOI: 10.1186/s12876-019-1139-1. PMID: 31842778. PMCID: PMC6916018.
Article3. Okada M, Ishimura N, Shimura S, et al. 2015; Circumferential distribution and location of Mallory-Weiss tears: recent trends. Endosc Int Open. 3:E418–E424. DOI: 10.1055/s-0034-1392367. PMID: 26528495. PMCID: PMC4612247.
Article4. Kim HS. 2015; Endoscopic management of Mallory-Weiss tearing. Clin Endosc. 48:102–105. DOI: 10.5946/ce.2015.48.2.102. PMID: 25844336. PMCID: PMC4381135.
Article5. Na S, Ahn JY, Jung KW, et al. 2017; Risk factors for an iatrogenic Mallory-Weiss tear requiring bleeding control during a screening upper endoscopy. Gastroenterol Res Pract. 2017:5454791. DOI: 10.1155/2017/5454791. PMID: 28348579. PMCID: PMC5350415.
Article6. Yamasaki T, Sakata Y, Suekane T, Nebiki H. 2021; Perforation of a gastric tear during esophageal endoscopic submucosal dissection under general anesthesia. Clin Endosc. 54:916–919. DOI: 10.5946/ce.2020.220. PMID: 33176411. PMCID: PMC8652158.
Article7. Chen W, Zhu XN, Wang J, Zhu LL, Gan T, Yang JL. 2019; Risk factors for Mallory-Weiss tear during endoscopic submucosal dissection of superficial esophageal neoplasms. World J Gastroenterol. 25:5174–5184. DOI: 10.3748/wjg.v25.i34.5174. PMID: 31558865. PMCID: PMC6747285.
Article8. Merchea A, Cullinane DC, Sawyer MD, et al. 2010; Esophagogastroduodenoscopy-associated gastrointestinal perforations: a single-center experience. Surgery. 148:876–882. DOI: 10.1016/j.surg.2010.07.010. PMID: 20708766.
Article9. Baron TH, Song LM, Ross A, Tokar JL, Irani S, Kozarek RA. 2012; Use of an over-the-scope clipping device: multicenter retrospective results of the first U.S. experience (with videos). Gastrointest Endosc. 76:202–208. DOI: 10.1016/j.gie.2012.03.250. PMID: 22726484.
Article10. Abidi WM, Thompson CC. 2016; Endoscopic closure of an iatrogenic perforation with an omental patch. Gastrointest Endosc. 83:652. DOI: 10.1016/j.gie.2015.09.004. PMID: 26386390.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Obstructive Jaundice after Insertion of Metallic Stent for Duodenal Obstruction by Recurrent Duodenal Ulcer
- A Case of Esophageal Perforation Cured by Conservative Management after Stent Insertion
- A Case of Afferent Loop Syndrome after Inserting a Double-Layered Pyloric Stent for Gastric Outlet Obstruction in a Patient with Stump Gastric Cancer after Undergoing Billroth II Radical Subtotal Gastrectomy
- Percutaneous transhepatic access to allow per-oral enteric stent insertion for malignant duodenal obstruction following failed endoscopic attempt
- Covered Self-expandable Metallic Stent Insertion as a Rescue Procedure for Postoperative Leakage after Primary Repair of Perforated Duodenal Ulcer