Neurointervention.
2022 Nov;17(3):168-173. 10.5469/neuroint.2022.00367.
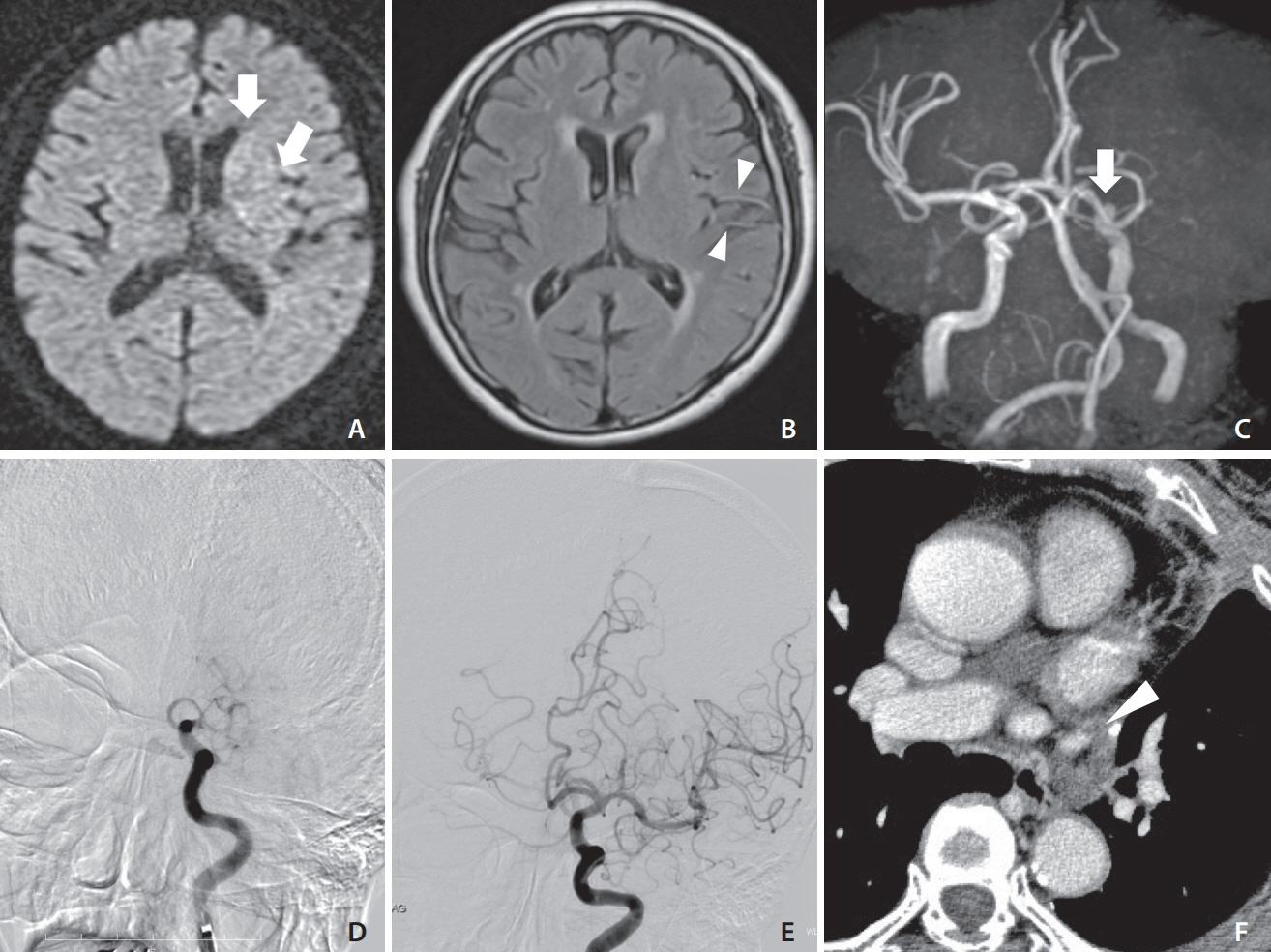
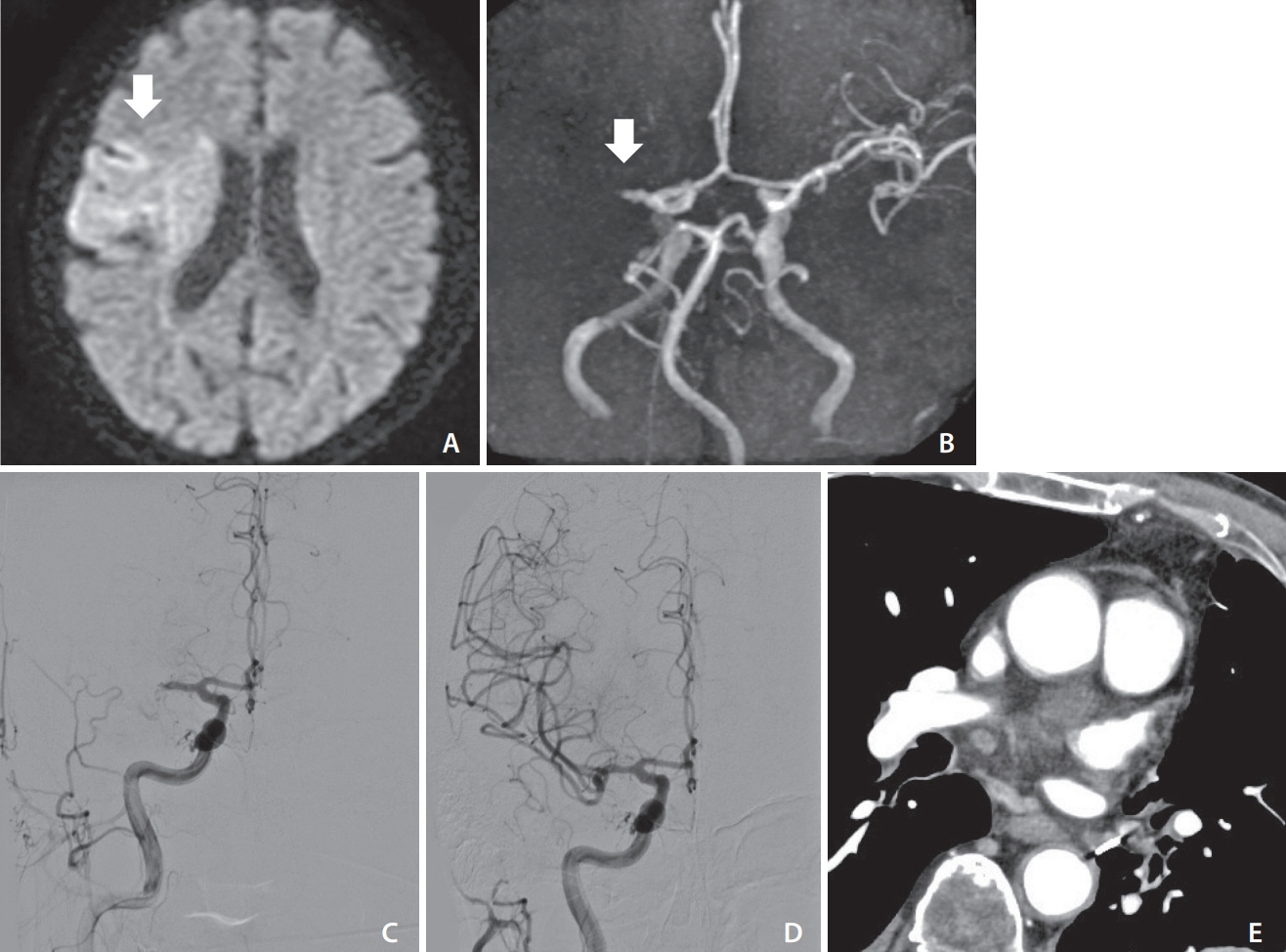
Mechanical Thrombectomy for Acute Ischemic Stroke due to Thrombus in the Pulmonary Vein Stump after Left Pulmonary Lobectomy: A Case Series
- Affiliations
-
- 1Department of Neurosurgery, Osaka Medical and Pharmaceutical University, Osaka, Japan
- 2Department of Neurosurgery, Kano General Hospital, Osaka, Japan
- KMID: 2535952
- DOI: http://doi.org/10.5469/neuroint.2022.00367
Abstract
- Cerebral embolic stroke caused by a thrombus in the pulmonary vein stump after left pulmonary lobectomy is a serious complication. We retrospectively analyzed four patients who underwent mechanical thrombectomy for large-vessel occlusion after left pulmonary lobectomy between January 2014 and March 2022. Two cases occurred after left upper lobectomy and the others occurred after left lower lobectomy. All patients presented with cerebral embolic stroke from the day after surgery to the 9th postoperative day, and successful reperfusion was achieved in all cases. Two patients had good outcomes at 90 days. Thrombus in the pulmonary vein stump is the probable cause of cerebral embolism, and mechanical thrombectomy is effective. Further studies are required to establish preventive measures and perioperative management strategies.
Figure
Reference
-
1. Yamamoto T, Suzuki H, Nagato K, Nakajima T, Iwata T, Yoshida S, et al. Is left upper lobectomy for lung cancer a risk factor for cerebral infarction? Surg Today. 2016; 46:780–784.
Article2. Kam PC, Calcroft RM. Peri-operative stroke in general surgical patients. Anaesthesia. 1997; 52:879–883.
Article3. Ikeda H, Yamana N, Murata Y, Saiki M. Thrombus removal by acute-phase endovascular reperfusion therapy to treat cerebral embolism caused by thrombus in the pulmonary vein stump after left upper pulmonary lobectomy: case report. NMC Case Rep J. 2014; 2:26–30.
Article4. Ohtaka K, Hida Y, Kaga K, Kato T, Muto J, Nakada-Kubota R, et al. Thrombosis in the pulmonary vein stump after left upper lobectomy as a possible cause of cerebral infarction. Ann Thorac Surg. 2013; 95:1924–1928.
Article5. Gual-Capllonch F, Teis A, Palomeras E. Pulmonary vein spontaneous echocontrast and stroke after pulmonary lobectomy. J Clin Ultrasound. 2013; 41:321–322.
Article6. Ohtaka K, Takahashi Y, Uemura S, Shoji Y, Hayama S, Ichimura T, et al. Blood stasis may cause thrombosis in the left superior pulmonary vein stump after left upper lobectomy. J Cardiothorac Surg. 2014; 9:159.
Article7. Xin Y, Hida Y, Kaga K, Iimura Y, Shiina N, Ohtaka K, et al. Left lobectomy might be a risk factor for atrial fibrillation following pulmonary lobectomy. Eur J Cardiothorac Surg. 2014; 45:247–250.
Article8. Nojiri T, Maeda H, Takeuchi Y, Funakoshi Y, Kimura T, Maekura R, et al. Predictive value of B-type natriuretic peptide for postoperative atrial fibrillation following pulmonary resection for lung cancer. Eur J Cardiothorac Surg. 2010; 37:787–791.
Article9. Ohtaka K, Hida Y, Kaga K, Takahashi Y, Kawase H, Hayama S, et al. Left upper lobectomy can be a risk factor for thrombosis in the pulmonary vein stump. J Cardiothorac Surg. 2014; 9:5.
Article10. Nakano T, Kaneda H, Kawaura T, Kitawaki T, Murakawa T. Ligating the pulmonary vein at the pericardial reflection is useful for preventing thrombus formation in the pulmonary vein stump after left upper lobectomy. Gen Thorac Cardiovasc Surg. 2019; 67:450–456.
Article11. Pillai JB, Barnard S. Cardiac tamponade: a rare complication after pulmonary lobectomy. Interact Cardiovasc Thorac Surg. 2003; 2:657–659.
Article12. Matsumoto K, Sato S, Okumura M, Niwa H, Hida Y, Kaga K, Committee for Patient Safety, Quality Management of Japanese Association for Chest Surgery, et al. Left upper lobectomy is a risk factor for cerebral infarction after pulmonary resection: a multicentre, retrospective, case-control study in Japan. Surg Today. 2020; 50:1383–1392.
Article13. Usui G, Matsumoto J, Hashimoto H, Katano T, Kusakabe M, Horiuchi H, et al. Thrombus reformation in the pulmonary vein stump confirmed 16 months after cerebral embolism on the day after left upper lobectomy for lung cancer. J Stroke Cerebrovasc Dis. 2018; 27:e225–e227.
Article14. Xie N, Meng X, Wu C, Lian Y, Wang C, Yu M, et al. Both left upper lobectomy and left pneumonectomy are risk factors for postoperative stroke. Sci Rep. 2019; 9:10432.
Article15. Morinaga Y, Nii K, Sakamoto K, Inoue R, Mitsutake T, Hanada H. Revascularization for in-hospital acute ischemic stroke after video-assisted thoracic surgery: report of 2 cases and literature review. World Neurosurg. 2019; 129:28–33.
Article16. Usui G, Takayama Y, Hashimoto H, Katano T, Yanagiya M, Kusakabe M, et al. Cerebral embolism caused by thrombus in the pulmonary vein stump after left lower lobectomy: a case report and literature review. Intern Med. 2019; 58:1349–1354.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Mechanical Thrombectomy for Large Vessel Occlusion via the Transbrachial Approach: Case Series
- Acute Ischemic Stroke Caused by Primary Pulmonary Adenocarcinoma with Extension to the Left Atrium
- Cerebral Embolism due to Thrombus in the Common Carotid Stump
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Pulmonary Infarction of Left Lower Lobe after Left Upper Lobe Lobectomy: 1 case report